When I wrote part I of this post, I naively assumed this would only be a two-part series. However, so many great questions and comments emerged from the discussion that I realize it’s worth spending much more time on this important and misunderstood topic. In terms of setting expectations, I suspect this series will require at least four parts.
So, back to the topic at hand…. (You may want to read or maybe reread part I for a biochemistry refresher before diving into part II.)
Is there a “metabolic advantage” to being in ketosis?
Few topics in the nutrition blogosphere generate so much vitriolic rhetoric as this one, and for reasons I can’t understand. I do suspect part of the issue is that folks don’t understand the actual question. I’ve used the term “metabolic advantage” because that’s so often what folks write, but I’m not sure it has a uniform meaning, which may be part of the debate. I think what folks mean when they argue about this topic is fat partitioning, but that’s my guess. To clarify the macro question, I’ve broken the question down into more well-defined chunks.
Does ketosis increase energy expenditure?
I am pretty sure when the average person argues for or against ketosis having a “metabolic advantage” what they are really arguing is whether or not, calorie-for-calorie, a person in ketosis has a higher resting energy expenditure. In other words, does a person in ketosis expend more energy than a person not in ketosis because of the caloric composition of what they consume/ingest?
Let me save you a lot of time and concern by offering you the answer: The question has not been addressed sufficiently in a properly controlled trial and, at best, we can look to lesser controlled trials and clinical observations to a make a best guess. Believe me, I’ve read every one of the studies on both sides of the argument, especially on the ‘no’ side, including this one by Barry Sears from which everyone in the ‘no’ camp likes to quote. This particular study sought to compare a non-ketogenic low carb (NLC) diet to a ketogenic low carb (KLC) diet (yes, saying ‘ketogenic’ and ‘low carb’ is a tautology in this context). Table 3 in this paper tells you all you need to know. Despite the study participants having food provided, the KLC group was not actually in ketosis as evidenced by their B-OHB levels. At 2-weeks (of a 6-week study) they were flirting with ketosis (B-OHB levels were 0.722 mM), but by the end of the study they were at 0.333 mM. While the difference between the two groups along this metric was statistically significant, it was clinically insignificant. That said, both groups did experience an increase in REE: about 86 kcal/day in the NLC group and about 139 kcal/day in the KCL group (this is calculated using the data in Table 3 and Table 2). These changes represented a significant increase from baseline but not from each other. In other words, this study only showed that reducing carbohydrate intake increased TEE but did not settle the ‘dose-response’ question.
This study by Sears et al. is a representative study and underscores the biggest problems with addressing this question:
- Dietary prescription (or adherence), and
- Ability to accurately measure differences in REE (or TEE).
Recall from a previous post, where I discuss the recent JAMA paper by David Ludwig and colleagues, I explain in detail that TEE = REE + TEF + AEE.
Measuring TEE is ideally done using doubly-labeled water or using a metabolic chamber, and the metabolic chamber is by far the more accurate way. A metabolic chamber is a room, typically about 30,000 liters in volume, with very sensitive devices to measure VO2 and VCO2 (oxygen consumed and carbon dioxide produced) to allow for what is known as indirect calorimetry. The reason this method is indirect is that it calculates energy expenditure indirectly from oxygen consumption and carbon dioxide production rather than directly via heat production. By comparison, when scientists need to calculate the energy content of food (which they do for such studies), the food is combusted in a bomb calorimeter and heat production is measured. This is referred to as direct calorimetry.
Subjects being evaluated in such studies will typically be housed in a metabolic ward (don’t confuse a metabolic ward with a metabolic chamber; the ward is simply a fancy hospital unit; the chamber is where the measurements are made) under strict supervision and every few days will spend an entire 24 hour period in one such chamber in complete isolation (so no other consumption of oxygen or production of carbon dioxide will interfere with the measurement). This is the ‘gold standard’ for measuring TEE, and shy of doing this it’s very difficult to measure differences within about 300 kcal/day.
Not surprisingly, virtually no studies use metabolic chambers and instead rely on short-term measurement of REE as a proxy. In fact, there are only about 14 metabolic chambers in the United States.
A broader question, which overlays this one, is whether any change in macronutrients impacts TEE.
Despite the limitations we allude to in the summary of this review, there is a growing body of recent literature (for example this study, this study, and this study) that do suggest a thermogenic effect, specifically, of a ketogenic diet, possibly through fibroblast growth factor-21 (FGF21) which increases with B-OHB production by the liver.
These mice studies (of course, what is true in mice isn’t necessarily true in humans, but it’s much easier to measure in mice) show that FGF21 expression in the liver is under the control of the transcription factor peroxisome proliferator-activated receptor a (PPARa), which is activated during starvation. Increased FGF21 promotes lipolysis in adipose tissue and the release of fatty acids into the circulation. Fatty acids are then taken up by the liver and converted into ketone bodies. FGF21 expression in liver and adipose tissue is increased not only by fasting but also by a high fat diet as well as in genetic obesity which, according to these studies, may indicate that increased FGF21 expression may be protective. Hence, ketosis may increase TEE either by increasing REE (thermogenic) or AEE (the ketogenic mice move more). Of course, this does not say why. Is the ketogenic diet, by maximally reducing insulin levels, maximally increasing lipolysis (which dissipates energy via thermogenic and/or activity ‘sinks’) or is the ketogenic diet via some other mechanism increasing thermogenesis and activity, and the increased lipolysis is simply the result? We don’t actually know yet.
Bottom line: There is sufficient clinical evidence to suggest that carbohydrate restriction may increase TEE in subjects, though there is great variability across studies (likely due the morass of poorly designed and executed studies which dilute the pool of studies coupled with the technical difficulties in measuring such changes) andwithin subjects (look at the energy expenditure charts in this post). The bigger question is if ketosis does so to a greater extent than would be expected/predicted based on just the further reduction in carbohydrate content. In other words, is there something “special” about ketosis that increases TEE beyond the dose effect of carbohydrate removal? That study has not been done properly, yet. However, I have it on very good authority that such a study is in the works, and we should have an answer in a few years (yes, it takes that long to do these studies properly).
Does ketosis offer a physical performance advantage?
Like the previous question this one needs to be defined correctly if we’re going to have any chance at addressing it. Many frameworks exist to define physical performance which center around speed, strength, agility, and endurance. For clarity, let’s consider the following metrics which are easy to define and measure
- Aerobic capacity
- Anaerobic power
- Muscular strength
- Muscular endurance
There are certainly other metrics against which to evaluate physical performance (e.g., flexibility, coordination, speed), but I haven’t seen much debate around these metrics.
To cut to the chase, the answers to these questions are probably as follows:
- Does ketosis enhance aerobic capacity? Likely
- Does ketosis enhance anaerobic power? No
- Does ketosis enhance muscular strength? Unlikely
- Does ketosis enhance muscular endurance? Likely
Why? Like the previous question about energy expenditure, addressing this question requires defining it correctly. The cleanest way to define this question, in my mind, is through the lens of substrate use, oxygen consumption, and mechanical work.
But this is tough to do! In fact, to do so cleanly requires a model where the relationship between these variables is clearly defined. Fortunately, one such model does exist: animal hearts. (Human hearts would work too, but we’re not about to subject humans to these experiments.) Several studies, such as this, this, and this, have described these techniques in all of their glorious complexities. To fully explain the mathematics is beyond the scope of this post, and not really necessary to understand the point. To illustrate this body of literature, I’ll use this article by Yashihiro Kashiwaya et al.
The heart is studied because the work action is (relatively) simple to measure: cardiac output, which is the product of stroke volume (how much blood the heart pumps out per beat) and heart rate (how many times the heart beats per minute). One can also measure oxygen consumption, all intermediate metabolites, and then calculate cardiac efficiency. Efficiency increases as work increases relative to oxygen consumption.
Before we jump into the data, you’ll need to recall two important pieces of physiology to “get” this concept: the acute (vs. chronic) metabolic effect of insulin, and the way ketone bodies enter the Krebs Cycle.
The acute metabolic effects of insulin are as follows:
- Insulin promotes translocation (movement from inside the cell to the cell membrane) of GLUT4 transporters, which facilitate the flux of glucose from the plasma into the inside of the cell.
- Insulin drives the accumulation of glycogen in muscle and liver cells, when there is capacity to do so.
- Least known by most, insulin stimulates the activity of pyruvate dehydrogenase (PDH) inside the mitochondria, thereby increasing the conversion of pyruvate to acetyl CoA (see figure below).
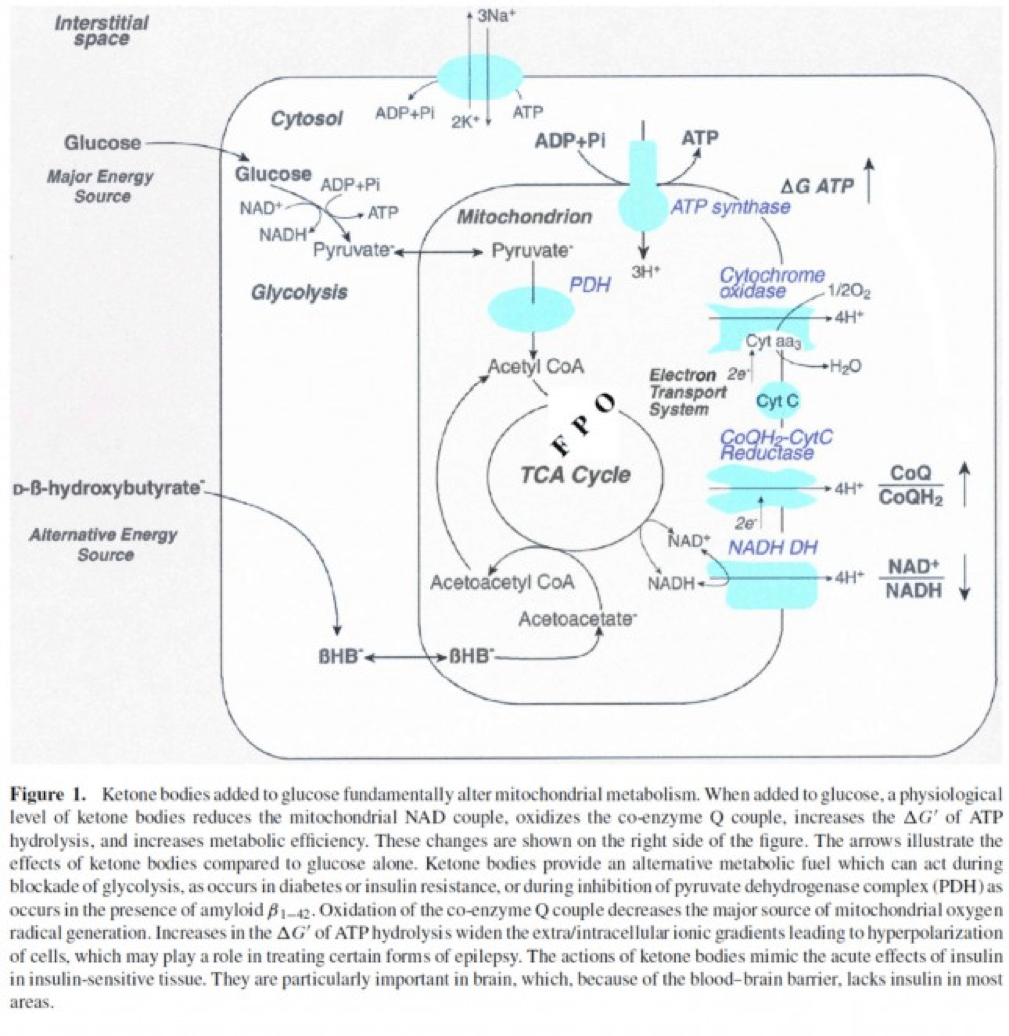
The second important point to recall is that ketone bodies bypass this process (i.e., glucose to pyruvate to acetyl CoA), as B-OHB enters the mitochondria, converts into acetoacetate, and enters the Krebs Cycle directly (between succinyl CoA and succinate, for any biochem wonks out there). I keep alluding to this distinction for a reason that will become clear shortly.
An elegant way to test the relative impact of glucose, insulin, and B-OHB on muscular efficiency is to “treat” a perfused rat heart under the following four conditions:
- Glucose alone (G)
- Glucose + insulin (GI)
- Glucose + B-OHB (GK)
- Glucose + insulin + B-OHB (GIK)
In fact, that’s exactly what this paper did. Look at what they found:
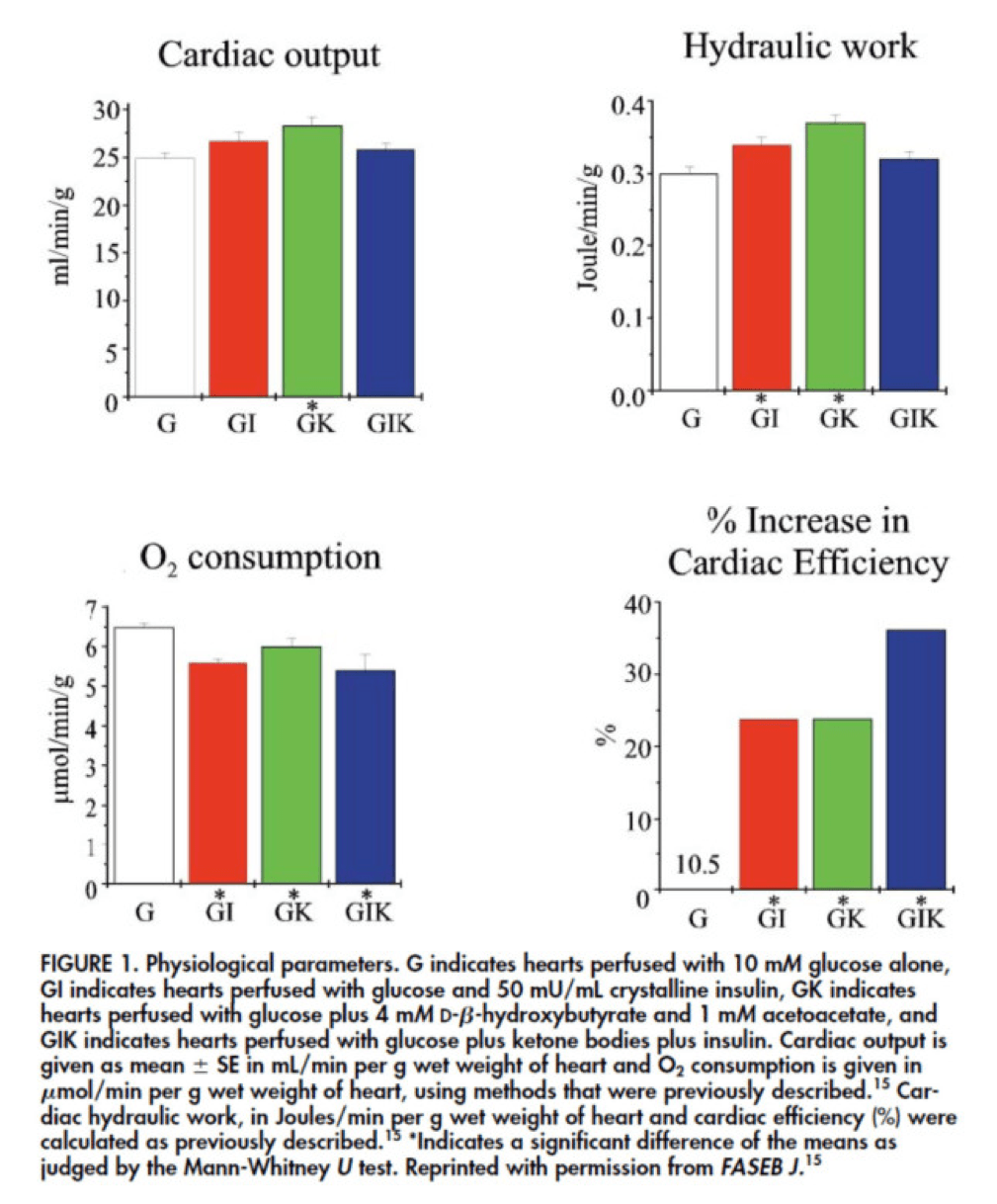
The upper two graphs in this figure show similar information, namely the response of cardiac output and hydraulic work to each treatment. (Cardiac output is pure measurement, as I described above, of volume of blood displaced per unit time. Hydraulic work is a bit more nuanced; it measures the mechanical work being done by the fluid.)
Adding insulin to a fixed glucose (GI) load increases both cardiac output and hydraulic work, but it’s only significant in the case of hydraulic work. Conversely, adding B-OHB to glucose (GK) increases both cardiac output and hydraulic work significantly. Interestingly, combining insulin and B-OHB with glucose (GIK) increases neither.
Oxygen consumption was significantly reduced in all arms relative to glucose alone, so we expect the cardiac efficiency to be much higher in all states. (Why? Because for less oxygen consumption, the hearts were able to deliver greater cardiac output and accomplish greater hydraulic work.)
The figure on the bottom right shows this exactly. If you’re wondering why the gain in efficiency is so great (24-37%), the answer is not evident from this figure. To understand exactly how and why adding high amounts of insulin (50 uU/mL) or B-OHB (4 mM) to glucose (10 mM) could cause such a step-function increase in cardiac efficiency, you need to look specifically at how the concentration of metabolic intermediates (e.g., ATP, ADP, lactate) varied in the rat heart cells.
This is where this post goes from “kind of technical” to “really technical.”
The figure below presents the results from this analysis. The height of the bar shows the fold-increase for each of the three treatments relative to glucose alone. To orient you, let’s look at a few examples. In the upper left of the figure you’ll note that GI and GIK both significantly increase glucose concentration in the cell, while GK does not. Why? The GI and GIK treatments both increase the number of GLUT4 transporters translocated to the cell surface so more glucose can flux in. GK does increase glucose concentration, but not significantly (in the statistical sense).
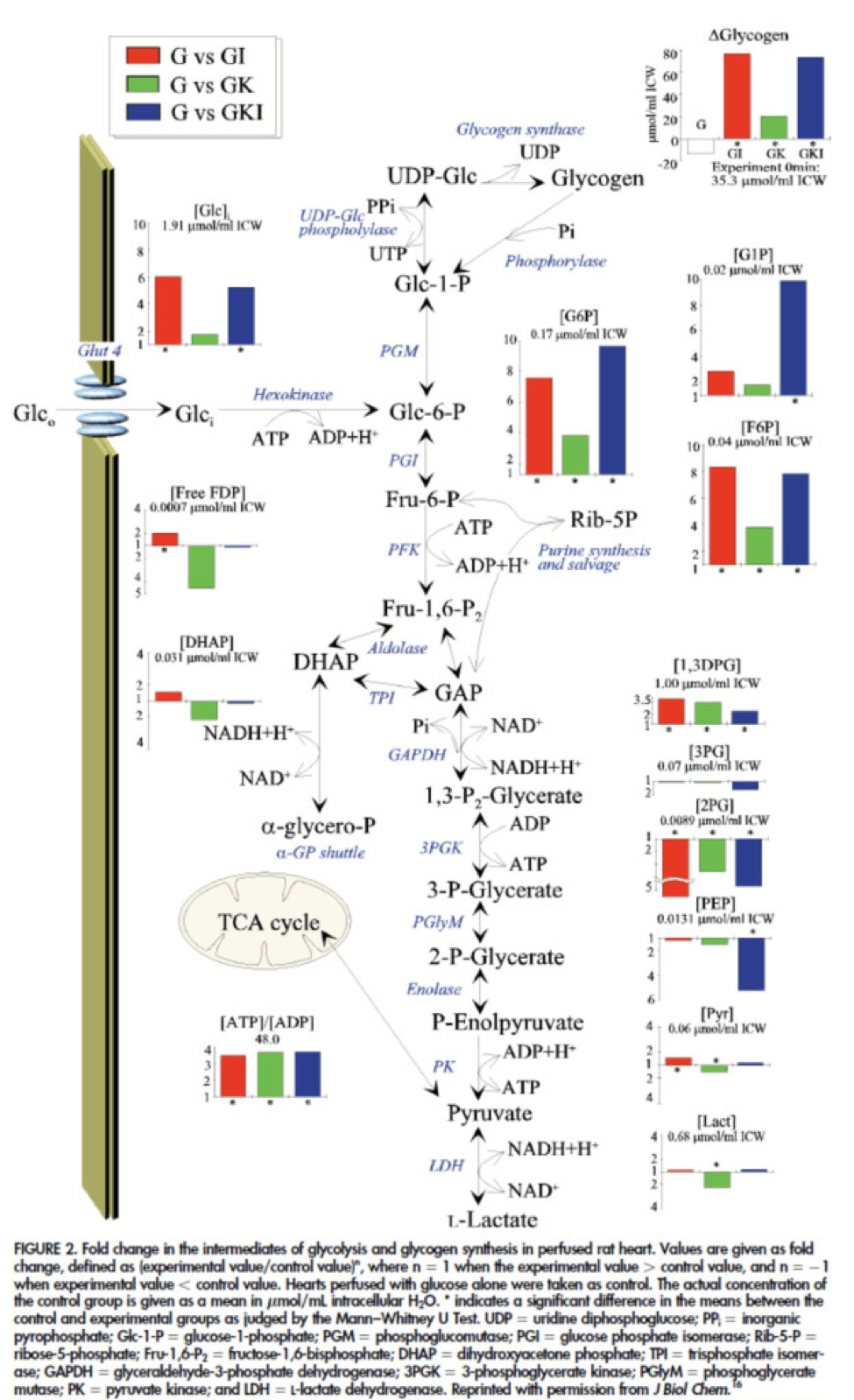
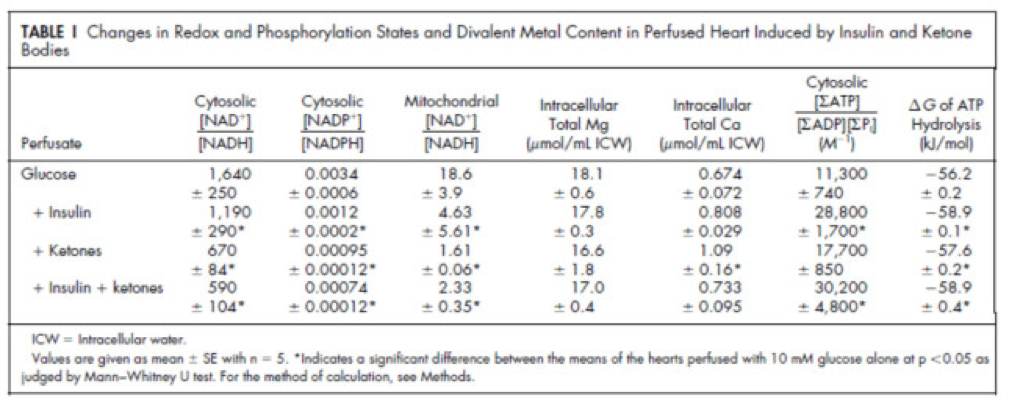
Table 1 from this paper, below, summarizes the important changes from this analysis. In particular, look at the last column, the Delta G of ATP hydrolysis.
I was really hoping to write this post without ever having to explain Delta G, but alas, I’ve decided to do it for two reasons:
- To really “get” this concept, we can’t avoid it, and;
- The readers of this blog are smart enough to handle this concept.
Delta G, or Gibbs free energy, is the “free” (though a better term is probably “available” or “potential”) energy of a system.
Delta G = Delta H – Temperature * Delta S, where H is enthalpy and S is entropy. The more negative Delta G is, the more available (or potential or “free”) energy exists in the system (e.g., a Delta G of -1000 kcal/mol has more available energy than one of -500 kcal/mol). To help with the point I really want to make I refer to you this video which does a good job explaining Gibbs free energy in the context of a biologic system. Take a moment to watch this video, if you’re not already intimately familiar with this concept.
Now that you understand Delta G, you will appreciate the significance of the table above. The Gibbs free energy of the GI, GK, and GIK states are all more negative than that of just glucose. In other words, these interventions offer more potential energy (with less oxygen consumption, don’t forget, which is the really amazing part).
To see what the substrate-by-substrate changes look like across the mitochondria and ETC, look at this figure:
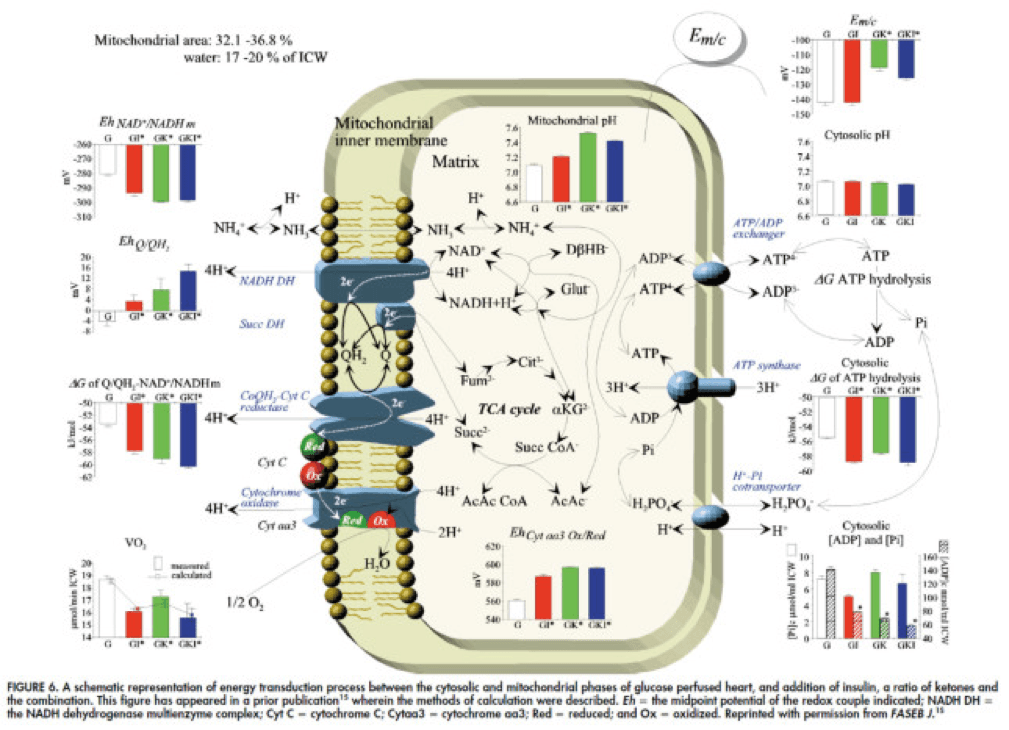
Though it is by no means remotely obvious, what is happening above boils down to two major shifts in substrate utilization:
- In one step the reactants NADH/NAD+ become more reduced (in the chemical sense), and;
- In another step the reactants CoQ/CoQH2 become more oxidized (in the chemical sense).
These changes, taken together, widen the energetic gap between the states and, in turn, translates to a higher (i.e., more negative) Delta G which translates to greater ATP production per unit of carbon.
Additional work, which you’ll be delighted to know I will not detail here, in fact shows that on a per carbon basis, B-OHB generates more ATP per 2-carbon moiety than glucose or pyruvate. As an aside, this phenomenon was first described in 1945 by the late Henry Lardy, who observed that sperm motility increased in the presence of B-OHB (relative to glucose) while oxygen consumption decreased!
Is there a reason to prefer GK over GI?
Yes. Recall that ketones make their way onto the metabolic playing field without going through PDH. Adding more insulin to the equation forces more pyruvate towards PDH into acetyl CoA. While B-OHB “mimics” the effect of additional insulin, it does so in a much cleaner fashion without the complex cascade of events brought on by additional insulin (e.g., decreased lipolysis) and, perhaps most importantly, avoids the logjam of impaired PDH due to insulin resistance (I’ll come back to this point in a future post when I address Alzheimer’s disease and Parkinson’s disease). In essence, B-OHB “hijacks” the Krebs Cycle via a slick trick that lets it bypass the bottleneck, PDH. All the glucose and insulin in the world can’t overcome this bottleneck. It’s truly a privileged state and a remarkable evolutionary trick that we can utilize B-OHB.
Back to the original question…
Clearly, in the highly controlled setting of a perfused rat heart, ketones offer an enormous thermodynamic advantage (28%!). But what about in aggregate human performance? There is no reason to believe that therapeutic levels of B-OHB (either through nutritional ketosis or by ingesting ketone esters) would increase anaerobic power, since the anaerobic system does not leverage the Delta G improvement I’ve outlined here. Same is true for muscular strength. However, there is reason to believe that aerobic capacity and muscular endurance could be improved with sufficient B-OHB present to compliment glucose.
It turns out this has been demonstrated repeatedly in subjects ingesting ketone esters, developed by Dr. Richard Veech (NIH) and Dr. Kieran Clarke (Oxford). Because the results of their work have not yet been published, I can’t comment much or share the data I have, which they shared with me. I can say the ingestion of B-OHB in the D-isoform (the physiologic isoform), resulting in serum levels between 4 and 6 mM, did lead to significant increases in aerobic power and efficiency in several groups of elite athletes (e.g., Olympians) across multiple physical tasks maximally stressing the aerobic system.
Once published, I believe these studies will be a real shot across the bow of how we view athletic performance. It is very important to point out, however, that these studies don’t exactly address the most relevant question, which has to do with nutritional ketosis. In other words, ingesting ketone esters to a level of 4 to 6 mM might not be the same as de novo producing B-OHB to those levels. But, such trials should be forthcoming in the next few years. Personally, I am most eager to see the results of a ketone ester alone versus nutritional ketosis versus combination treatment, all to the same serum level of B-OHB.
The Hall Paradox
For the really astute readers, you may be saying, “Waaaaaaaait a minute, Peter…if ketones increase Gibbs free energy while reducing oxygen consumption, should this imply TEE goes down?” You’re right to ask this question. It was the first question I asked when I fully digested this material. If each molecule of B-OHB gives your muscles more ATP for less oxygen, you should expend less not more energy at the same caloric intake, right?
I was discussing this with Kevin Hall at NIH, an expert in metabolism and endocrinology. Kevin pointed out the error in my logic. I failed (in my question) to account for the energetic cost of making the ketones out of fat. Remember, in the experiments described above, the B-OHB is being provided for “free.” But physiologically (i.e., in nutritional ketosis or even starvation), we have to make the B-OHB out of fat. The net energy cost of doing this is actually great. According to Kevin, it is not generally appreciated how making ketones from fatty acids affects overall energy efficiency. Nevertheless, this can be examined by comparing the enthalpy of combustion of 4.5 moles of B-OHB, which is about -2,192 kcal, with the enthalpy of combustion of 1 mole of stearic acid (about -2,710 kcal) that was used to produce the 4.5 moles of ketones. Thus, there is about 20% energy loss in this process. Hence, the energy gain provided by the ketones is actually less than the energy cost of making them, at least in theory.
This suggests that being in nutritional ketosis may require more overall system energy, while still increasing work potential. In other words, a person in nutritional ketosis may increase their overall energy expenditure, while at the same time increasing their muscular efficiency. In honor of Kevin, I refer to this as the Hall Paradox.
Parting shot
Ok, if you’re still reading this, give yourself a pat on the back. This was a bit of chemistry tour de force. Why did I do it? Well, frankly, I’m tired of reading so much nonsense on this topic. Everybody with a WordPress account (and countless people without) feels entitled to spew their opinions about ketosis without even the slightest clue of what they are talking about. As I said in part I of this series, there is no bumper sticker way to address this question, so to say ketosis is “good” or “bad” without getting into the details is as useful as a warm bucket of hamster vomit (unless you’re Daniel Tosh, in which case I bet you can find a great use for it).
Next time, I’ll try to back it out of the weeds and get to more clinically interesting stuff. But we had to do this and we’re better for it.
Chemistry by Marcin Wichary is licensed under CC by 2.0




I got lazy and stopped the bouillon. And I’ve been eating some “bad” foods – a half cup or so of rice, a little sweet potato occasionally. I’ve actually dropped a few pounds (I’m 57 and cannot be slim – I’m 5′ 1″ and probably weigh about 133; my top weight was about 215 25 years ago) and feel better than I have in a long time – more energy. I have no idea why! Anyway, I keep telling myself to drink the bouillon, but then don’t… on the other hand, I eat processed turkey and canned salmon almost daily, so maybe I get enough salt there. I know – processed = bad. I hate to cook. 🙂
Hey Peter, I have been doing ketosis diet on and off for about 2 years. I am currently in medical school and it is funny to debate with people why I do and the benefits. I have done labs twice one control and one about 6 months ago. They were very similar to yours. I used to play college football and was, at my highest was 315 lbs. Granted I was very strong and athletic. This diet was the only way for me to get down to my current weight of about 225 lbs. I do still like to lift weights, very heavy at some times. I do mild cardio most days. My question to you is pre-workout/intraworkout supplements and their effects on ketosis. I usually go to the gym in a fasted state, but cant seem to find any information online as to whether pre-workout drinks with the normal creatine and BCAAs will hinder the benifits of ketosis and fasted state exercise.
Zac, I use BCAA (about 5 or 6 gm) in-workout (otherwise fasted), then about 5-6 gm glutamine + 25 gm whey post-workout. This does not appear to hinder my ketosis, per se. The actual HIIT is probably doing most of the transient hindering due to marked HGO.
Hi Peter,
Are you currently below 50g of carbs or did you permanently increase it above 50g? Why do you not use MCT oil anymore? Is there a reason why you keep high monounsaturated fats?
Yes, well below. Probably 20 gm/day. Just stopped using MCT and it made no difference. Maybe carbs and protein are low enough now (ketosis, round 2) that I don’t need the kick-start.
Peter I noticed that you stopped taking MCT oil…can you share the reason why?
See previous response.
I’m not sure I’m understanding this correctly, so my question may be hopelessly naive. The Hall Paradox (I think) says that burning B-OHB is more efficient than glucose but that making B-OHB is less efficient than making glucose. So my question is: how long can you exercise before you burn through the already circulating (or stored?) B-OHB and have to start making more. How long does an exercise session have to be before the extra energy cost of making B-OHB makes it less efficient than glucose (overcoming the extra efficiency of burning the already circulating B-OHB)?
Almost right. B-OHB, when oxidized, gives more ATP per unit O2 than glucose. But we get glucose for “free” (we eat it). We need to make B-OHB out of our fat, that costs us energy. To answer the question, pretty soon. Our plasma amount of glucose or B-OHB gets used up very quickly when we’re exercising, so we quickly turn to the liver to give us more of both.
Hi Peter,
Thanks for all the articles. To be completely honest, most of the technical information goes over my head but I get the general idea. I have been on a ‘cold turkey’ <50 carbs a day for about a week now. It has been difficult as I'm still swimming 2.5km about 7-8 times a week so doing this with headaches and some nausea has been difficult. I am starting to have a bit more energy so hopefully I’m getting towards the end of the worst… I am battling to find resources on the web that give example diets and I’m struggling to lower my protein intake. I’m also struggling with how to increase my fat intake. A lot of searches for low carbs diets seem to point to information that contradicts a lot I hear here and so I can’t take the rest of that site seriously. I have my own criteria for who i believe on facts – If the person is prepared to admit they are wrong if presented with real evidence to the contrary then I am more likely to believe what they say. People like you, Gary Taubes & Prof Noakes fall into this category. In the coming months, I am going to start increasing my swim distances so if anyone can help out with info on increasing my fat intake as well as feeding around the swim, I would appreciate it. (I would love to get my hands on some UCAN Superstarch, but unfortunately this is not available in the UK)
David, Check with the UCAN company. I do believe they can ship to the UK. It may be worth trying a more gradual approach to your dietary intervention, versus a dramatic shift to ketosis. Take a look back at my path to ketosis in 2009-2011. Very slow and gradual…
Hi there,
My path to ketosis was quite fast (2-3 weeks) after eliminating most high carbs food (grains / sugar / starches). My fat intake increased quite a lot (fat cheeses, oil, butter / ghee, lard, etc).
BUT, I knew I would feel a bit funny during the transition so I did NOTHING at all in terms of physical activity. I waited for about 1 month before being active (cycling, hiking for hours, etc). Note that I do not try to be the fittest, strongest, most endurance hardened person in the world, I just want to have fun and feeling all the energy I feel today allows me that. If I were you, I would stop the swim for 2-3 weeks. I know you will probably think that you are slacking off, or whatever, but changing your metabolism from sugar burning to fat burning is too big a change and your body will surely be “fatigued” during the transition.
Peter,
1 more question about MCT. I see you stopped taking it. Have you stopped ingesting Coconut Oil as well?
KC
No, still cook with it.
Hi Peter,
I’m sorry to hear about your friend Woody.
It will be really interesting to see the data from the study by Veech & Clarke. From personal experience I feel most ‘energised’ when I wake up in the morning after not having eaten for >11h. I would expect my ketone levels to be the highest (I don’t have a device for measuring them) at this time of day.
Have you ever tested this yourself by performing the same type of exercise with (statistically significantly) different ‘starting’ ketone levels?
Keep up the good work!
Peter,
This information came at a pretty convenient time.
I recently had blood work done for a physical and my liver enzymes were elevated (AST=41;ALT=86) so that caused my physician to be concerned.
I recalled this series as well as the physician being surprised at how my ketone level was and thought to myself that my liver enzymes could be elevated because my ketone production is high (I’m also sure the multiple shots of tequila as well as some wine that I had on Saturday night did not help either!). I tried looking through your diagrams for ALT/ALS and couldn’t find anything. A wiki search however revealed that ALT is used to produce alpha-ketoglutarate.
This leads me to believe that my initial guess was correct in that liver enzymes were elevated due to:
1) fat adapted –> high ketone production –> high alpha-ketoglutarate –> high ALT/ALS
2) high alcohol intake 36 hours prior to the test (note: I do not regularly drink heavily)
Is my understanding correct?
Thanks again for all of the information you provide at this site.
Now that I think about it a little more I’m going to eliminate (1) as a possible cause and leave it just as (2).
From studying your diagram more it appears that AST/ALT are only used in Glucose-CoA pathway and not the the Fat-CoA chain. This leads me to conclude that (1) is not possible. I think it is much more likely that the high AST/ALT levels were from the alcohol consumption I had less than 36 hours prior to the test.
I also forgot to consider that my ketone levels were from a urine sample I took today and not at the time the blood was drawn (Monday). Therefore case (1) falls apart completely.
Please let me know if this is correct.
Thanks again.
….forgot one other crucial thing.
<36hours before the test I consumed almost an entire Chocolate Wall of Cake (376carbs) from PF Chang's. Certainly not my proudest moment.
I think I know why my liver enzymes were elevated….
Interesting hypothesis. I, too, had mild elevation of AST and ALT for about 6 months. All better now, so hard to say. Could have been a viral infection, could have something else. But, as you point out, could have part of the adaptation. Just had a liver MRI 2 days that showed zero fat in my liver.
Your site, although technical is very accessible to non scientists like myself, many thanks for all the information. One question not specifically addressed is why some indivuals become insulin resistant, while others don’t? Having been pretty skinny all my life I rapidly gained weight after surgery to remove my ovaries, so in my case it would appear to be hormone related. Staying low carb has fixed this and I now maintain easily at 65 kg 169.5 cm tall. But I don’t understand why one of my sons (aged 42) is obese, now thankfully starting a low carb diet, whilst the other remains very slim (aged 30) whilst apparently consuming refined carbohydrates and high sugar sodas? In spite of eating all the wrong things, there do seem to be individuals who remain slim throughout their lives, are you able to shed any light on why this might be the case?
Hard to make a case that hormones aren’t playing a role, huh?
i agree some people appear to be able to eat anything and remain thin.
not specifically healthy but thin.
i have read in various artilcles that around 25 percent of people have the ability to break down or use the carbs in a more efficicent way then the 75 percent majority.
although health and weight are connected i do not see all thin people as healthy people. fit and thin are not the same.
Important distinction, of course. Just because one is thin doesn’t mean healthy. 7-10% of adults who are normal or underweight have MetSyn. “Only” 65% of obese adults have MetSyn. Best to focus on metabolic health, rather than weight. My TED talk in April will focus on this.
Hi Peter
Just came across your site, although I have seen your interview on Youtube. I have been low carb for the past 4-5 months and am now at a below 50g Carb level per day. I am a 50 year old competitive runner and must say that my energy levels are so high now. I am absolutely flying in training and fully expect, not only to set Age PR’s, but absolute PR’s this year from 5k upwards. I am convinced this lifestyle is the way to go.
At last nights club 8 mile tempo run I nailed my previous best time by 40 secs in a much easier effort level than the previous time. I even ran my son close and he is a 33 min 10k guy. I do feel sort of buzzy, in a hightened state for want of a better word and not sure if this a symptom of ketosis. Even my 20 mile long runs I can do without any fuelling and do not see any detriment at all.
Great site and keep up the good work. This message needs to get out.
Kind Regards
Nick Jones
Barton-Le-Clay
Beds
United Kingdom
Very exciting. Thanks for sharing, Nick.
Peter,
Thank you so much for your work and blogs. I have my doctorate in sports nutrition, and never during my education was I even introduced to this topic of nutritional ketosis and performance implications. You and others like Taubes, Sisson and Volek have really flipped the world that I have known upside down- I like it. I’m currently completing my dietetic internship to become a registered dietitian and once again low-carb, high-fat eating is almost viewed as blasphemy by most. I, however look forward to speaking out and supporting these concepts within the professional nutrition community.
I do have a question for you regarding sport performance. I provide a lot of nutrition education to teen and professional ballet dancers. These athletes require power for short aerobic stints (no more than 5-minutes of consistent activity, but potentially 6 or more hours of this on and off throughout the day) as well as anaerobic power for large jumps/partnering, etc (similar to gymnasts). They need endurance capabilities which makes me feel like a lower carbohydrate diet would benefit them. A lot of them also constantly struggle with maintaining the low body weights often required (dancers actually don’t burn many calories, and are taught to eat moderate/high carb to fuel their activity. Very low calorie diets are usually what they succumb to and as a result their metabolic rates are significantly depressed and the female athlete triad comes into play). Like I mentioned before, however dancers do need to tap into their max efforts. I noticed in one of your blogs that ketosis negatively affected your top-end power. I bet dancers challenge their VO2max multiple times a day. I’ve also read in your blog, however, that you have no issues with intense resistance training (I can’t see tire flipping being much easier than what they are doing ?) So, I’m wondering: do you think a low-carb diet would benefit this type of athlete in a non-steady state/high-intensity type of activity or would it detract from their top-end performance capabilities? If a dancer isn’t quite ready to get into nutritional ketosis, but I urge them to reduce their carb intake (say to 100-150 grams as Mark Sisson suggests) would this be helpful or put them into a mid-zone that only hinders them? Prior to all of my recent readings, I recommended (via conventional wisdom) complex carbs for breakfast, a pre-activity higher carb/low fat/moderate protein snack and then of course, the post-activity recovery snack of carb/protein (3:1). Now, I wonder if I am doing them a disservice. With this recommendation they can’t up their caloric intake and continue their battle with weight and other health concerns. Thanks so much for your insights.
Interesting question. I just saw this paper last month. Don’t recall who sent it to me, but it seems to try to address your question:
https://www.jissn.com/content/9/1/34
Hi Peter,
In that they consume 2.8g protein/kg which seems rather high (even though they say it’s to preserve lean muscle mass). I would think that 2g protein/kg was closer to the upper limit.
Have you seen any studies on how much protein one can eat without going out of ketosis? How much is gluconeogenesis related to absolute body weight vs. an absolute of protein? I’m thinking that a fixed amount of protein will have a more negative effect for a lighter person compared to a heavier.
If I may ask, how many grams of protein per kg/lbs of body weight do you aim for?
Br,
Hemming
It’s probably a function of timing of protein ingestion and anabolic need. I aim for about 120 gm/day, but with very special attention to when I consume it.
Hi,
I am patiently waiting for the next in the ketosis series- specifically, a nuanced explanation of what to eat to get (and stay) there! I have an extremely hard time keeping protein levels down. I know that I probably need to increase the fat quite a bit, but I just can’t seem to get there. I always end up eating more and more protein to get that “full” feeling, but have realized that I’m probably eating almost 200g of protein a day- and I’m a 5’4″ woman.
I guess I’m hesitant to up the fat so much because I’m still mentally tracking calories in my head (I know, I know, but old habits die hard). I’m concerned that I will just keep upping the calories with fat but not really feel satisfied.
I’ve tried upping fats “independently” of meat before (lots of EVOO on salad, MCT oil, etc.) with no success in terms of satiety. My new approach is to eat only fatty cuts of meat and moderate added fats.
Have you heard of this issue before? I’ve been LC for a year or so, but haven’t succeeded with ketosis at all.
Thanks!
One more thing:
For a 5’4″ woman weighing around 120 pounds, what would ideal ratios (on average) look like? Reading through comments, I see people eating anywhere from 50-150 grams of protein daily- I seem to remember you saying less than 150 would achieve ketosis (generally) as long as carbs are under 50g.
Sorry to be so nitpicky- I’m just anxious to get it all “dialed” in….
Will discuss later in this series. You’ll want to hear the full story before you decide to dial in.
J — you may want to wade through these threads
https://www.marksdailyapple.com/forum/thread73597.html
https://www.marksdailyapple.com/forum/thread65113.html
There are several discussions of what numbers to use. Personally, at 5’1″ (155cm) my goal weight (age 61 – postmenopausal by several years) is 110-120 (50-54kg). I use 50-55g protein, 25-28g carb, and the rest is fat (from a combination of diet and current stores). This works for me. Some folks split the protein into multiple meals, some do one meaty meal per day. There’s a lot of finding what works for you in these threads.
Peter,
Can you talk a little bit more about the LC/NK impact on the urine data ? Jimmy Moore just posted his urine test results, 3+ protein, rbc presented in the urine, plus calcium oxalate crystal, cloudy and foamy urine, high specific gravity, all pointing to some sort of Kidney damages. Is it caused by lower carb intake or higher protein intake ? You know Jimmy is doing LC/NK for years.
Kang
I’m not familiar with Jimmy’s urine data and am not in a position to comment on it.
Peter,
I was curious to see what you thought about Berberine, specifically what is mentioned on this site:
https://examine.com/supplements/Berberine/
I’m not familiar with it.
great thoughts on this blog, thanks!
I’m on low carb for quite some time now (approx 2 years, even not in strict ketosis, some cheat days) and love it! My wife a bit less, she complains I smell of acetone, obviously one of the ketone bodies.
Is that an indicator I’m in NK?
Is acetone smell typical for NK?
Is there a way to avoid that smell and yet stay away from the carbs?
You mention you pay close attention to the timing of the protein consumption, but you don’t say what that timing should be? When should I (or shouldn’t I) have protein, ideally?
I’ll get to it.
Peter,
I’ve lost 30 pounds, will soon have a BMI of 25, and no longer need my BP meds – all from following your example. I can’t thank you enough.
From your posts and videos, I understand that insulin is an anabolic (building) hormone – that it helps the body use proteins, fats, and carbs for energy and store them as muscle and fat. I also get that while carbs cause a significant insulin response, protein causes some and fat causes none.
I get that eating these foods together can change their glycemic effect and our insulin response. (For example, that eating bread with olive oil or cheese may be better than eating bread alone.) But if someone eats plenty of carbs and fat together, they will get a significant insulin response. I’ve read that the body then does a great job of storing both dietary fat and carbs as body fat.
My question is this: I wonder if there might be additional benefit by eating one’s protein and fat at different times. The idea would be to eat lean meat and other protein alone, with no carbs and little fat, so the insulin response just helps build muscle. Then, when the insulin level has dropped, one would eat fat and other foods while still avoiding carbs (e.g., cheese, bacon, veggies with butter, salad with a high fat dressing, etc.).
In short, do you think it might help to eat fat mostly when one knows the insulin response will be low (from not eating protein and carbs)? Do you know whether anyone has tested this, or tried it on themselves?
Don’t get me wrong. I love eating meat with fat and it’s easier to eat normal meals. You are at your goal, and I’m getting there, so we might not need to bother with it. But I know others who say that the low-carb approach just doesn’t work for them. I tell them to make sure they really cut the carbs (e.g., to fewer than 20 gms/day). But I wonder if this might help them see results faster – not by changing what they ate as much as changing when they ate it.
Thanks again!
Very important question, Richard, and one I think about a lot. Your assumption certainly makes sense, but I’m not sure how much experimental data out there confirms it.
Hi Richard,
I’ve been thinking exactly the same. What I do currently is to have the bulk of my protein and carbs at breakfast and dinner because I bike to and from work (I’m thinking that the exercise will help lower the insulin response). At lunch I’ll limit protein and carbs, usually having mainly a salad, a little meat and olive oil to negate the insulin response.
I apply the same thinking around the ‘real’ exercise sessions. I’ll have more carbs after those as I think it’s better to have the hgher insulin response at that point. I still have fat with those meals though.
I think I have to try your suggestion of keeping the fat low at a post-workout meal to see if I hopefully can gain weight with that approach.
Best regards,
Hemming
I think you need to eat fat with your meat to be able to digest the meat.
It does make lots of sense and I have been thinking about exactly this: eating my fat and proteins at different times.
However, from what I understand (after reading Phinney and Volek’s books), free fatty acids are available in the blood stream at all times, and for the cells that will absorbe them, it does not matter whether they come from the meal you have just eaten or have been released from the fat cells. If the insulin levels go up, the fat cells will start storing them. So in the end it might not matter if you eat protein and fat at the same time.
On the other hand, it’s probably a good idea to eat more protein and less fat after the workout and then limit the protein and eat more fat at other not-post-workout meals. This is the approach I will want to test: fat only for breakfast (basically coffee and/or tea with coconut oil and heavy cream), a workout around noon followed by a higher-protein, lower-fat lunch, and for dinner, some meat (not too much) with green vegatebles and enough fat not too be hungry.
Thanks for the responses. Interesting observations. I’m still debating whether and how to experiment with this. I’ve gotten so used to eating fat and protein together, and have come to really enjoy it. (The sauteed mushrooms made my hamburger taste so much better last night!)
My diet path has been somewhat similar to Peter’s — from low-fat, to lower-carbs and whole grains, to high-fat and no carbs. My success has been similar too. (Except I don’t work out at his level. But who does?) I might go back to the high-protein, low-fat, low-carb approach for some meals (e.g., for supper, when I get most of my protein), and focus on eating higher-fat, lower-protein meals and snacks at other times. If I succeed in giving it a good try, I’ll let you know how it goes.
Thank you for this blog – it is exactly what I have been seeking. What are your thoughts on LCHF for those of us who are being treated for hypothyroidism? It seems that both calorie restriction and VLC reduce T3. The last thing I want to do to his reduce my already slow metabolism even further. I am looking to lose about 15 lbs of fat. In the past, LCHF has worked for me, but it seems since being treated for hypothyroidism, it doesn’t work as well. I am not looking for medical advice, just wondering what your thoughts are on LCHF and T3. Thanks!
Very misunderstood topic, and probably stems from an unclear understanding of clinically significant hypothyroidism (vs. lab value abnormality — typically normal TSH, but low T3 — this is probably not hypothyroidism).
Hi Peter,
I know you are already busy enough but is there any reliable information concerning insulin resistance and significant clinical hypothyroidism (i.e. due to a thyroidectomy)?
I ask because if you say the topic is not clearly understood, I’m hoping there’s some good info out there which you may have gathered for your upcoming post “Relationship between hypothydroidism and insulin resistance”.
I am aware of Chris Kresser’s info on the subject but anything else would be appreciated.
I’m grateful every day or the knowledge you share!
Chris has probably thought most about this. Also, check with Ron Rosedale.