Celia Morgan is a Professor of Psychopharmacology at the University of Exeter who has authored numerous publications on the potential therapeutic uses of ketamine in mental healthcare. In this episode, Celia dives deep into the neurobiology of ketamine, how it affects users, and how it differs from other, more classical psychedelics (LSD, MDMA, PCP, and psilocybin). She explains the potential promise of ketamine as a treatment for recalcitrant depression and addiction, and she details the results from her clinical trials in these areas. She discusses the importance of using ketamine in combination with psychotherapy to maximize its benefits, the potential risks associated with ketamine use, and advice for those interested in the therapeutic use of ketamine.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Celia’s training and interest in ketamine [2:15];
- The history of ketamine, medical uses, and use as a party drug [3:30];
- Neurobiology and pharmacology of ketamine [8:15];
- Ketamine regulation and abuse, and how it compares with psychedelics and other molecules [18:15];
- Ketamine as a therapeutic for depression [30:45];
- The brain under the influence of ketamine and theoretical mechanisms for its anti-depressive effects [48:00];
- Risks and concerns with overusing ketamine, and what an intermittent or maintenance dose might look for a patient [57:15];
- Treating addiction with ketamine: Celia’s studies of alcohol dependance [1:04:00];
- Advice for people considering the therapeutic use of ketamine [1:19:45]; and
- More.
Celia’s training and interest in ketamine [2:15]
Celia’s training
- Celia did her undergraduate in psychology with pharmacology and astrophysics
- She did a PhD program at University College London
- As part of that, she spent time at Yale on a scholarship to do some research in the US
- Her PhD was largely focused on the effects of ketamine
- She looked at the acute effects of ketamine as a model of psychosis
- At the time people were using ketamine with the idea that would help us understand the neuro-biological underpinnings of psychosis, because actually, from the outside, ketamine looks a little bit similar to people who are psychotic
- They were using that to map the kind of cognitive processes altered by ketamine
- Simultaneously, she was also looking at people who take ketamine recreationally
- At the time that was quite a big problem in the UK
- She looked at the acute effects of ketamine as a model of psychosis
- When she went to the US, it was to work on neuro-imaging studies looking at ketamine as a model for psychosis
- This was before it really became established as an antidepressant
The history of ketamine, medical uses, and use as a party drug [3:30]
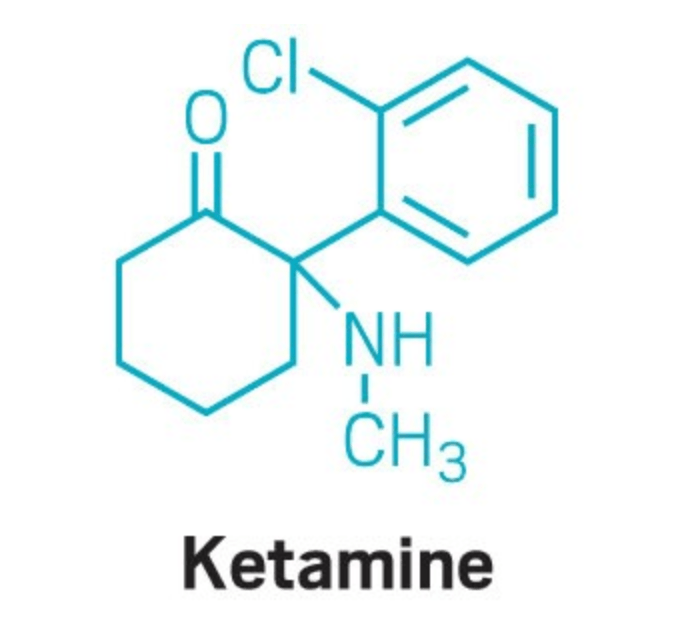
Figure 1. The chemical structure of ketamine. Image credit: c&en 2020
- Ketamine was synthesized in the ‘60s as an anesthetic to replace PCP (phencyclidine)
- People know PCP as angel dust
- There is a kind of folklore around it, of people running at the police and being shot down yet kept running.
- The problems with PCP is it had this protracted psychosis-like effects that lasted for a really long time following anesthesia
- It was still a good analgesic anesthetic
- Ketamine was synthesized as a similar molecule, so it still worked on the same receptor in the brain, the NMDA receptor, but it was 10 times less potent
- The drug company that synthesized it was initially really impressed by its analgesic and anesthetic effects, but then with increasing clinical experience, it was noticed that people were coming around from ketamine anesthesia reporting a variety of weird effects
- Things like hallucinations and out-of-body experiences
- And that’s what’s really limited its routine clinical use
- But it’s still one of the most widely used anesthetics in the world today
- It’s on the World Health Organization list of essential medicines
- One of the things Peter remembers from his clinical training is ketamine doesn’t produce respiratory depression
- This was a perk
- Most things used as anesthetic agents have this problem where if you overshoot them you can cause respiratory depression
- This is not an issue if you’re doing general anesthesia because you have an endotracheal tube in the main stem bronchus, so you’re breathing for the patient
- Otherwise though, respiratory depression is a frightening consequence that must be managed closely
- You don’t have to do this with ketamine
Is it true that kids are less susceptible to the hallucinogenic effects of ketamine?
- It is used more with children
- Celia tried to do a study on this, but it never really came off
- She doesn’t know if people have asked kids on ketamine if they have hallucinations
- Ketamine is widely used in pediatrics, geriatrics, and battlefield medicine
- It was the most widely used anesthetic in the Vietnam War
- It’s a really good question about kids
- Some people are trialing ketamine for antidepressant use in adolescents
The benefits of ketamine as an anesthetic
- It’s really safe, physiologically as an anesthetic, because it doesn’t slow your breathing or your heart rate
- So when you’ve lost a lot of blood, it’s good as well because it actually even vaguely increases your blood pressures
- That’s why it’s a widely used aesthetic
- Peter can understand why it became a turning point in the field medicine of Vietnam
- It’s the perfect anesthetic in trauma and shock where patients are hypovolemic, their blood pressure is going down
- Ketamine is an agent that acts slightly like a vasopressor, it raises blood pressure without the respiratory depression
- Celia adds, “The acute experience must be really unusual when you’re in that setting”
- The benefit of not having to intubate people made it really popular in developing countries where there is limited ability to intubate patients
- Ketamine is a really important medicine in anesthesia still, and Celia thinks that’s something people forget with all the new uses of ketamine
- It’s ridiculous to think that anesthesia is something we’ve only had vor about 140 years
- The concept of losing consciousness and how you measure it is fascinating
- We can measure on an EEG how your consciousness drops, but Celia doesn’t think we really know what turns it on and off
Is ketamine an analog of PCP?
- They’re all under the class of arylcyclohexylamines
- Edward Domino coined the term, dissociative anesthetics to describe PCP and ketamine
- People include nitrous oxide in that category
- This is based on the fact that they kind of disassociate you from your body and are characterized by these out-of-body experiences
- This can be quite helpful in anesthetic use
- They are related compounds; their main action is on the NMDA receptor
Neurobiology and pharmacology of ketamine [8:15]
A primer on how neurotransmitters work, how neurons can amplify or attenuate the response to them, and the action of ketamine on the NMDA receptor
- Glutamate is the major excitatory neurotransmitter in the brain and it’s prevalent all across the brain
- One of the receptors that glutamate works on is the NMDA receptor (N-methyl-D-aspartate receptor)
- The NMDA receptor is really important in a lot of our higher cognitive functions
- It plays a fundamental role in learning and memory
- Particularly in a process in learning called long term potentiation
- This is where brain cells that activate at the same time‒ if they both activate, then they’re more likely to activate in future
- This is characterized by this saying, “Neurons that fire together, wire together”
- Glutamate is really important in that and other excitatory functions in the brain
- GABA is an inhibitory neurotransmitter
- It shuts down the flow of electrical impulses across the brain
Peter’s summary: glutamate is excitatory and GABA is inhibitory
{end of show notes preview}

Celia Morgan, Ph.D.
Celia Morgan completed her undergraduate degree and Ph.D at the University College London (UCL). She then spent time at Yale University on a scholarship program before returning to UCL for postdoctoral research. Following this she worked at University of Melbourne as a visiting research fellow; then she returned to UCL for a fellowship and then Lectureship. She joined University of Exeter as a Senior Lecturer in May 2013 and was given a Chair in Psychopharmacology in 2015. She co-directs the Beckley/Exeter Cannabis Centre at the University of Exeter. She is also the Head of Ketamine Assisted Psychotherapy for Addiction at Awakn Life Sciences Corp. Additionally, she currently holds an Honorary Readership at UCL.
Dr. Morgan is interested in the effects of drugs and alcohol on the brain and behavior. Her research examines both the benefits and side effects of recreational drugs on cognition, mental health, and neurobiology. Through behavioral, neuroimaging studies, and clinical trials, she has investigated potential therapeutic uses of controlled substances. She uses a range of techniques from experience sampling and qualitative interviews to cognitive testing and functional and structural neuroimaging of the DTI and VBM. In particular, she has investigated treatment of addiction with a combination of psychological therapy and drugs such as ketamine and MDMA. [University of Exeter]




Please cover and emphasize the dangers here more. Ketamine, like other psychedelics, disrupts blood flow within the brain forcing the brain to form new pathways to orient sensory input; this is modern ‘lobotomy-like’ neuroplasticity. Please cover this issue in more depth, the medical exploration of these drugs is culturally endorsing recreational drug use. I am concerned that there is not enough harm reporting from these medical studies in order to drive more research, building more social support can and creating more recreational drug use. Thank you for your work Peter, I appreciate you.
Having suffered from depression (off and on) for two decades, I recently completed a 2 week, 6 dose (each IV infusion 2-3 days apart) ketamine treatment. The initial results have been extremely promising. I’m only two weeks out, but still feel a huge improvement in both my mood, anxiety and malaise. During the sessions, I was able to access (and feel) positive childhood memories that had completely disappeared. My brain feels like a fog has been lifted, and my ability to focus (zapped from years of depression/anxiety) has returned. I also have a renewed ability to genuinely laugh out loud, something that I’ve missed while on my most recent anti-depressant. Part of my treatment included the adoption of “new” habits while my brain was malleable from the ketamine — including healthier eating, daily walking, healthy relationships — which are designed to help sustain the positive affects. According to my doctor, I may need a booster (a one time infusion) at 4 weeks, or I may not need it for 6 months. Either way, this has been the most promising treatment I’ve experienced to date.
Ketamine is a miracle drug for me. I accidentally discovered its effect after surgery using Ketamine, and then sought treatment purposely for depression. I did not find that clinics were easy to qualify for, and I contacted four clinics (California and Washington) for treatment.
The expansion of Ketamine Clinics may be due to so many patients unable to improve their lives with standard treatment protocols, rather than a dodgy clinic practice.
Great discussion on Ketamine. While perhaps beyond the focus of this podcast I was disappointed that ketamine use for pain was not addressed. I encourage you to have someone on to talk about ketamine for pain. I actually see it used more for pain than depression.
RE: Dillion L comment above
I feel that firstly, the word “lobotomy“ is an incorrect word of choice to be used here as it is just full of bad mental health stigmatic connotations
Secondly, lobotomy permanently ended specific brain area functioning – Ketemine infusion is actually attempting to or is awakening previous atrophied areas of the brain. So, it’s not a disruption of the brain’s blood flow ( it’s more like re-wiring of the brain) making the brain form new pathways because of purposeful destruction and damage to particular areas the brain. I think you are off on your blood flow premise, as far off as you are speaking “ plumbing “ and I am speaking “ electricity “. Ketemine is in no way “lobotomy “ nor even like the lobotomy procedure or “lobotomy- like” using your words. Honestly, I cringed when I read your comment. As a Ketemine Infusion patient in midway ( 3 infusions to date) to find some relief from my lifelong MDD, I see as a “last hope” in so many ways and comparing it to the horribly stigmatic word “L” just does not seem necessary and may result in harm to us that are trying Ketemine infusion because it’s promising.
Peter, any comment on the recent surge of at home buccal/sublingual administration of Ketamine??