I wrote this post at about the same time Germany won the World Cup in Rio de Janeiro in 2014. There’s been a lot of moving and shaking in the world of exogenous ketones since then, not to mention soccer. Looking back on my post, I still consider it relevant in terms of what exogenous ketones possibly can (and cannot) do for performance. In this case, to see if exogenous ketone esters provide me a “boost” by allowing me to do the same amount of work while expending less energy (and work at a relatively lower VO2) compared to no supplementation.
I’m getting an increasing number of questions about exogenous ketones. Are they good? Do they work for performance? Is there a dose-response curve? If I’m fasting, can I consume them without “breaking” the fast? Am I in ketosis if my liver isn’t producing ketones, but my BOHB is 1.5 mmol/L after ingesting ketones? Can they “ramp-up” ketogenesis? Are they a “smart drug?” What happens if someone has high levels of both glucose and ketones? Are some products better than others? Salts vs esters? BHB vs AcAc? Can taking exogenous ketones reduce endogenous production on a ketogenic diet? What’s the difference between racemic mixtures, D-form, and L-form? What’s your experience with MCTs and C8?
Caveat emptor: the following post doesn’t come close to answering most of these questions. I only document my experience with BHB salts (and a non-commercial version at that), but say little to nothing about my experience with BHB esters or AcAc esters. But it will provide you will some context and understanding about what exogenous ketones are, and what they might do for athletic performance. We’ll likely podcast about the questions and topics above and cover other aspects of exogenous ketones in more detail.
—P.A., June 2018
§
Original publication date: August 14, 2014
Last year I wrote a couple of posts on the nuances and complexities of ketosis, with an emphasis on nutritional ketosis (but some discussion of other states of ketosis—starvation ketosis and diabetic ketoacidosis, or DKA). To understand this post, you’ll want to at least be familiar with the ideas in those posts, which can be found here and here.
In the second of these posts I discuss the Delta G implications of the body using ketones (specifically, beta-hydroxybutyrate, or BHB, and acetoacetate, or AcAc) for ATP generation, instead of glucose and free fatty acid (FFA). At the time I wrote that post I was particularly (read: personally) interested in the Delta G arbitrage. Stated simply, per unit of carbon, utilization of BHB offers more ATP for the same amount of oxygen consumption (as corollary, generation of the same amount of ATP requires less oxygen consumption, when compared to glucose or FFA).
I also concluded that post by discussing the possibility of testing this (theoretical) idea in a real person, with the help of exogenous (i.e., synthetic) ketones. I have seen this effect in (unpublished) data in world class athletes not on a ketogenic diet who have supplemented with exogenous ketones (more on that, below). Case after case showed a small, but significant increase in sub-threshold performance (as an example, efforts longer than about 4 minutes all-out).
So I decided to find out for myself if ketones could, indeed, offer up the same amount of usable energy with less oxygen consumption. Some housekeeping issues before getting into it.
- This is a self-experiment, not real “data”—“N of 1” stuff is suggestive, but it prevents the use of nifty little things likes error bars and p-values. Please don’t over interpret these results. My reason for sharing this is to spark a discussion and hope that a more systematic and rigorous approach can be undertaken.
- All of the data I’ll present below were from an experiment I did with the help of Dominic D’Agostino and Pat Jak (who did the indirect calorimetry) in the summer of 2013. (I wrote this up immediately, but I’ve only got around to blogging about it now.) Dom is, far and away, the most knowledgeable person on the topic of exogenous ketones. Others have been at it longer, but none have the vast experiences with all possible modalities (i.e., esters versus salts, BHB versus AcAc) and the concurrent understanding of how nutritional ketosis works. If people call me keto-man (some do, as silly as it sounds), they should call Dom keto-king.
- I have tried the following preparations of exogenous ketones: BHB monoester, AcAc di-ester, BHB mineral salt (BHB combined with Na+, K+, and Ca2+). I have consumed these at different concentrations and in combination with different mixing agents, including MCT oil, pure caprylic acid (C8), branch-chained amino acids, and lemon juice (to lower the pH). I won’t go into the details of each, though, for the sake of time.
- The ketone esters are, hands-down, the worst tasting compounds I have ever put in my body. The world’s worst scotch tastes like spring water compared to these things. The first time I tried 50 mL of BHB monoester, I failed to mix it with anything (Dom warned me, but I was too eager to try them to actually read his instructions). Strategic error. It tasted as I imagine jet fuel would taste. I thought I was going to go blind. I didn’t stop gagging for 10 minutes. (I did this before an early morning bike ride, and I was gagging so loudly in the kitchen that I woke up my wife, who was still sleeping in our bedroom.) The taste of the AcAc di-ester is at least masked by the fact that Dom was able to put it into capsules. But they are still categorically horrible. The salts are definitely better, but despite experimenting with them for months, I was unable to consistently ingest them without experiencing GI side-effects; often I was fine, but enough times I was not, which left me concluding that I still needed to work out the kinks. From my discussions with others using the BHB salts, it seems I have a particularly sensitive GI system.
The hypothesis we sought out to test
A keto-adapted subject (who may already benefit from some Delta G arbitrage) will, under fixed work load, require less oxygen when ingesting exogenous ketones than when not.
Posed as a question: At a given rate of mechanical work, would the addition of exogenous ketones reduce a subject’s oxygen consumption?
The “experiment”
- A keto-adapted subject (me) completed two 20-minute test rides at approximately 60% of VO2 max on a load generator (CompuTrainer); such a device allows one to “fix” the work requirement by fixing the power demand to pedal the bike
- This fixed load was chosen to be 180 watts which resulted in approximately 3 L/min of VO2—minute ventilation of oxygen (this was an aerobic effort at a power output of approximately 60% of functional threshold power, FTP, which also corresponded to a minute ventilation of approximately 60% of VO2 max)
- Test set #1—done under conditions of mild nutritional ketosis, while still fasted
- Test set #2—60 minutes following ingestion of 15.6 g BHB mineral salt to produce instant “artificial ketosis,” which took place immediately following Test set #1
- Measurements taken included whole blood glucose and BHB (every 5 minutes); VO2 and VCO2 (every 15 seconds); HR (continuous); RQ is calculated as the ratio of VO2 and VCO2. In the video of this post I explain what VO2, VCO2, and RQ tell us about energy expenditure and substrate use—very quickly, RQ typically varies between about 0.7 and 1.0—the closer RQ is to 0.7, the more fat is being oxidized; the reverse is true as RQ approaches 1.0
Results
Test set #1 (control—mild nutritional ketosis)
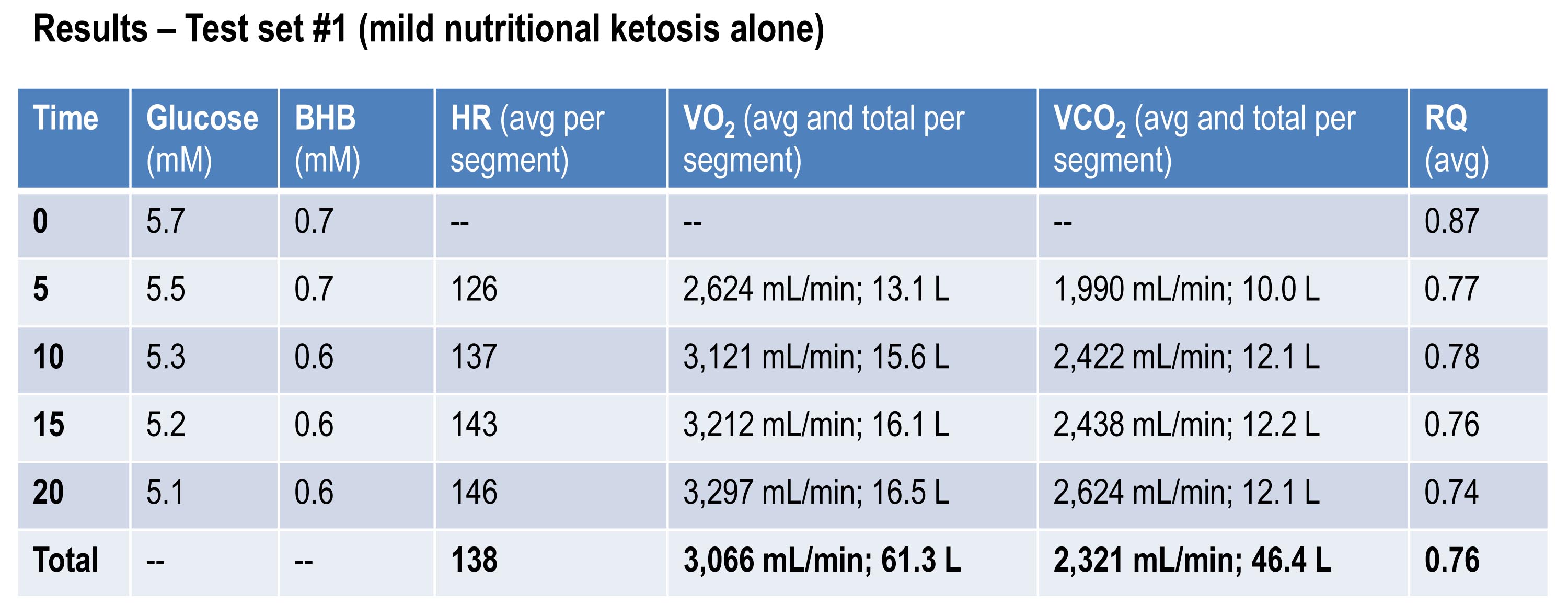
The table below shows the data collected over the first 20 minute effort. The 20 minute effort was continuous, but for the purpose of presenting the data, I’ve shown the segmental values—end of segment for glucose and BHB; segment average for HR, minute ventilation (in mL per min), and RQ; and segment total for minute ventilation (in liters).
Glucose and BHB went down slightly throughout the effort and RQ fell, implying a high rate of fat oxidation. We can calculate fat oxidation from these data. Energy expenditure (EE), in kcal/min, can be derived from the VO2 and VCO2 data and the Weir equation. For this effort, EE was 14.66 kcal/min; RQ gives us a good representation of how much of the energy used during the exercise bout was derived from FFA vs. glucose—in this case about 87% FFA and 13% glucose. So fat oxidation was approximately 12.7 kcal/min or 1.41 g/min. It’s worth pointing out that “traditional” sports physiology preaches that fat oxidation peaks in a well-trained athlete at about 1 g/min. Clearly this is context limited (i.e., only true, if true at all, in athletes on high carb diets with high RQ). I’ve done several tests on myself to see how high I could push fat oxidation rate. So far my max is about 1.6 g/min. This suggests to me that very elite athletes (which I am not) who are highly fat adapted could approach 2 g/min of fat oxidation. Jeff Volek has done testing on elites and by personal communication he has recorded levels at 1.81 g/min. A very close friend of mine is contemplating a run at the 24 hour world record (cycling). I think it’s likely we’ll be able to get him to 2 g/min of fat oxidation on the correct diet.
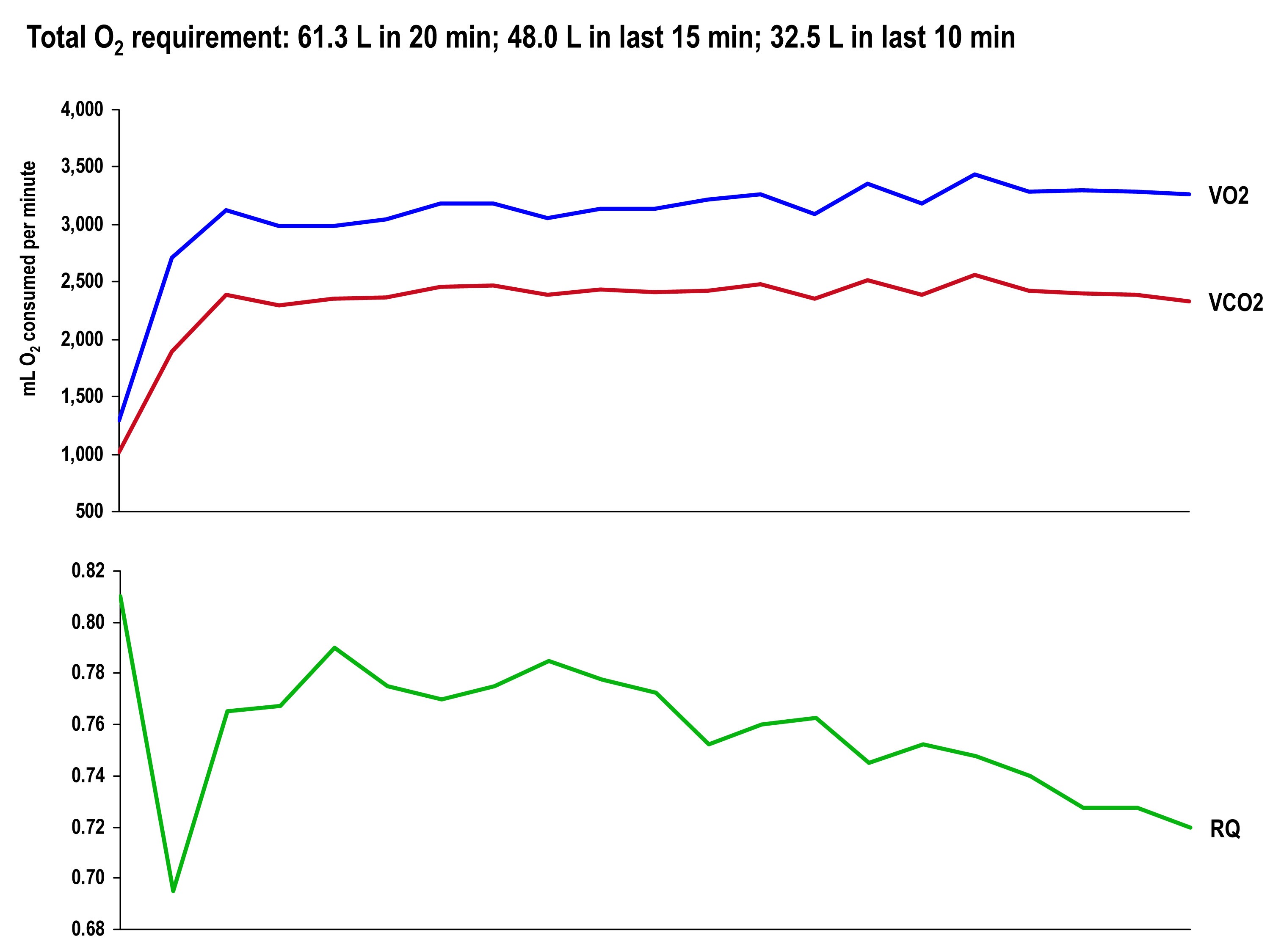
The graph, below, shows the continuous data for VO2, VCO2 (measured), and RQ (calculated).
Test set #2 (ingestion of 15.6 g BHB salt 60 minutes prior)
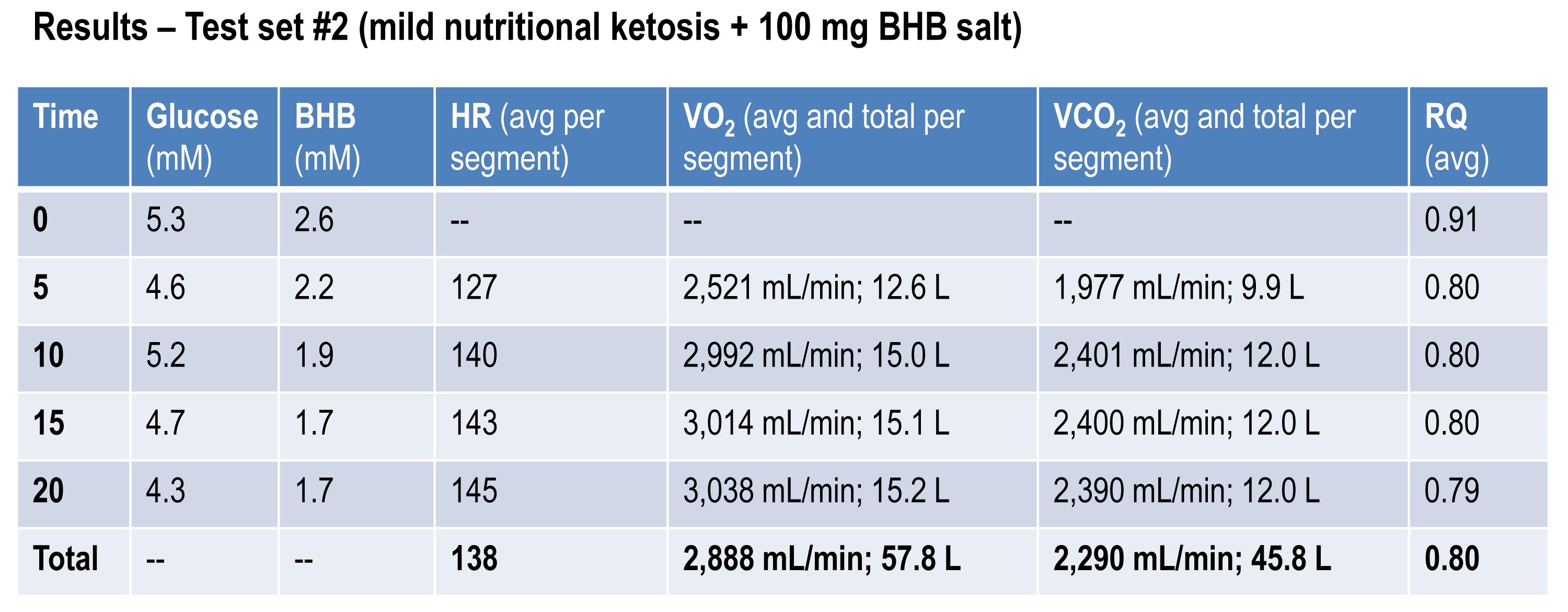
The table below shows the same measurements and calculations as the above table, but under the test conditions. You’ll note that BHB is higher at the start and falls more rapidly, as does glucose (for reasons I’ll explain below). HR data are almost identical to the control test, but VO2 and VCO2 are both lower. RQ, however, is slightly higher, implying that the reduction in oxygen consumption was greater than the reduction in carbon dioxide production.
If you do the same calculations as I did above for estimating fat oxidation, you’ll see that EE in this case was approximately 13.92 kcal/min, while fat oxidation was only 67% of this, or 9.28 kcal/min, or 1.03 g/min. So, for this second effort (the test set) my body did about 5% less mechanical work, while oxidizing about 25% less of my own fat. The majority of this difference, I assume, is from the utilization of the exogenous BHB, and not glucose (again, I will address below what I think is happening with glucose levels).
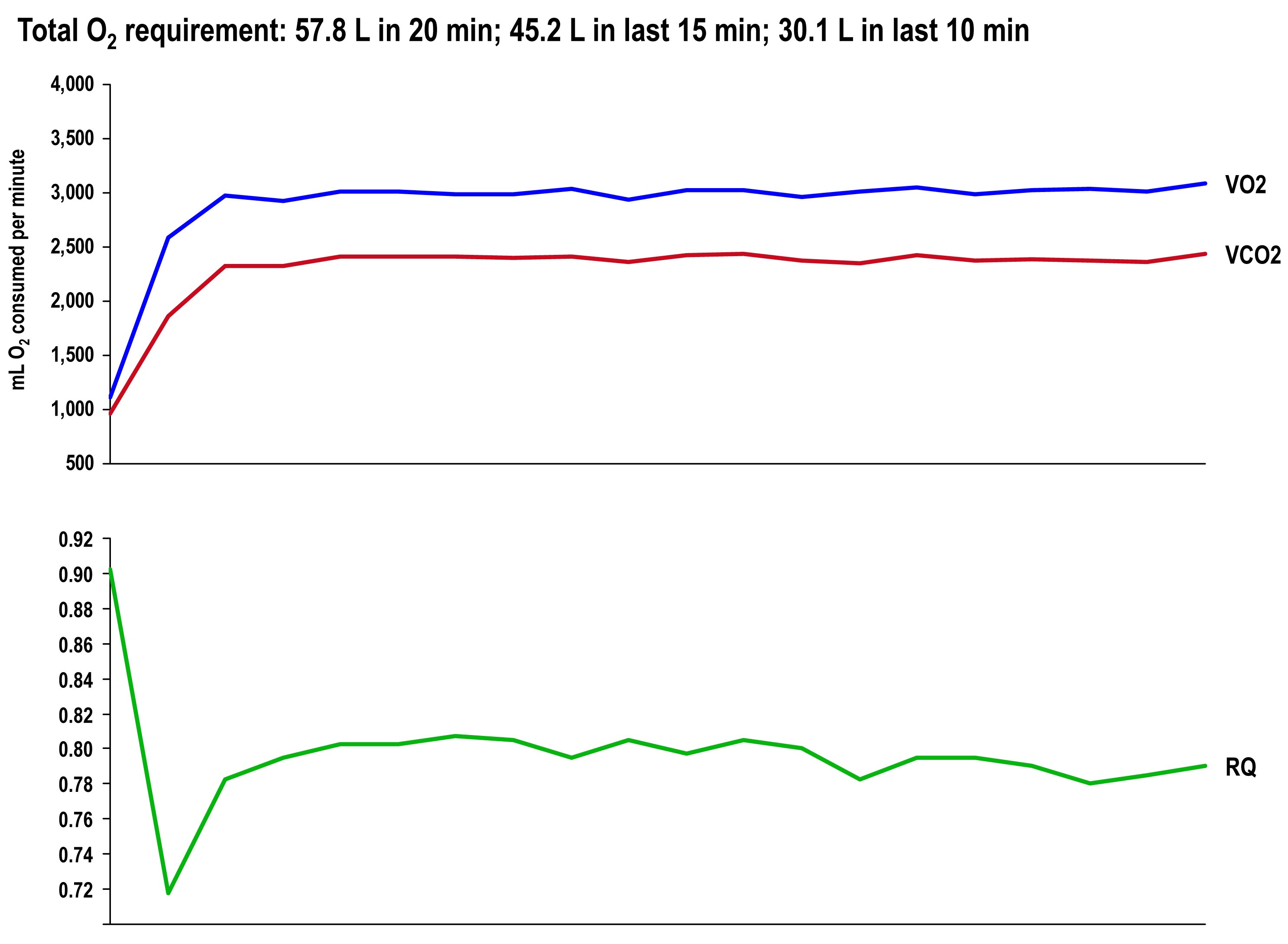
The graph once again shows the continuous data for VO2, VCO2 (measured), and RQ (calculated).
Side-by-side difference
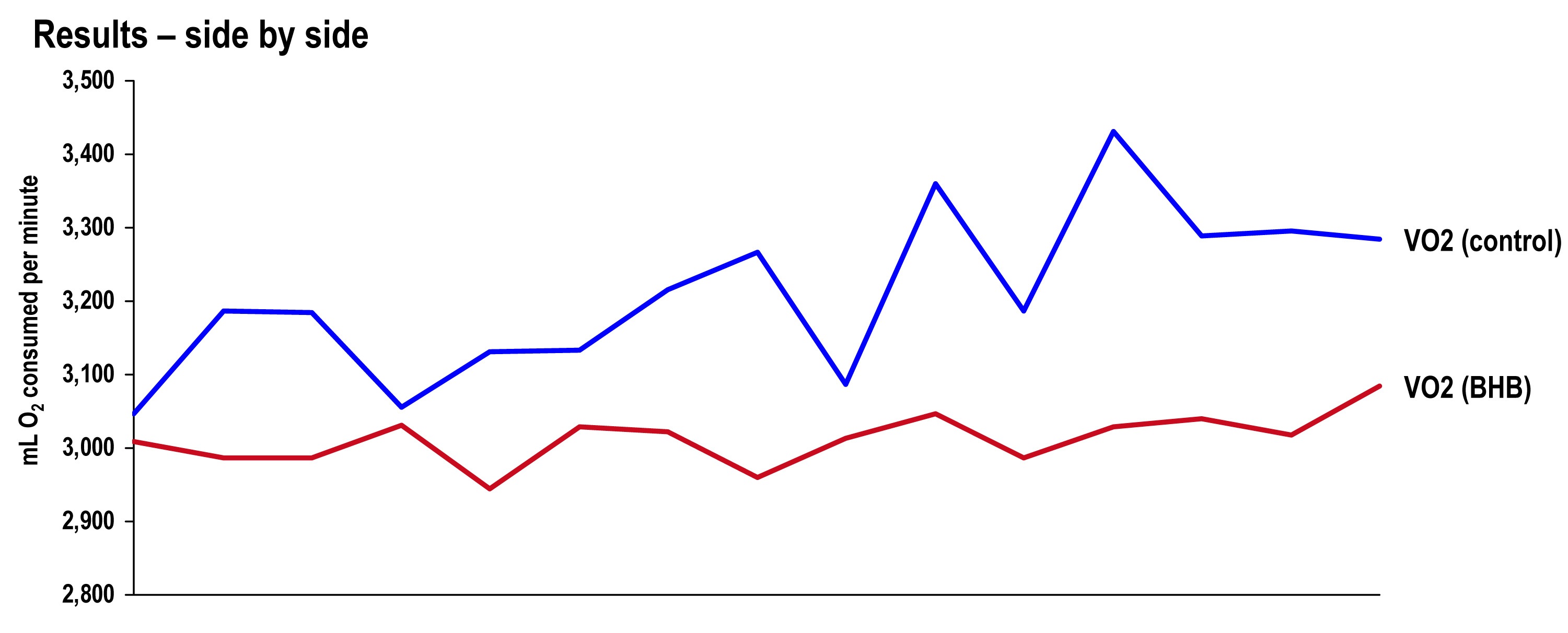
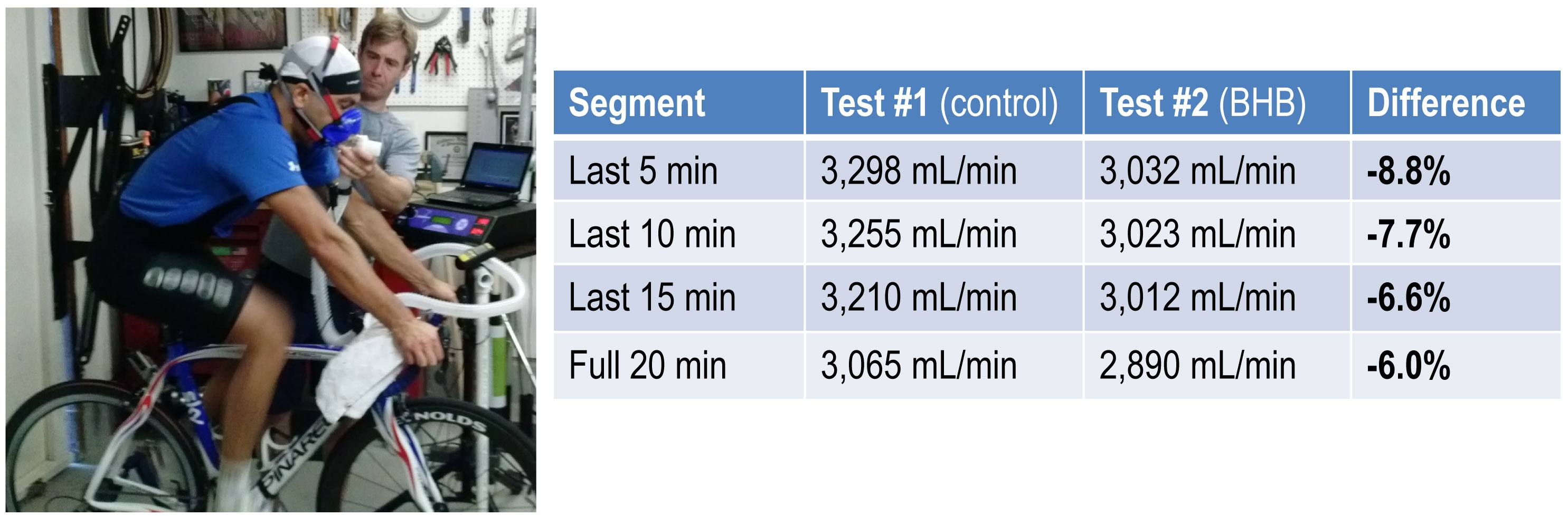
The final graph, below, shows the continuous data for only VO2 side-by-side for the 20 minute period. The upper (blue) line represents oxygen consumption under control conditions, while the lower line (red) represents oxygen consumption following the BHB ingestion. In theory, given that the same load was being overcome, and the same amount of mechanical work was being done, these lines should be identical.
The hypothesis being tested in this “experiment” is that they would not be the same. Beyond visual inspection, the difference between the lines appears to grow as the test goes on, which is captured in the tabular data showing 5 minute segmental data.
Limitations
The most obvious limitation of this endeavor is the fact that it’s not an appropriately controlled experiment. Putting that aside, I want to focus on the nuanced limitations—which don’t impact the primary outcome of oxygen consumption—even if one were appropriately doing a real experiment.
- It’s not clear that the Weir coefficients used to estimate EE are relevant for someone in ketosis, let alone someone ingesting exogenous BHB. (The Weir formula states that EE is approximated by 3.94 * VO2 + 1.11 * VCO2, where VO2 and VCO2 are measured in L/min; 3.94 and 1.11 are the Weir coefficients, and they are derived by tabulating the stoichiometry of lipid synthesis and oxidation of fat and glucose and calculating the amount of oxygen consumed and carbon dioxide generated.) While this doesn’t impact the main observation—less oxygen was consumed with higher ketones—it does impact the estimation of EE and substrate use.
- In addition to the Weir coefficients being potentially off (which impacts EE), the RQ interpretation may be incorrect in the presence of endogenous or exogenous ketones. As a result, the estimation of fat and glucose oxidation may be off (though it’s directionally correct). That said, the current interpretation seems quite plausible—greater fat oxidation when I had to make my ketones; less when I got my ketones for “free.”
Observations from this “experiment” (and my experience, in general)
Animal models (e.g., using rat hearts) and unpublished case reports in elite athletes suggest supplemented BHB produces more ATP per unit carbon and per unit oxygen consumed than glycogen and FFA. This appears to have been the case in my anecdotal exercise.
The energy necessary to perform the mechanical work did not appear to change much between tests, though the amount of oxygen utilization and fat oxidation did go down measurably. The latter finding is not surprising since the body was not sitting on an abundant and available source of BHB—there was less need to make BHB “the old fashioned way.”
As seen in this exercise, glucose tends to fall quite precipitously following exogenous ketone ingestions. Without exception, every time I ingested these compounds (which I’ve probably done a total of 25 to 30 times), my glucose would fall, sometimes as low as 3 mM (just below 60 mg/dL). Despite this, I never felt symptomatic from hypoglycemia. Richard Veech (NIH) one of the pioneers of exogenous ketones, has suggested this phenomenon is the result of the ketones activating pyruvate dehydogenase (PDH), which enhances insulin-mediated glucose uptake. (At some point I will also write a post on Alzheimer’s disease, which almost always involves sluggish PDH activity —in animal models acute bolus of insulin transiently improves symptoms and administration of exogenous ketones does the same, even without glucose.)
In addition, the body regulates ketone production via ketonuria (peeing out excess ketones) and ketone-induced insulin release, which shuts off hepatic ketogenesis (the liver making more ketones when you have enough). The insulin from this process could be increasing glucose disposal which, when coupled with PDH activation, could drive glucose levels quite low.
If that explains the hypoglycemia, it would seem the absence of symptoms can be explained by the work of George Cahill (back in the day; see bottom figure in this post)—when ketone levels are high enough they can dominate brain fuel, even ahead of glucose.
Finally, these compounds seemed to have a profound impact on my appetite (they produced a strong tendency towards appetite suppression). I think there are at least two good explanations for this, which I plan to write about in a dedicated post. This particular topic—appetite regulation—is too interesting to warrant anything less.
Open questions to be tested in real experiments
- Are these results reproducible? If so, how variable are the results across individuals (by baseline metabolic state, diet, fitness)?
- Would the difference in oxygen consumption be larger (or smaller) in an athlete not already keto-adapted (i.e., not producing endogenous ketones)?
- Would the observed effect be greater at higher plasma levels of BHB (e.g., 5 to 7 mM), which is “easily” achievable with exogenous ketones?
- Would the observed effect be the same or different at higher levels of ATP demand (e.g., at FTP or at 85-95% of VO2 max)?
- Would the trend towards improved energy efficiency continue if the exercise bout was longer in duration (say, greater than 2 hours)?
- How will exogenous ketones impact exercise duration and lactate buffering?
- Why do exogenous ketones (both BHB and AcAc it seems) reduce blood glucose levels so much, and can this feature be exploited to treat type 2 diabetes?
- Are there deleterious effects from using exogenous ketones, besides GI side-effects?
- What are the differences between exogenous BHB and AcAc (which in vivo exist in a reversible equilibrium) on this particular phenomenon? (Work by Dom D’Agostino’s group and others have shown other differences in metabolic response and clinical application, including their relative impact on neurons.)
Photo by Alexey Lin on Unsplash







Got my September issue of Wired in the mail yesterday. Great article Peter.
Thanks, Dan. My daughter asked why she couldn’t be in it holding a spoon.
The beard looks good, too.
Totally OT, but I read your old post on Do calories matter? (Feb-March 2012):
You seem to have got it backwards when you speak of breaking [chemical] bonds as a way of “releasing energy”.
Its the other way around: Bonds are “valleys”; you need [external] energy to get out of them. You release energy when bonds are formed (“electrons rolling into valleys”).
Otherwise a very interesting site?
Otherwise, a very interesting site!
Exclamation, not question!
Hi Peter, fascinating stuff and considering buying KetoForce exogenous BHBO product. In your knowledge, has there been any research on the effectiveness of exogenous ketones when combined with elevated insulin? Obviously ketones wouldn’t be produced by the liver under these conditions, but is there any research proving how exogenous ketones might act in these situations?
Cheers
Not sure.
With the wealth of knowledge you are accumulating, Dr. Attia, I think you should do a startup on customized nutrition plans :-). People will send their Lipid profile history and details (you could even hookup with 23andme) and you and your team create a custom nutrition plan. You could even do enterprise pricing 🙂 .
I am spending too much time on your website :-/
Hi Peter,
I was trying to find some information on your site with regard to flow-mediated dilation of the brachial artery. I was reading several journal articles on ketogenic diets and came across this meta-analysis:
https://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=8976486&fileId=S000711451300216X
It sounds like the low-carb diets results in greater cardiovascular risk when using the FMD but it’s unclear to me why this might be and whether this would hold true if I tried to maintain ketosis through soy, fish, eggs, and nuts but no land or air animals. Any thoughts or can you point me to good follow-up reading?
It’s unclear to me if this artificial test of the radial artery has any clinical significance.
I find your blog really interesting and was considering making a PDF with all its entries so that I can read it more easily. There’s something else I want to do with that PDF that might be problematic: I have several medicine students among my friends and I was considering printing and distributing it among them to try and make them understand that there might be one or two things wrong about the approach their professors take. So, is the content of this blog available for public reproduction and distribution?
Thanks a lot for your knowledge and for sharing it with us!
Sure, if you reference it appropriately, please pass around as you see fit.
Peter,
First, thanks for sharing so much.
Second, over the last several months I have been suggesting a low carb diet to patients (mainly to help reduce cavity risk). It would be advantageous to have resources to suggest to them. Currently, I give them (or suggest they buy) Volek/Phinney’s Low Carb Living book. Any other suggestions?
Third, as products come into the market in the supplement world. Do you have a suggestion on how we can determine the quality and contents of any products? The concern, obviously, being the stated ingredients are only partly true/accurate.
Finally, excited to see what NUSI does in the nutrition world.
keep it up!
Cheers,
Jason
I don’t really follow the books in the space. I don’t know the answer to your last question. Because I know a very good compounding pharmacist, I run any supplement I try by him first. I think there are folks out there trying to put info together on supplements, more broadly.
Wow, your fat oxidation rate of 1.2g/min still is pretty darn high, given that the average person is about 0.5g/min, and even professional (high carb?) racers are around 1g/min. What range of numbers do Pat and Dominick see in their clients? (Do they see the “standard” < 1.2g/min for high-carb athletes?)
So having a 0.5g/min FOR advantage will provide you with 270 kCal/hr additional fuel "without eating". Pretty interesting. Thanks for sharing your data.
BTW, there's a scatter plot of VO2max vs. FOR, showing a fairly linear correlation, over data points including untrained subjects as well as professional cyclists:
https://www.pponline.co.uk/encyc/fat-burning-using-body-fat-instead-of-carbohydrates-as-fuel-40844
I can’t speak for them, but Pat has tested me at much higher levels when we push through to VO2 max. Jeff Volek has seen the gamit of fatOx rates. LIke I said in the post, I think there are folks out there who can get to 2 g/min, though I doubt I can get above 1.7 g/min.
I have followed a ketogenic diet on and off for a few years. As a long distance runner, I do find that the ketone adapted state yields greater muscular endurance (my own experience) and helped me with a marathon I ran in the Himalayas. I placed 2nd out of the females who were foreign (I train at sea level) and 6th out of all females.
I have recently learned, however, that my son has a disorder of ketone metabolism. We have followed low carb style eating for years and my son has truly struggled. After a great deal of testing leading absolutely no where, we finally decided that he has an IEM and had arrangements with the local hospital to do the right tests during an episode (encephalopathy, vomiting, etc). What we learned is that he produces very high levels of BHB and AcAc and was experiencing metabolic acidosis with a high anion gap. He also produced respiratory chain metabolites in his urine. The doctors have narrowed it down to Beta keto thialase deficiency, SCOT deficiency, or SCADD. So far the tests are inconclusive. For BKT and SCOT, they are enzymes needed to break ketones down into usable form in order to go through the citric acid cycle. I am not a biochemist so I might be wrong about the details. (Economist here!)
Thanks to my years of keto-running, I now test my son for BHB and blood glucose and use the keto sticks to test the AcAc. We are now catching the episodes earlier because we know what to look for and can test for it easily. While he continues to have episode of keto/metabolic acidosis, they are less severe than his first episode.
In the intervening months, I have begun studying the different energy pathways to try and understand what is happening to my son. I am curious about your perspective on these abnormal metabolic issues and ways to work around them.
Thank you so much for all your research. I have thoroughly enjoyed reading your blog for years.
Have you tested your son’s VO2Max? In metabolic disorders where the aerobic capacity is not limited by oxygen, but by efficiency of the electron transport chain, a low VO2Max might help you to very cheaply quantify how well his mitochondria are working.
I have some extreme mitochondrial injury, which has taken me the better part of 14 months to chase down. It was not until I did VO2Max, and objectively quantified that I had changed from endurance trained to aerobic metabolism that was worst data point in a 200-person study, that I realized the extent of the injury. VO2Max might help you to add another data point to your son’s condition to help characterize it.
Hi Peter, this is probably well off topic, but I am interested in your view. A friend, who is a type 1 diabetic, and I have been following a ketogenic diet for a few years now. We both do trail running and have seen big improvements in our performance. Incidentally, his insulin consumption has dropped from around 25 units per day to around 5. In the past, when he has mismanaged his insulin or sugar intake, and become hypoglycemic, he has become disorientated and, sometimes, almost semi conscious. More recently when he has stopped and tested his blood sugar during a run, he has discovered it to be extremely low, for instance 1,4 mmol/L and yet he is quite focused and calmly consumes some sugar to bring it back up. I am sure that, before he was on a ketogenic diet, he would have been incoherent at this blood sugar level. Is it possible that, since his brain is being fuelled by ketones, it is less susceptible to hypoglycemia? This may be of great benefit to type 1 diabetics if true.
I think that is exactly what is going on.
Along this line, I’ve wondered about the effects of the insulin production caused by proteins as per the Insulin Index (II). If one is on a ketogenic diet, one is, and is aiming for around 20 grams a day of CHO, one should already have low blood sugar. Then, if one were to eat beef or whey one would get a dose of insulin without the signal of rising blood sugar, since beef or whey do not raise the blood sugar but cause insulin secretion anywhey. Golly, I thought, wouldn’t that cause hypoglycemia big time by pushing down an already very low blood sugar, a dietary situation I’m likely to be in several times a day. I’m goofy by nature, so the disorientation symptom of hypoglycemia might not be so noticeable, still, I don’t think I’d miss it entirely if it were happening that often. So the idea of keytones feeding the brain, and most tissues, would explain the absence of hypoglycemia on a ketogenic diet when high II foods generate insulin production into a low blood sugar situation. Or am I missing something?
Rewrite of penultimate sentence: So the idea of keytones feeding the brain, and most tissues, would explain the absence of hypoglycemia [symtoms] on a ketogenic diet when high II [proteins] generate insulin production into a low blood sugar situation. Or am I missing something?
Robb Wolf describes an experience of imitating a paleo-era hunt, which was physically taxing. He was mildly keto-adapted when doing it. Afterward, his blood glucose was measured and it was incredibly low – IIRC, somewhere in the 40 mg/dL range – but he was fine. The belief is that his brain was using ketones.
I’ve been in ketosis for about a month now and I test my blood ketone levels first thing in the AM. Today’s reading was 3.4 mM…is that too high? I’ve read all the books and they mention that 3.5 mM is the upper end of a therapeutic level and above 3.5 is known as “starvation ketosis”. I’m going to adjust my protein from 70 grams to 90 grams and see what happens. Any insight would be appreciated.
Hi Mark,
If it helps, I’ve had BHB levels of over 5.0mM/l without any ill effects at all. Acidosis happens at considerably higher levels than that (I faintly recall seeing a threshold in the double figures being quoted somewhere but please do check if you want to know for sure). In a healthy and non-diabetic person ketone body production will be down-regulated well before such levels are reached.
Best regards,
Mike
Hi Peter,
might I know your opinion on whether ketosis affects in any way a bone fracture healing? I read somewhere that acidic environment is not ideal for bone healing.
Thanks a lot.
Jan
PS: wonderful web of yours, thanks for it.
I had two relatively straight forward questions that should be mildly interesting-
1. For some unknown reason, I have started to think that artificial sweeteners are at least the smallest bit responsible for insulin insensitivity. That is, perhaps the taste of “sweet” is *somehow* relayed from the tongue to brain/intestines(just guessing here?) to the pancreas, causing insulin to be released. Of course, the taste is artificial and there is no sugar and therefore, the body starts to ignore changes in insulin levels independent of blood sugar.
Of course, I could totally be wrong about this. Any thoughts?
2. If someone on the ketogenic diet strictly limits their sugars, and bacteria in the mouth prefer digesting sugars (I am not sure of this assumption), then wouldn’t the ketogenic diet support teeth/gum health?
Thanks!
@Drew M
I don’t know about question #1, but the answer to question #2 is a resounding YES! I used to have gingivitis, but since going low carb, and eventually to nutritional ketosis, my gums have healed up and I never wake up with “fuzzy teeth” anymore. No more cavities either. This appears to be a common and pleasant surprise bonus to folks who reduce their carb consumption for other reasons, such as weight loss or diabetes management.
Keep on smiling!
Hi Peter,
Great post and great self-experiment. It looks like you’re done a couple of posts now regarding exercise/energy and ketosis. I was wondering if you know of any good resources about the effect of nutritional ketosis on muscle growth (or atrophy). I’ve found some literature online but it’s a bit lacking in the science department.
Jeff Volek and Lyle McDonald are worth reading on this topic.
Re insulin index, look at Mark’s comments:
https://www.marksdailyapple.com/insulin-index/#ixzz3CVHlkE2O
Peter,
Three weeks on high fat, low carb average less than 50g Carbs, 110g protein and > 200g fat per day.
NMR lipoprofile
LDL-p 1470
LDL-C 115
HDL-C 58
TG 66
Chol. total 186
HDL-p 36.4
Small LDL–P 672
LP-IR score 46
46 year old male. 6 foot, 195 pounds. Weigth lifting. Family history unknown-adopted
Any interpretation greatly appreciated. Thanks for all your insights and work!
Mike
Hi Peter!
I just came across this link and reminded me of your comments about how different types (like your wife and you) react differently to carbs. Thought you might want to check it out:
https://www.precisionnutrition.com/carbohydrate-tolerance-genes
Mario, I checked out the site you referenced and I noticed it does not entertain comments. This site looks like a “for profit” site. Personally, I don’t trust sites which do not accept commentary. Commentary keeps you honest and credible. I learn a lot from comments. So my impression of what this site presents is biased from the start. For me, a no-biochemistry engineer, the content may be correct, but I would not give it much credibity.
Hi Peter,
Thanks for investing the time to write a very interesting post again. What is the possible explanation for the resting state’s RQ to be higher then in the workout. I was sure that the higher the intensity the higher the RQ. Specifically in the control test.
Avner
O2 consumption goes down more than CO2 production does.
then=than
https://www.amazon.com/Fed-Up-Katie-Couric/dp/B00L5R5GE2/ref=sr_1_1?ie=UTF8&qid=1409336102&sr=8-1&keywords=fed+up
DENNIS BANKS – RIDERS AND SUPPORT PEOPLE — This Katie Couric Documentary — Sugar and Diabetes and Obesity Epidemic — Came out just days ago and has 120 feedback already. — You guys are doing great! Keep up the great work! — People just don’t know and aren’t able to grasp and understand the reality and truth in this. There should be five thousand feed back already. The world just doesn’t know. There genuinely may not be a seventh generation with enough health to do anything to take the land back if this epidemic is not stopped in it’s tracks. It is preventable with diet and exercise. Dennis is a perfect example. Dr. Jay Wortman “My Big Fat Diet” Documentary is another example. — After this war is won DECLARING WAR ON INDIAN CASINO’s AND GAMING, CLOSING ALL FIVE HUNDRED CASINO’S ON THE RESERVATIONS, needs to be next. These Casino’s are ten times worse than Diabetes. There will be no more Indians unless they are stopped and closed. Assimilation/Quantum Reductions so that they will have more “white” people to work at the Casino’s, like Las Vegas and Reno and Tahoe and Atlantic City. More money for the white man power brokers who are supplying everything for the Casino’s, five hundred Casino’s strong and growing. Five hundred cash cows. Hundreds of millions of dollars annually, “Billions of Dollars”. — Many leaders and Chiefs are taken in and fooled by all that money. “Blinded by the light”. — ” Blinded by the glitter of all that “gold”. — Thank for your time and looking at and reading this, miguich, or however you say it, thanks again, Tom Bunnell, a 100% White Man, 69 years old, from Detroit Lakes, Minnesota — White Earth — My grandfather moved onto the reservation 1935 — I would like to live to see the day “my” seventh generation, of white people “all” move off from the reservation. The people paid for their land and farms and resorts by the US Government and a few generations allowed to stay for awhile as the transformations take place with all land transactions going back to the tribes. It’s a wonderful place to live and I wish we white people could have such a beautiful piece of land even though it is a pittance of what you had and should have.