In this episode, Jason Fung, nephrologist and best-selling author, shares his experiences utilizing an individualized approach to fasting to successfully treat thousands of overweight, metabolically ill, and diabetic patients, and why being a doctor who specializes in kidney disease gives him a unique insight into early indications of metabolic disease. We also have a great discussion on insulin resistance where Jason makes the case that we should actually think of hyperinsulinemia as the underlying problem. We also discuss the difference between time-restricted feeding, intermittent fasting, and dietary restriction (e.g., low-carb) and how they can be used to attack the root cause of T2D, metabolic syndrome, and obesity. We also have a fascinating discussion about the limitations of evidence-based medicine which leads to a conversation where we compare and contrast the scientific disciplines of medicine and biology to theoretical physics.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Comparing scientific disciplines: Medicine and biology versus physics [7:25];
- The limitations of evidence-based medicine [12:30];
- Early signs of metabolic disease: How specializing kidney disease gives Jason a unique insight into early indications of illness [20:50]
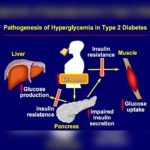
- Insulin resistance, hyperinsulinemia, and the overflow paradigm [29:30];
- Why the common treatments for type 2 diabetes seem to make things worse [42:30];
- How hyperinsulinemia (not insulin resistance) drives metabolic syndrome [53:15];
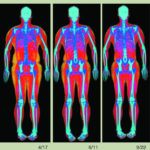
- Insulin and weight gain, and using fasting to empty the cells of glucose [59:30];
- The two step process of developing type 2 diabetes and how they are both manifestations of hyperinsulinemia [1:03:15];
- NAFLD and hyperinsulinemia: A vicious cycle [1:08:30];
- Are the features and symptoms of diabetes actually protective? [1:12:15];
- Is obesity causing insulin resistance or is it the other way around? [1:17:30];
- What role does inflammation play in obesity? [1:21:45];
- CVD and cancer: Diseases of too much growth? [1:27:30];
- How to reduce proliferation with rapamycin, nutrition, exercise, fasting, and manipulating hormones [1:32:45];
- Getting patients to fast: How Jason and Peter utilize fasting in their practice, and how their approach differs [1:40:15];
- Comparing bariatric surgery to fasting as a treatment for type 2 diabetes [1:48:00];
- Why people think that fasting is bad for you [1:55:15];
- Time-restricted feeding and intermittent fasting: Defining terms, and how Jason applies them in his practice [1:58:30];
- A fasting case study: A diabetic patient with a non-healing foot ulcer [2:04:00];
- Keys to a successful fast [2:12:45];
- Muscle loss during fasting, and why Jason isn’t worried [2:24:45];
- Will fasting help a healthy person live longer? [2:31:30];
- Does fasting cause gallstones? [2:38:45]; and
- More.
Comparing scientific disciplines: Medicine and biology versus physics [7:25]
What makes Jason’s perspective unique
- Peter says what distinguishes Jason from others who like to speak about the benefits (and risks) of fasting is that Jason is on the front lines treating patients
- Jason agrees, and adds that he’s only interested in what works ⇒ “You can talk all you want about this and that, but if it doesn’t change management, then it doesn’t interest me particularly.”
Physics
- Jason loves the approach to scientific progress in the realm of physics
- He really looks up to Richard Feynman (as does Peter), Einstein, and Niels Bohr
- “The way they do science is so much better than we do in medicine.”
- In physics, if the theory doesn’t agree with experimental evidence, you have to throw out the theory
- In medicine, bad theories tend to go round and round and round because they make sense, but nobody’s actually put them to the test
- In the case of insulin resistance… “the way we think about insulin resistance is sort of totally wrong and that’s why we have the sort of mess that we have”
Biology vs. physics
- Peter: “I’m generally suspect of people who have very, very strong points of view on things in biology or medicine who no longer interact with patients. Doesn’t mean that they’re wrong, but I’m generally suspect because of that.”
- Biology is harder than physics…. it’s just a lot messier
- Peter: “Every time I think I’ve really got it figured out, I’ll always meet a patient who proves me wrong.”
What Jason appreciates most about physics
- Many great theories (e.g., Newton)
- But then inevitably there are anomalies ⇒ “Anomalies are what drives sort of science forward because you have to come up with a better theory that explains the anomalies”
- Then you come up with a better theory which may have wild predictions but it could supplant the existing theory (i.e. Niels Bohr’s quantum theory supplanted Einstein)
- This doesn’t happen in medicine, says Jason… instead we have a super laborious process of evidence-based medicine
The limitations of evidence-based medicine [12:30]
Jason explains his frustrations…
- In medicine, we have a super laborious process
- We need evidence in order to move things forward
- Whereas physics moves at “light speed” because it doesn’t demand the sort of evidence base
- Evidence-based medicine is not a search for truth… it’s a search for consensus
- This approach makes things move glacially
⇒ For example, fasting…
{end of show notes preview…}

Jason Fung, M.D.
Dr. Jason Fung is a Canadian nephrologist who one of the most significant clinical practices that utilizes fasting for treatment of metabolic disease in Toronto, Canada.
He has written multiple best-selling books and he co-founded the Intensive Dietary Management program.
Dr. Fung graduated from the University of Toronto and completed his residency at the University of California, Los Angeles.


my name is Dr, Retta i am a veterinarian please tell me that the relationship between vomiting and diabetic.
Love your podcasts peter. Was introduced to you via the Joe Rogan interview. Subscribed to your podcasts and have been blown away with the new information I have discovered. First started with the A4M in functional medicine almost ten years ago and had a similar experience. It’s amazing how long I’ve been treating patients on my limited knowledge base taught in school, I’m hooked. As side note though, I almost exclusively listen in my car and can’t count the number of times a siren in your podcast has completely confused me searching for the EMS vehicle in my real time, lol. Thanks
While fasting, should I continue vitamins? Or wait 3 days to take? Thank you. Love the podcasts.
Curious how phlebotomy / iron reduction, has been shown to treat insulin resistance, and insulin resistance is found in those with increased red blood cells, and increased red blood cells are also treated by phlebotomy?
“Our findings provide in vivo evidence of a relation between hyperinsulinaemia/insulin resistance, the main variables of insulin resistance syndrome and erythropoiesis. Increased red blood cell count could be considered as a new aspect of the insulin resistance syndrome that could contribute to the increased risk of developing cardiovascular problems.”
https://pubmed.ncbi.nlm.nih.gov/11692171/
“Reduction of the body iron stores can improve hyperandrogenemia and insulin resistance.”
“Effect of phlebotomy”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6716867/
Re-listening in late 2020, and Jason’s not answering Peter’s queries about hyperinsulemia possibly damaging the macro vasculature.
great interview, but I don’t buy the “overflow paradigm” re “… we use sulfonylureas and exogenous insulin trying to shove more glucose into this already filled cell” b/c when my blood glucose (BC) surges to >180 after a high GI meal I’ll do some short weight lifting exercise that gets my muscle a bit tired and heart rate up and my glucose reading will immediately drop to 16 hrs my BC drops to ~80 and all my muscles feel lethargic, no energy, and gets dangerous if I don’t eat some high GI food fast. So, if my my muscle cells were already over filled w/ glucose then when would adding more glucose give me energy on the hypoglycemia BC and how would non-insulin intake pathways induced by exercise be possible on the hyperglycemia BC drop observed?
I have been fasting for many years. Until recently I was doing 40 day water fasts. After each time I fasted I saw weight loss, generally about 40 pounds, but I also saw roughly a 20% increase in my eyesight, hearing, sense of smell, and flexibility.
Each time I fast I remove all caffeine for two weeks before I begin. This is because caffeine has a push on the endocrine system. Removing this push allows more healing. This means that if you smoke, that should be removed for two weeks before fasting too, and for the same reason.
After 2020 with all of the stay at home, etc… I lost sight of my health goals altogether. I realized on January 1 of 2021 that I was at my heaviest weight of my life. I started the year at 283 pounds. I changed my plan to fast for the first three weeks of each month. After each week of fasting I do a saline flush to remove the buildup of poisons. After the full three weeks I do a vegetarian high protein diet for the remainder of the month. On the last day I have one cheat meal. I then start the cycle again the following month.
By the end of my fasting period in March I was down almost 60 pounds. I am about to start it again for April. I am feeling SO MUCH BETTER! Given that this is a repeatable solution I plan to continue to do this until I experience a full body reset.