One of the questions I most often receive: Does being in ketosis automatically translate to fat loss?
For those too busy to read ahead, let me give you the punch line: No. For those who want to understand why, keep reading (hopefully this is still everyone). This topic is — surprise, surprise — very nuanced, and almost always bastardized when oversimplified, which I’m about to do, though hopefully less than most. Without oversimplifying, though, this will turn into a textbook of 1,000 pages.
From the ketosis series, or at least the first and second part, along with the video in this previous post, you should have taken away that ketosis is not some ‘magical state of mystery.’ It’s simply a state of physiology where our liver turns fatty acid (both ingested and stored) into ketones.
There seems to be great confusion around ‘nutritional’ ketosis (a term we use to distinguish ‘dietary-induced’ ketosis from the other 2 forms of ketosis: starvation ketosis and ketoacidosis, the latter a serious complication of type I diabetes). But, before I try to dispel any of the confusion, we need to go through a little primer on what I like to call “fat flux.”
One point before diving in, please do not assume because I’m writing this post that I think adiposity (the technical term for relative amount of fat in the body) is the most important thing to worry about. On the contrary, I think the metabolic state of the cell is far more important. While there is a correlation between high adiposity (excessive fat) and metabolic dysfunction, that correlation is far from perfect, and, as I’ve discussed elsewhere, I think the arrow of causation goes from metabolic dysfunction to adiposity, not the reverse. But, everyone wants to lose fat, it seems, so let’s at least get the facts straight.
Let’s start with an assertion: Barring the presence of scientific evidence I’m unaware of, and barring surgical intervention (e.g., liposuction), reducing the adiposity of a person is achieved by reducing the adiposity of individual adipose cells, collectively. In other words, the number of adipocytes (fat cells) we have as an adult does not change nearly as much as their size and fat content. So, for people to reduce their fat mass, their fat cells must collectively lose fat mass.
Fat flux 101
According to “An Etymological Dictionary of Modern English,” the word flux comes from the Latin word fluxus and fluere, which mean “flow” and “to flow,” respectively. While the term has a clear mathematical meaning in physics, defined by a dot product I promise I won’t speak of, you can think of flux as the net throughput which takes into account positive and negative accumulation.
If we start with a bucket of water and put a hole in the bottom, the result, needless to say, is an efflux of water, or negative water flux. Conversely, if we start with a bucket – no hole – and we pour water in, that’s an influx of water, or positive water flux.
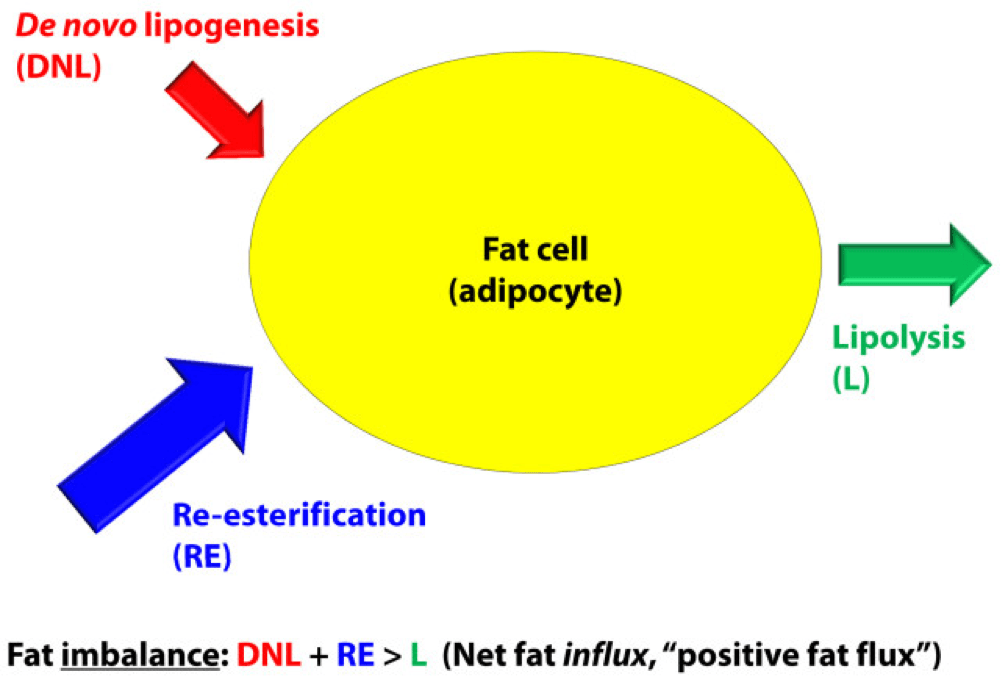
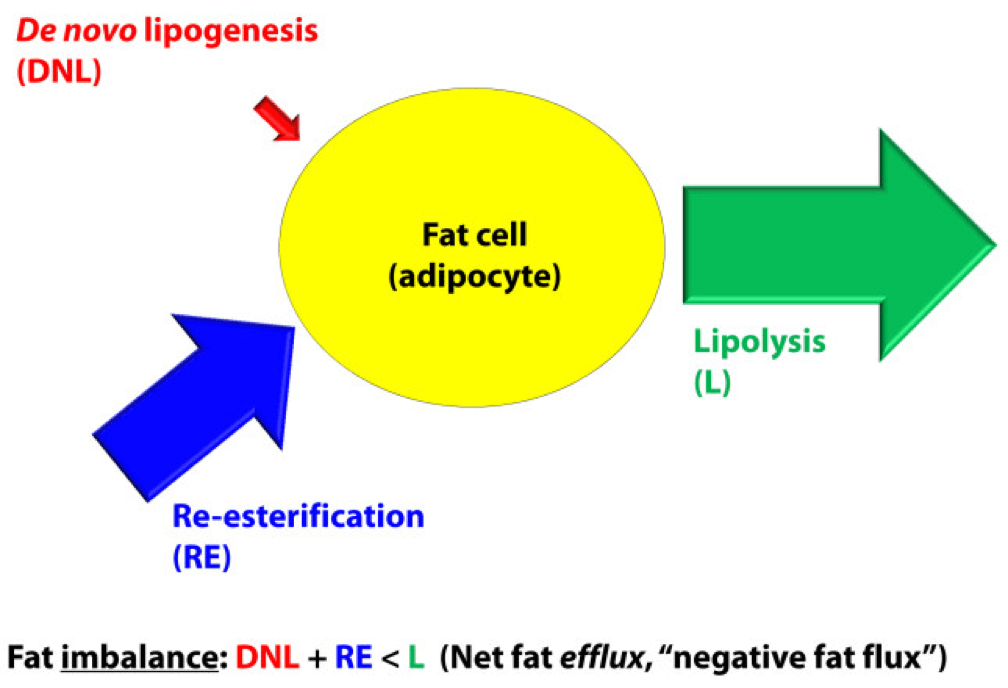
If that makes sense, then the idea of fat flux is pretty straight forward. If more fat enters a fat cell (called an adipocyte) than leaves it, the fat cell is experiencing a net influx – i.e., positive fat flux. And, if more fat leaves a fat cell than enters, the reverse is true: it is experiencing a net efflux, or negative fat flux.
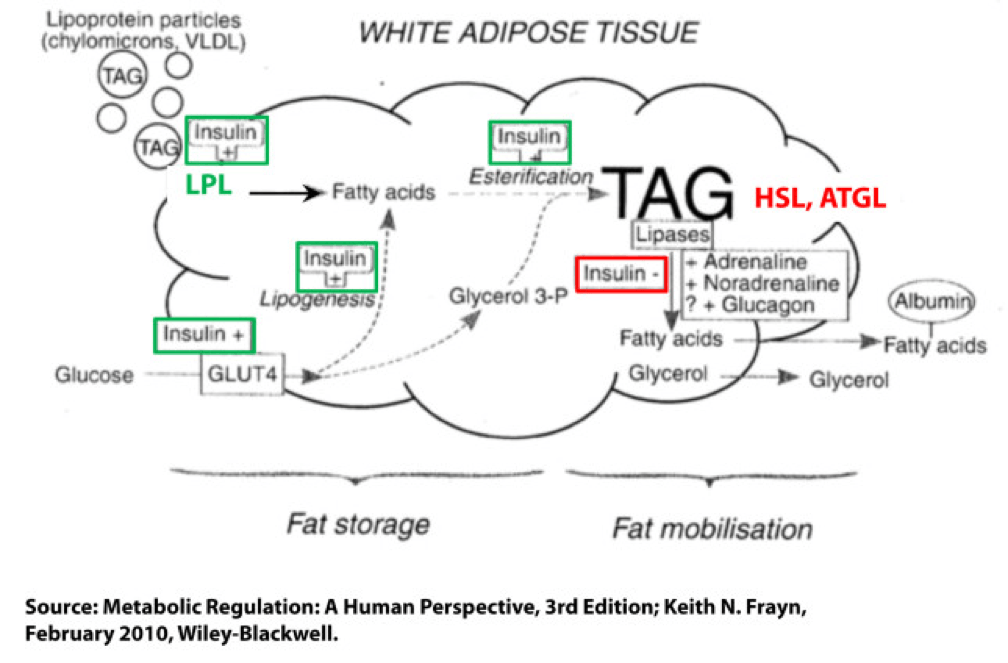
Not surprisingly, a fat cell is more complicated than a bucket. Basically, though, there are two “inputs” and one “output.” The figure below shows this in some detail. (TAG stands for triacylglycerol, which is another word for triglyceride, which is the storage form of fat.) The first thing you may appreciate, especially since I’ve highlighted it, is the role insulin plays in regulating the process of fat flux. Insulin does the following:
- Upregulates lipoprotein lipase (LPL), an enzyme that breaks down TAG so they can be transported across cell membranes. Since TAG are too big to bring across cell membranes, they need to be “hydrolyzed” first into free fatty acids, then re-assembled (re-esterified) back into TAG.
- Translocates GLUT4 transporters to the plasma membrane from endosomes within the cell. In other words, insulin moves the GLUT4 transporter to the cell surface to bring glucose into the cell.
- Facilitates lipogenesis, that is, facilitates the conversion of glucose into acetyl CoA which gets assembled into fatty acids along with glycerol.
- Facilitates esterification, that is, facilitates the process of assembling fatty acids into TAG (3 fatty acids per TAG).
- Inhibits hormone-sensitive lipase (HSL) and adipose triglyceride lipase (ATGL), two important enzymes that breaks down TAG into fatty acids and glycerol such that the fatty acids can be released from the fat cell. Once bound to albumin the free fatty acids are free to travel elsewhere in the body for use (e.g., to the liver for conversion to ketones, to the heart muscle or skeletal muscles for conversion to ATP).
- Though not shown in this figure, insulin appears to indirectly act on malonyl-CoA, a potent inhibitor of CPT I, one of the most important mitochondrial enzymes that facilitates the oxidation of fatty acids. (CPT I is what enables fatty acids to be shuttled into the mitochondria for oxidation, the process which releases or liberates their energy through electron transport.)
Other hormones and enzymes in the body also play a role. For example, under a sympathetic response, the so-called “fight or flight” response, adrenaline and noradrenaline (i.e., epinephrine and norepinephrine) activate HSL and ATGL to combat the effect of insulin as an inhibitor of lipolysis, thereby increasing lipolysis, or liberating stored energy from the fat cell. Glucagon may also play a role in this process, though the exact role is not as well understood, at least not in humans.
So in summary, insulin is indeed the master hormone that regulates the flow of fat (and glucose) into and out of a fat cell. There are other players in this game, to be sure, but insulin is The General. High levels of insulin promote fat storage and inhibit fat oxidation, and low levels of insulin promote fat mobilization or release along with fat oxidation.
If this sounds crazy – the notion that insulin plays such a crucial role in fat tissue — consider the following two clinical extremes: type 1 diabetes (T1D) and insulinoma. In the former, the immune system destroys beta-cells (the pancreatic cells that make insulin) – this is an extreme case of low insulin. In the case of the latter, a tumor of the beta-cell leads to hypersecretion of insulin – this is an extreme case of high insulin. Prior to the discovery of insulin as the only treatment, patients who developed T1D would become emaciated, if the other complications of glycosuria and dehydration didn’t harm them first. They literally lost all fat and muscle. Conversely, patients with insulinoma often present looking not just obese, but almost disfigured in their adiposity. Because Johns Hopkins is a high-volume referral center for pancreatic surgery, it was not uncommon to see patients with insulinoma when I was there. As quickly as we would remove these tumors, the patients would begin to return to their previous state and the adipose tissue would melt away.
For the purpose of our discussion, I’ve simplified the more detailed figure above into this simplified figure, below. I’ve tried to size the arrows accordingly to match their relative contributions of each input and output.
The first figure, below, shows a state of fat balance, or zero net fat flux.
Input #1: De novo lipogenesis, or “DNL” – Until the early 1990’s there was no way to measure this directly, and so no one really had any idea how much this process (i.e., the conversion of glucose to fat) contributed to overall fat balance. Without going into great technical detail, , arguably one of the world’s foremost authorities on metabolomics and DNL, developed a tracer technique to directly measure this process. If I recall correctly, the original report was in 1991, but this paper is a great summary. Published in 1995 in the Journal of Clinical Investigation, this paper would go on to become the “citation classic.” This study demonstrated that under eucaloric feeding conditions, with about 50% of energy coming from CHO, DNL did not represent a significant contribution to fat flux. It was about 5%, hence the tiny red arrow under a state of fat balance (i.e., a state where fat entering the fat cell is equal to fat leaving the fat cell). A very important point to be mindful of, however, is this: this represents an average throughout the body and does not differentiate specifically between, say, DNL in the liver and DNL in the periphery (i.e., fat cells). This limitation is not trivial, but rather than focus on the very specific details of this paper, I’d rather use it as a framework for this discussion. (This paper is really interesting, and were it not for the fact that this post is going to be long enough, I would say much more about it. As such, I will probably do a full post on this paper and related topic in the future. The 1995 paper also examined what happened to DNL during periods of over- and under-feeding CHO and fat.)
Input #2: Re-esterification, or “RE” – In a state of fat balance, RE is largely composed of dietary fat sources that are not immediately used, but rather stored for later use. (Nuanced point: RE also includes fatty acids that were previously liberated from adipocytes, not oxidized, and are now being recycled back into TAG. This is a normal consequence of fat liberation. The fat cell probably ‘deliberately overdoes it’ by liberating more fatty acid from TAG just to be safe; that which is not oxidized is re-esterified. The exact balance of RE composed from dietary sources versus recycled fatty acids will depend on fat consumption and energy demands of the person. For the purpose of simplicity, this diagram does not show some portion of the L fraction returning to the RE fraction, though this is exactly what is happening in ‘real life.’)
Obviously, though, the relative size of the blue arrow depends on how much fat one is consuming and how many metabolic demands are in place for fatty acids. The latter is highly determined by dietary composition (see the discussion on RQ, or respiratory quotient, at about minute 31 in this video).
For the real aficionado, there is another wee bit of nuance here. This study, published in 1991 in the Journal of Lipid Research, suggested that the RE process is a bit more complicated than simply re-assembling fatty acids on a glycerol backbone inside an adipocyte. Based on these experiments, which used a similar* tracer method to the one used by Hellerstein et al. to evaluate DNL, the authors (which included Rudy Leibel, the co-discoverer of leptin) suggested that RE requires an intermediate step outside of the adipocyte in the interstitial and capillary space (figure 8 of the paper demonstrates this very well schematically).
(*) Technically, Hellerstein et al. used a heavy isotope; Leibel et al. used radioactive isotopes.
Output: Lipolysis, or “L” – Finally, in a state of fat balance, lipolysis must be equal to the sum of DNL and RE. This is true if we are talking about tiny little fat cells or giant ones. Remember, it’s the balance that matters.
I hope it’s clear from this summary that there are an infinite number of physiologic states that can satisfy the equation of fat balance: DNL + RE = L. For example, someone like me who is in fat balance (i.e., I’m neither gaining nor losing fat mass at this point) on a ketogenic diet with daily fat intake often exceeding 400 grams, has virtually zero DNL, but quite high RE, especially after meals. Consequently, I have very high L. If you took a person on a very low-fat diet (e.g., 20% fat, but 65% CHO), they would have modest DNL and low RE, but they would have low L. We would both be in fat balance, but we satisfy the equation DNL + RE = L by very different means.
OK, so let’s turn our attention to the non-equilibrium states: Net fat influx and net fat efflux.
Fat influx
In a state of net fat influx – accumulation of fat within a fat cell – the following condition must be met (on average): DNL + RE > L. (I say “on average” because, of course, a fat cell is a dynamic system with constant changes in these parameters. So, at any moment in time the balance can shift, but over a period of time the equation is correct.)
The next (overly simplistic) figure below gives you a representative state of what fat influx or ‘positive fat flux’ probably looks like. DNL is higher, but still relatively small, unless overfeeding CHO. RE is larger than it was in a balanced state, but not necessarily ‘huge.’ Most cases of net fat influx are probably governed by low L. In other words, fat accumulation is probably more governed by a failure to mobilize (breakdown TG into fatty acids for export and use) TAG than anything else.
Have you ever spoken with someone who is trying desperately to lose weight (fat) who says, “I don’t understand what’s happening…I hardly eat any fat, and yet I can’t lose a pound (of fat)!” The skinny people in the group scoff, right? Well, not so fast. It’s quite possible, if the hormones that regulate fat tissue are not working in your favor, to do such a poor job mobilizing fat from fat cells, and oxidizing that fat (see below), that you can be in fat balance, or even fat imbalance with accumulation, despite small DNL and small RE.
If you think about it, lipolysis (L), or liberating fat from a fat cell is a necessary, but not sufficient condition to actually generate the free energy inherent or stored within it. One more major step is necessary – oxidizing the fatty acid via the process of beta-oxidation. This is where one actually gets the energy (ATP) from fatty acids. The same hormones and enzymes that promote L, directly or indirectly act on other intermediaries that promote oxidation, more or less. The converse is also largely true.
Brief digression: I’m always troubled by folks who have never tried to take care of someone who is struggling to lose weight (fat), and who themselves have never been overweight, but who insist obesity is ‘simply’ an energy balance problem – people eat too many calories. When eternally lean people preach about the virtues of their ‘obvious’ solutions to obesity – just eat less and exercise more – I’m reminded of a quote (source unknown to me), “He was born on the finish line, so he thinks he won the race.” You only need to meet one woman with PCOS, or one person with hypothyroidism, or one child with Cushing’s disease to know that adiposity can – and is – largely regulated by hormones. The fact that such patients need to create a positive energy balance (i.e., eat more calories than they expend) to allow it does not seem to provide a meaningful insight into the mechanism of why.
Fat efflux
In a state of net fat efflux – reduction of fat within a fat cell – the following condition must be met (on average): DNL + RE < L (same caveat as above on the idea of “on average”). Again, looking at the figure, you can see one physiologically common way this occurs, the setting of carbohydrate restriction. DNL is reduced (probably even to immeasurable levels, depending on the extent of restriction), but RE actually goes up. The net efflux, however, results from the greater increase in L.
A person in nutritional ketosis, if experiencing fat loss, probably looks like this. (Don’t worry, I have not forgot the opening questions: Does being in nutritional ketosis automatically put you in this state?). Certainly another state of net fat efflux is starvation. DNL and RE are both very small, especially DNL, and lipolysis is quite large. This is probably the most rapid state of negative fat flux a human can experience.
So what we do about it?
I do not believe there is only one state, shy of total starvation, which will assuredly put you in state of negative fat flux. Of course, starvation is not sustainable, and therefore should be taken off the table as a viable long term eating strategy.
What about profound caloric restriction? Yup, this is probably (though not necessarily) going to work, depending on how “profound” is defined. If defined as a 40% reduction of energy stable intake, it’s probably going to work. If defined as a 10% reduction, it would be difficult to know without knowing at least two other things:
- Baseline level of insulin resistance;
- RQ of pre- and post-diet.
What about dramatic alterations in macronutrient composition? This is where the discussion gets really interesting. Many people, myself included, advocate a diet that overall reduces insulin secretion. The rationale, of course, is provided by the first figure above (from the textbook) and a slew of clinical studies which I will not review here (see Gardner JAMA 2007, Ludwig JAMA 2012, and Shai NEJM 2008 to name a few).
But, the bigger question is why? Why do most (but not all, by the way) people with excess fat to spare who are on well-formulated carbohydrate-reduced diets lose fat? (Notice, I did not say weight, because the initial – and often rapid — weight loss achieved by many is actually water loss.)
Is it because of a physiologic change that leads them to reduce overall intake?
Is it because of a physiologic change that, despite the same intake in overall calories, increases their energy expenditure?
Is it some combination of these?
I wish I knew the answer, but I don’t (universally). I believe we will know the answer to this question in a few years, but until then, I’m left to offer the best my limited intuition can offer. In other words, what I suggest below is my best interpretation of the literature, my personal experience that I’ve had with hundreds of other people, and my discussions with some of the most thoughtful scientists in the world on this topic:
Thought #1: I suspect that many people who reduce simple carbohydrates and sugars end up eating fewer calories. This observation, however, may confound our understanding of why they lose weight. Do they lose weight because they eat less? Or, do they eat less because they are losing weight? I suspect the later. In this state, lipolysis — and by extension, given the hormonal milieu, oxidation — are very high, certainly relative to their previous state. By definition, L > DNL + RE, so there is ample ATP generated by oxidation of the fatty acid. If you believe (as I do*) that the liver is the master organ of appetite regulation, increases in ‘available energy’ (i.e., ATP) would naturally reduce appetite (though I don’t think we know if ATP per se is the driver of this feedback loop). But don’t confuse what’s happening. They are not giving up fat from their fat cells because they are eating less. They are eating less because they are giving up fat from their fat cells. Big difference.
(*) The especially astute reader will note that this is the first time I have made reference to this point. I have been heavily influenced recently by the work of Mark Friedman, and a discussion of this point is worth an entire post, which I promise to deliver at some point in the future. If you can’t wait, which I can understand, I highly encourage you to start scouring the literature for Mark’s work. It’s simply remarkable.
Thought #2: I also suspect that some fraction of people who follow this eating strategy lose fat without any appreciable reduction in their total caloric intake, at least initially. What?, you say, doesn’t this violate the First Law of Thermodynamics? Not at all. If L > DNL + RE, and the increase in lipolysis (i.e., fatty acid flux out of the fat cell) results in increased oxidation of fatty acids, energy expenditure (EE) would be expected to rise. A rise in EE, in the face of constant input, is a sign of fat loss. What differentiates those in this camp (I was in this camp) from those above (point #1), is unclear to me. It may have to do with concomitant exercise. I have seen unpublished data, which I can’t share, suggesting non-deliberate EE rises more in a low RQ (high fat, low carb) environment when a person is exercising significantly. I’m not stating the obvious – that the deliberate EE is higher – that is clearly true. I’m suggesting resting EE is for some reason more likely to rise in this setting. Since I’m taking the liberty of hypothesizing, I would guess this effect (if real) is a result of the body trying to keep up with a higher energy demand and making one trade-off (generating more free ATP via more lipolysis) for another (ensuring a constant supply of available energy to meet frequent demands). It is also possible that this increase in free/available energy results in an increase in deliberate EE (i.e., the person who suddenly, in the presence of a cleaned up diet feels the desire to walk up the stairs when they previously took the elevator). Finally, and perhaps most importantly, whether or not this up-regulation of energy takes place may be dependent on the other hormones in the body that also play a role in fat regulation, including cortisol, testosterone, and estrogen. They could be partly or mostly responsible for this. The literature is quite dilute with respect to this question, but in my experience (feel free to dismiss), it is not uncommon to see a reduction in cortisol and an increase in testosterone (I experienced about 50% in free and total testosterone) with a dietary shift that improves food quality. The same may be true of estrogen in women, by the way, though I have less clinical experience with estrogen.
Thought #3: As a subset to the point above (point #2), in an ‘extreme’ state of carbohydrate restriction, i.e., — nutritional ketosis — there is an energy cost of making the ketones from fatty acids. I referred to this as the “Hall Paradox” after Kevin Hall, who first alerted me to this, in this post (near the bottom of the post). What is not clear (to me, at least) is if this effect is transient and if so, how significant it is. I recall that during the first three months of my foray into nutritional ketosis, I was eating between 4,000 and 4,500 kcal/day for a 12-week period, yet my weight reduced from 176 lb (about 9.5% bf by DEXA) to 171 lb (about 7.5% bf by DEXA), which means that of the 5 pounds I lost in 12 weeks, 4 were fat tissue. Today, however, I don’t consume this much, closer to 3,800 kcal/day, and one reason may be that two years later my body is more efficient at making ketones and this so-called “metabolic advantage” is no longer present.
(I have always found the term “metabolic advantage” to be misleading, though I’m guilty of using it periodically. It’s really a metabolic disadvantage if your body requires more energy to do the same work, but nevertheless, people refer to – and argue vehemently about – this phenomenon. The question is not, does it exist? One look at individual summary data from David Ludwig’s JAMA paper on this topic makes that clear. The questions are, why does it only exist in some people, what relevance does it have to fat loss – is it cause or effect? – and, for how long does it persist?)
Thought #4: For reasons I have yet to fully understand, some people can only lose fat on a diet that restricts fat (and by extension a diet that is still high in carbohydrate, since I’m excluding starvation and profound caloric restriction from this discussion). In my experience (and Gardner’s A TO Z trial seems to validate this, at least in pre-menopausal women), about 20% of people aspiring to reduce adiposity seem to do it better in a higher RQ environment. Using the Ornish diet as the example from this paper, I suspect the reason is multifactorial. For example, the Ornish diet restricts many things, besides fat. It restricts sugar, flour, and processed carbohydrates. Much of the carbohydrate in this diet is very low in glycemic index and comes primarily from vegetables. So, I don’t really know how likely it is to lose weight on a eucaloric diet that is 60% CHO and 20% fat, if the quality of the carbohydrates is very poor (e.g., cookies, potato chips). The big confounder in these observations is that most low-fat diets, though still modestly high in RQ relative to a low-carb diet, reduce greatly the glycemic index and glycemic load, as well as the fructose.
Which brings us to the point…
Does being in nutritional ketosis ensure negative fat flux (i.e., fat loss, or L > DNL + RE)?
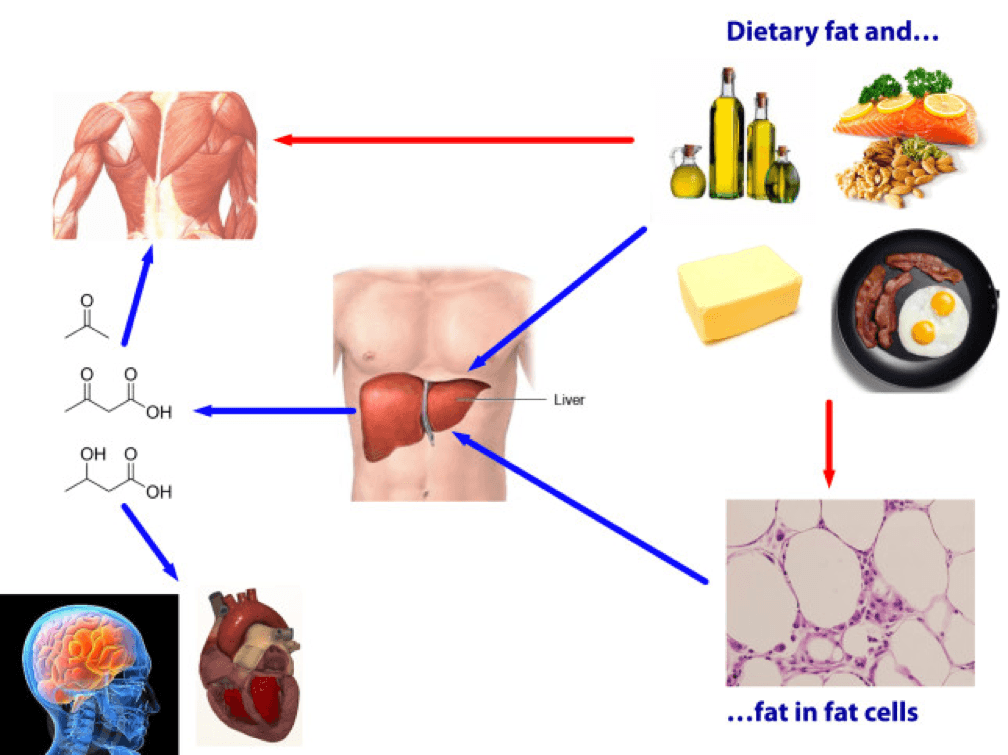
Being in ketosis tells us nothing about this equation! Let me repeat this: It is metaphysically impossible to infer from a measurement of B-OHB in the blood if this equation is being satisfied. It just tells us that our body is using some fraction of our dietary fat and stored fat (once it undergoes lipolysis) to make ketones, given that glucose intake is very low and protein intake is modest (net effect = minimal insulin secretion).
If you look at the figure below, you see this point (It’s simplified, obviously, and for example, does not show that fat from fat cells can be used directly by skeletal muscles). Nothing in this figure implies a reduction in the size of the cells at the bottom right of the figure. It’s quite possible, of course, since ketosis results in a large L and implies a very small DNL. But, if (small) DNL + (very large) RE is greater than (large) L, guess what? Fat flux is net positive. Fat is gained, not lost. Still in ketosis, by the way (quantified loosely by fasting levels of B-OHB greater than about 0.5 to 1 mM), but not losing fat. (I hope the first attempt at a solution in this setting is obvious by now, notwithstanding the fact that I’ve seen this situation dozens of times with more than one solution, including the ‘obvious’ one — reducing fat intake.)
The other myth worth addressing is that the higher the level of B-OHB, the more “fat burning” that is going on. This is not necessarily true at all. As you can tell, I love equations, so consider this one:
B-OHB (measured in blood) = B-OHB produced (from dietary fat) plus B-OHB produced (from lipolysis of TAG) less B-OHB consumed by working muscles, heart, brain.
How does knowing one of these numbers (B-OHB measured in blood) give definitive answers to another (B-OHB produced from lipolysis of TAG)? It can’t. That’s the problem with multivariate algebra (and physiology).
Many people who enter nutritional ketosis do so, I worry, because they believe it “guarantees” fat loss. I hope I have convinced you that this is not true. Nutritional ketosis is one eating strategy to facilitate negative fat flux, and it works very well if done correctly. It comes with some advantages and some disadvantages, just like other eating strategies. When I get back to the series on ketosis, I will address these, but for now I felt it was very important to put things in perspective a bit. Furthermore, I am convinced that it is not the ideal eating strategy for everyone.
Delorean by Marci Maleski is licensed under CC by 2.0





Peter,
From your site and the phenomenal Phinney and Volek books I read that the ideal range for blood ketones is 1.5-3 mmol/L. In one of their books, it shows a ketone level chart that shows a curve where levels over 3 mmol/L approach starvation ketosis and then at much higher levels, keto acidosis. Is there any literature that you’re aware of that looks at the effects of ketone levels above 3, but lower than the amount present during keto acidosis?
I ask because after reading their books, I began a reduced carbohydrate diet this week and I’m only 4 days in. Being a geek, I bought the Precision Xtra and the (expensive) ketone strips to measure ketone levels and I’ve received readings of 5.4, 6.7, and 5.7 mmol/L. Is there any literature that suggest these readings should be harmless? Or is there incentive to add carbohydrates to achieve levels between 1.5-3? It’s referenced at the ideal range, so is there some knowledge that something negative happens above 3 mmol/L? Also is there any indication of what might amuse those heavy levels in such a short time period? I read that keto adaption takes a few weeks, and that it takes a while for blood ketone levels to rise above .5 mmol/L. I’m a 29 year old woman, 5 weeks post partum and breastfeeding. My carb intake hasn’t been super restrictive either as there isn’t much in the way of literature on ketosis and lactation. I’ve been eating dark chocolate, berries, fresh cherries daily. My ketone readings are a mystery to me!
DKA does not typically occur until BHB levels reach north of 15 mM. More importantly, they are virtually impossible to consider in the face of a working pancreas. Does seem odd, though. Perhaps your meter is not calibrated correctly?
You can get test solutions for the Precision Xtra to check it on both glucose and ketones.
I think keto acidosis also requires high blood glucose, hence the meter flagging a high glucose for you to test for ketones. https://endoemergencies.org/sample-chapter.html
https://www.anaesthesiamcq.com/AcidBaseBook/ab8_2.php says of starvation ketosis “The acidosis even with quite prolonged fasting is only ever of mild to moderate severity with ketoanion levels up to a maximum of 3 to 5 mmol/l and plasma pH down to 7.3”
Just a note that the expensive ketone strips are available through universal drugstore for $2 a piece. They come from Canada, so may be a longer delivery time. Am I allowed to say that on this site??
Peter, I find I readily lose weight when I cut calories from my diet. I’ve done that in a few different ways – skipping whole meals, removing food items from meals, etc. I know you say it’s not about the calories but rather the amount of non-complex carbs that are in the diet, but it seems to me that consumption of very calorie-dense low carb foodstuffs could contribute to obesity. What is your opinion on that?
(I can lose as much as 5-6 lbs in less than a week by doing this. I weigh myself reliably in a fasting state each morning after voiding. The weight is a key indicator for me to go hard on diet or ease up a little. Physical activity leading to expenditure of calories could be a factor here but I think much less so.)
I respect and value your input.
Dan
Dan, it would be hard to imagine a scenario, outside of near or total starvation, where ones fat mass could change by 5 to 6 pounds in a week. My weight, too, fluctuates by this much at times, but it’s clearly movements in water (e.g., more or less retention due to inflammation resulting from over- or under-training, illness, travel, supplementation). An actual fat deficit of 2 pounds in one week is VERY significant.
Some good writing here and a very useful discusion.
Just a little addition to the hepatic DNL discussion; this is around 5% normally, but if the liver is diseased can increase to 25%. A lot of the glucose in such a scenario is not used to synthesise palmitate, but to convert palmitate to oleate; the supply of oleate means that palmitate is more likely to be converted to TGs, less likely to be oxidised. (palmitate alone cannot be made into TGs, is instead a PPAR-alpha ligand)
Now, we have diets that produce NAFLD quite consistently these days; fructose plus enough linoleate to drown out the fat-burning signalling from DHA. So the rate of hepatic DNL is sneaking up.
Info derived from this book: https://books.google.co.nz/books?id=T_Jwh1OmYV8C&printsec=frontcover#v=onepage&q&f=false
Hi Dr. Attia!
‘ When I get back to the series on ketosis, I will address these, but for now I felt it was very important to put things in perspective a bit. Furthermore, I am convinced that it is not the ideal eating strategy for everyone.’
Did you mean it’s not ideal for people/athletes doing higher intensity workouts? I noticed on my N=1 performance drop in NK. I can up fat as much as I want but running or biking over 80% max HR and longer lifting workouts suffer. I can’t get max performance like eith carbs and can easily overeat fats, hopping I’ll perform better my next workout. But it doesn’t happen.
No, I meant what I said. If I meant it’s not for athletes, I promise I would have said so. I understand what you’re describing, and experienced it for about 18 months. However, the effect is gone and I appear to have no difficult reaching anaerobic peaks I did 2 or 3 years ago. Adaptation seemed to take me a while.
Peter,
Thanks for yet another incredible post. I think I speak for all your readers when I say how much we appreciate the amount of time and dedication that clearly goes into the research behind your posts. If it’s a choice between more frequent but less in-depth forays versus posts that are fewer and farther between but so meticulously researched and detailed, I’ll opt for the latter every time.
I’m fascinated (and simultaneously annoyed, discouraged, and inspired,) by the ever-changing theories and explanations behind obesity as science digs deeper. And even more so, as interested parties (yourself near the top of this list) continue to dissect the information. Thank goodness for curious minds that are *not* satisfied by simple and straightforward — but often INCORRECT — answers. I shudder to think where metabolic research as a whole would be today if no one had ever spoken up and said, “Hey, wait a minute…I *am* eating less and moving more. Why aren’t I losing weight?!” Or, “Hey, doc, weren’t my cardiovascular markers supposed to *improve* on this low-fat, high-grain diet you put me on? How come they’re getting worse?”
One more point before I get out of your hair…
I find it ironic that even among the people who visit your blog–and are presumably aware of just how unbelievably complex metabolism is–there are those who ask how many calories they should be eating, or how many carbs, fat grams, etc. If only it were that simple, folks. (No one ever seems to ask how much sleep they should get, or how much they need to calm down behind the wheel in traffic. Or how a day off, lounging in a park with a hammock and a good book could lower their cortisol levels. I *wish* it were only a matter of what we do or do not cram down our pieholes.)
Amy, thanks so much for sharing these insights. I’ve never intended this blog to be for the casual reader, and I do think it attracts the absolute smartest and most curious readers out there. From what I’ve noticed, those looking for bumper stickers don’t still around long. I mean, who in their right mind would read this 4,000 word post on fat flux if they thought they only needed to know how many calories to eat!
Peter, July 27th you commented to Dan that
‘it would be hard to imagine a scenario, outside of near or total starvation, where ones fat mass could change by 5 to 6 pounds in a week’.
Jimmy Moore (livin the vida low carb) writes that he lost 100 pounds in the first 100 days of following the Atkins diet. At 2 lbs. of fat per week he would have lost 28.56 lbs. of fat. If you subtract a generous 15 pounds for water fluctuations (he was quite heavy at the start), you are still at 56.44 of unexplained loss. Are you saying that this weight would most likely have been loss of lean mass?
I am new to the process and one of my fears is that I preserve lean muscle mass. I have been on less than 20 carbs for about 6 weeks now. Keeping my carbs consistant, I have just reduced my protein to move my blood ketones from .6 to .9 (so far) in an attempt to get into optimal ketosis of 1.5 – 3.0. I have lost almost 8 lbs. in the past 12 days while drinking the same amount of water (but I understand my body may handle the water differently).
QUESTION: At what point should I start to be concerned that the loss is lean muscle mass? Also, this might be a silly question, but is protein the only variable in maintaining lean mass, or does the number of calories/fat come into play.
As usual thanks,
Kathy
I guess anything is possible, and I’m not sure what Jimmy started at, but it’s far outside of the norm.
Hi Peter,
Thank you for taking the time to share all of your knowledge. You’ve provided a great service for all of us searching for unbiased accurate information.
I would like your take on someone adopting nutritional ketosis that is also dealing with a-fib. There seems to be conflicting information as to NK being harmful, causing more problems.
NK could make a-fib if electrolytes are not managed carefully, especially potassium and magnesium. I have not seen research around this, though, just a few clinical observations.
I have a friend who is a lone A-fibber. He controlled his A-fib with large – on the order of several grams of Mg, K and Na. He has also been NK for 4 years. The electrolytes are a major answer for him – when the electrolyte levels are low he goes into A-fib, high he does not. The NK does not seem to be part of the answer for him but he does not get altitude sickness and has more fun exercising when he is NK. He does not need as much water skiing above 11,000 feet and he only eats morning and night. He prefers the NK state. He has type 2 diabetes and Alzheimer’s in his family so he figures that besides the better performance at recreational sports, he may be slowing down the progression toward these conditions.
Peter,
I assume there are likely to be a number of factors which will determine how well an individual is suited to a ketogenic diet. I do not wish to get hung-up on a tenth-order term but there is one factor I would like to like to propose.
I understand there are a number of studies which have shown individuals who sleep longer and/or who have better quality sleep tend to eat and weigh less (I have seen it postulated this has to do with leptin and ghrelin regulation). Before I completely changed my own diet I had significant problems with sleep and no matter how much (normally cereal) I ate often late at night, I always seemed to wake up in the middle of the night starving and felt completely exhausted the following day. This in turn could theoretically have resulted in me eating more and gaining more weight than if I had enjoyed better quality sleep.
Do you think this is a factor worth considering i.e. how well an individual sleeps or if they have any difficulties with sleep (obviously there are a number of other lifestyle factors which influence quality of sleep itself)?
As I noted above, I do not wish to overemphasise this effect particularly if it is a side-effect of some other much more important factor.
One should be a bit wary of these data. They are very associative and contain zero causal information. I can think of a dozen reason why those who sleep more, and sleep with better quality, have less adiposity, including but not limited to the ones you mention. That said, if you’re not sleeping well, absolutely resolve that issue! Hint: Vit D deficiency needs to be corrected.
Apologies for not explaining, sleep quality has been much better adopting low carb diet.
It’s amazing you mentioned Vitamin D as I recently had this tested due to my skin type, environment and occupation (often work in office basement) and I was found to be deficient.
Points taken, just wanted to throw one in the mix for your view.
Hi Peter,
I have a question about keto adaptation. In one of your videos you mention that it takes about two weeks to reach a keto adaptive state. After you are keto adapted, if you fall out of ketosis because you ate too many carbohydrates on a given day, does it take another two weeks to return to keto adaptation?
Also–I might be confused on this point–is there a difference between keto adaptation and being in ketosis? If there is, is there a reason to prefer being keto adapted?
Thanks! Love your blog!
No, usually quicker. Adaptation probably takes longer than 2 weeks, also. The more I study this, the longer it appears to take for full functional adaptation. 2 weeks is generally good for day-to-day stuff, but not necessary high-end performance.
Hi Peter,
This probably belongs in one of your posts focussing on sugar, but I thought you might find it interesting. It is Australian, out of the University of Adelaide and on Australian public television last night. The site below has the video segment (also downloadable) and the transcript:
https://www.abc.net.au/catalyst/stories/3816207.htm
Yes, quite interesting, isn’t it. Hard to believe this stuff is good for us.
Hi Peter, I greatly respect how you are educating all of us fatsos to lose weight. I have been on keto for around 2 weeks now and already lost close to 15 lbs. My main issue is this, I travel maybe once or twice a month for work. Can you kindly write an article on what you eat when you travel. It will be so very kind of you.
Present for you on your journey of self healing and discovery have you found Ray Peat yet? he’s the man for the man with an open mind – dr of physiology and what he knows about the cell is amazing! https://raypeat.com/articles/articles/sugar-issues.shtml ( been there done that and wish i’d found him sooner ) it is easier to listen to him if you google up some of the interviews he has done around the place. Goodluck with your studies.
I’ve read a bit of his stuff.
Thanks Peter, useful as always.
I know you have this on your “coming soon” session, but I’ve been struggling to find the scientific basis behind it. Why protein overconsumption jeopardizes ketosis maintenance?
Thousands of LCHF dieters make this “common” mistake (protein overconsumption) especially when starting the diet, given the common sense against fat consumption (seems you’ve incurred in that same mistake yourself) and results show that shifting a fraction of your caloric intake from proteins to fat (keeping protein intake around 1-1.5g/kg) enhances ketosis and weight loss.
However, as per my understanding (please correct me if I’m wrong) aminoacids can only be processed into glucose in the liver via gluconeogenesis (GNG), and it seems that there are no indications that GNG is a supply-driven process (higher availability of protein, higher level of GNG).
So what am I missing here? How do we get to the common “25-40% of our protein intake is processed as carbs” affirmation?
Thanks so much in advance!
p.s. sorry for jumping into something already listed in the “coming soon” section, but a single line (let’s call it a teaser) would be quite helpful…
It is GNG, and probably insulin, too. Protein also stimulates insulin release and insulin inhibits conversion of FFA to BHB.
I have been reading HFLC diet information extensively for weeks; numerous different sites including many of your blogs, writings and responses to many posts your site. I also have read Gary Taubes 2 books (‘Why we Get Fat/ Good Calories/ Bad Calories).
I saw something you wrote in one response (i.e.- “I had a coronary CT in 2009 which prompted this intervention.”), that has intrigued me to comment in hopes you will have some opinion on the best diet for me.
I have a strong family history of CAD (father- MI @40, mother- hyperlipidemia/ MI/CABG early 70’s, brother- CABG early 40’s). Since my twenties, I have always trended with high total chol, LDL but High HDL that I thought I was controlling fairly well with healthy diet ( 🙁 ) of complex carbs/LF/ minimal processed foods) and exercise. I have always been active, thin ( BMI < 22 my whole life). This year, I've had advanced lipid testing twice since Jan. (2nd time after starting Niaspan after 1st test). Now, I am at a loss as to how to eat??? I have discordant results, Apo- B is better but still high, LDL-P normal. Unfortunately, I have Apo E 3/4.
So, would you recommend the HFLC diet and see what my lipid response is to that? Or go to LCLF??
Thanks for any input. Keep up the great work; my husband is on board with your diet (he's metabolic syndrome, which I'm sure will change with diet).
Carol, in all but the most obscure cases, LDL-P drives risk, rather than apoB, so if LDL-P (by NMR) is at goal based on your history, your doctor should be pleased. “At goal” will need to be defined by your doctor. For some people, that may be as low as <800 nmol/L, while for others it may be <1,200 nmol/L.
I also meant to say I had a CAC with a 369 score!! (Which is why I was prompted to write you because of your post about your scan).
Thanks Peter; you are doing great work.
Hi Peter,
I am on a diet which begins with 3 weeks of almost no carbs (less than 3g) and gradually adds back 10g per week to determine the optimal level for weight loss. The first week I lost 4kg (which I assume is water) and have since been standing still. I have tested my urine with ketostix, which also shows no ketosis. (in week 2 it turn slightly pink, but week three nothing). I have been sticking to this so strictly and am quite dissapointed that it isnt working. I also havent had any of the symptoms of ketosis. What could be the cause for not reaching ketosis? Should I start reintroducing carbs (10g) before I have actually reached ketosis?
I assume you mean 10 gm per day, not per week, right? My best guess is that you’re consuming too much protein. Very hard to be in NK with more than about 120 gm of protein in your diet.
Dr. Attia – Thanks for the blog, the right amount of information for people like me who are not doctors but crave the detail! I am a nursing mom, have 3 kids, and work as a management consultant. Needless to say, the first thing that goes out the window is my workout, against my instincts! My problem is, I am “pre-diabetic” with a history of diatebetes in my family. Over the last 5 years, I have tried every workout possible, every diet possible, but I lost a few pounds initially and stall. Being a vegetarian makes it harder too. Anyway, long story short, I need to fix my “pre-diabetic” state and have enough energy for my kids. I tried the higher fat, low carb levels, gained much from the increased energy levels, but lost 0 lbs. Also, I worry (not to my real question), if it is ok for my baby to be drinking breast milk while I am in ketosis. (The cave women did this right? They only ate meat !) So it should be ok for my baby? Please point me to something on this, or formulate your own hypothesis, I will take anything.
Janaki, the main goal should be to fix your IR first, and worry about what the scale says second. There are enough hormonal changes in your body right now, that weight loss may be tough.
What about breastfeeding while in ketosis? Do you think that ketones can get into breastmilk?
When I don’t answer a question, it’s usually for one of two reason: I’m not qualified to answer; the question is a request for medical advice, which I am legally not permitted to provided.
How do you fell about the association of Omega-3 Fatty Acids being linked to increase risk in Prostate Cancer?
I read the study a few weeks ago, and did not find it at all compelling. Read the commentary of Bill Harris on Lecturepad.org for a great review.
Hi Peter,
After losing about 80 lbs on Atkins in 2002, I am now trying NK again to lose weight. I abandoned it in 2003 for two reasons. 1) I started feeling really awful during workouts 2) It was freaking my wife out because she thinks that low-carb is really unhealthy. Over the past decade I gained all that weight back in spite of running three times a week, etc. etc. The high carb=high insulin response makes a good deal of sense.
So I am back in NK again. It feels great! I took the “new” advice of supplementing my sodium and I have had little trouble with my workouts. However, my wife is still freaked out. I have addressed some of her fears, but she has two questions that I have not been able to answer:
1) What of the loss of antioxidant benefits from a diet high in greenery? Is that just propaganda?
2) What of the proportionally higher consumption of nitrates? I have found that many convenient low carb meats are filled with nitrates, and we are both worried about higher cancer risk. I know that it is possible to avoid nitrates while doing low carb, but it takes alot more work.
Thanks, Peter. I appreciate the work you do, including your N=1 human Guinea pig experiments. It is truly meaningful.
Sean, not sure you need to abandon greenery. I’m pretty sure I eat more salad than 99% of Americans, though I’m in ketosis. That said, I don’t find the evidence compelling that dietary antioxidants do anything (vs. the effect being the removal of things that do harm).
Ditto on the nitrates. That is, no need to consume them in any great quantities, but no compelling science they are as bad the propaganda would have us believe.
Thanks, Peter. I suppose it is just a matter of challenging firmly entrenched beliefs through honest scientific inquiry.
Hi Sean,
Don’t forget that cholesterol is an antioxidant!
Also: glutathione, the body’s “master antioxidant” is actually a peptide (made from amino acids) and you get more amino acids from protein foods than from, say, lettuce & spinach. 😉
Colored fruits & veg aren’t the only ways to get antioxidants. I’m not saying whether someone would be better off including them or not; just pointing out that they’re not the only game in town.