In this episode, Dr. Peter Hotez M.D., Ph.D., Dean for the National School of Tropical Medicine Baylor College of Medicine, returns to continue the conversation on COVID-19. Dr. Hotez informs us on how we can gauge the number of infected people, behaviors to reduce the probability of becoming infected, and the inconsistency of hospitalizations among young adults between different countries. Dr. Hotez underscores the continued uncertainty in many virus-related developments, but ends with some points of optimism.
Disclaimer: This is information accurate as of March 19, 2020, when it was recorded.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- How to gauge true number of infected people [5:45];
- Reducing the probability of getting infected [22:45];
- Inconsistency by country in infected young people [27:15];
- Conferred immunity, seasonality, and repurposed therapeutics [30:30];
- Vaccine development [39:30];
- Practical behaviors to reduce risk of transmission [46:00];
- Mental health resource and funding [51:00];
- Points of optimism [56:00]; and
- More.
Show Notes
How to gauge true number of infected people [5:45]
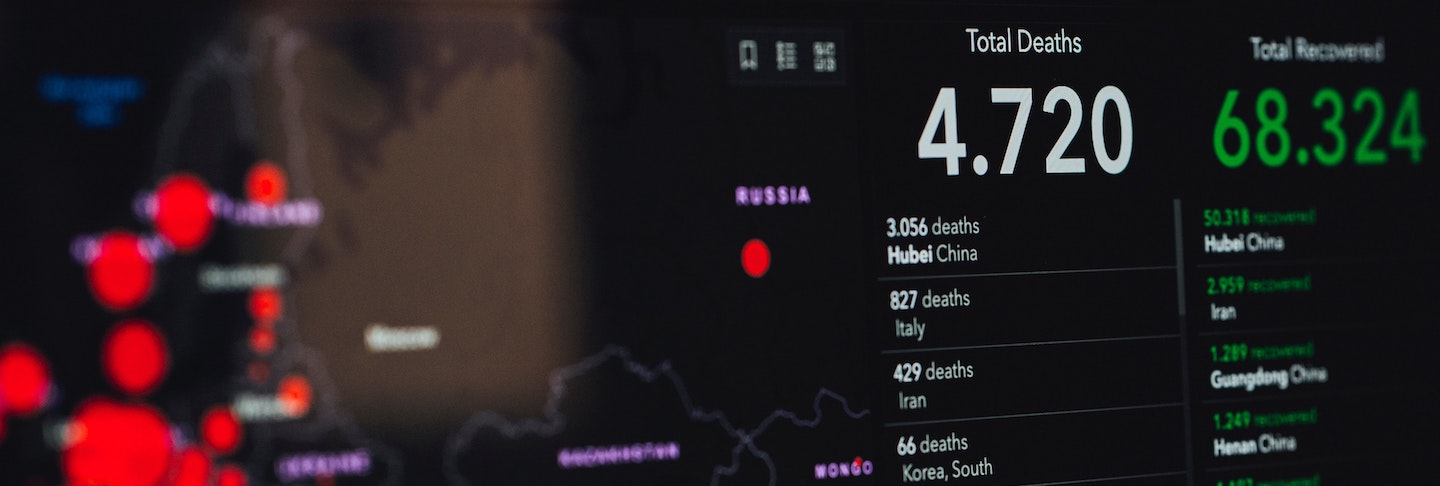
- ~13k cases confirmed in US as of midafternoon time of recording PST on March 19 2020
How does that translate to an estimate of actual people infected?
- Every day there is a large increase because there is testing underway
- We don’t have a real sense of % population infected and we are just beginning to pick up existing transmission
- Physicians in major hospitals are seeing a lot of cases and feeling overwhelmed meaning:
- Despite number of tested cases, there is still a ramp increase
- Creates concerned for system threshold to care for the sick
Distribution of total U.S. cases is where we should focus concern
- The distribution of absolute case numbers in the US is more insight-producing rather than total case numbers
Evaluating confirmed infected case multiplier (estimation):
-
- Takes into consideration:
- What is the assumed number of days to a fatality
- What is the assumed fatality rate?
The status of U.S. healthcare delivery
- Unclear how CDC made decisions around testing
- Peter has deflected these questions because there were missteps made and a committee will have to retrospectively evaluate to make sure the same mistakes are not made in the future
- It is a matter of figuring out how we rapidly fix the problem around hospital system stress
Rate limiting step in healthcare delivery
- New York City as a case example ….
- Doctors and nurses are demoralized: initial breakdown of trust
- Seeing colleagues get sick and inadequate support and preparation
- Disconnect between state and federal government management
No longer a disease of young adults
- Destabilizing for young physicians
- Front line healthcare workers are getting sick
What is the solution for staff workers getting sick?
- Heavily-hit Covid19 areas are likely experiencing understaffed medical support
- The whole healthcare system was fragile to begin with due to high demand on physicians
- There is no clear solution
Could we expand the U.S. public health service?
- Bring in individuals to train as medics who are currently under Furlow?
Reducing the probability of getting infected [22:45]
How much insight do we have about transmissibility?
- There is not a lot of new information about virus survival time on various surfaces
- We know that it can live on cardboard but how relevant is that?
- CDC came out with guidelines that loosened criteria of exposure
- A desperate move to have people remain in the workforce
- Convalescent serum could help people remain in the workforce as a form of prophylaxis
- White House came out with press report to create convalescent serum
- The recent study of blood type and susceptibility: not clear how relevant it is yet
- Study out of china showing that type O blood type had reduced risk
- Protective antibodies but not immunity like a convalescent serum
Inconsistency by country in infected young people [27:15]
- Younger age group in Italy getting ill but not seen in China
- High number of hospitalized people between 20-40 years old, accounting for ~33% of hospitalizations in the U.S.
- ~50% in the U.S. are under the age of 54 years old – very different than what was observed in China
- Individuals aren’t dying at as high rates as older population groups but they are still hospitalized
- Could this be due to vaping?
- Require good epidemiology on young patients to identify differences
Conferred immunity, seasonality, and repurposed therapeutics [30:30]
- Non-human primates show that once exposed, the infection should confer immunity
- The federal government thinks that the pandemic should last 18 months
- Operating under the assumption that the virus comes back in the fall
- Or could be anticipating that there is a vaccine in 17 months, but Peter does not think this is realistic
- Peter hopes that the model is not dependent on vaccine development
Repurposed drugs…
- Published Kaletra paper interpretation: drugs administered when viral progression is too far gone is not helpful
- Didier Raoul preliminary work has looked at hydroxychloroquine (HCQ)
- Small study reveals HCQ potential but has yet to be rigorously tested
We are on a steep learning curve around ARB and mechanistic action …
- ARBs have the ability to block viral entry but on the other hand, it may upregulate ACE2 receptor
- They may have anti-inflammatory effects
- Preliminary look on camostat out of Japan seems promising
Vaccine development [39:30]
Should we be considering a universal coronavirus vaccine rather than SARS or Covid-19 specific?
Practical behaviors to reduce risk of transmission [46:00]
- Peter Hotez does not believe receiving mail to be an issue
- Real risk is close, personal contact with someone infected
Mental health resource and funding [51:00]
“The psychological devastation on the United States […] is going to be almost as big as the damage of the infection.” —Peter Hotez, M.D., Ph.D.
Points of optimism [56:00]
- We are seeing scientists put at higher esteem
- At times of stress, people are looking to scientists and in leadership roles
- Science communication and data sharing has improved
“The heroism we are seeing of physicians of nurses… there is going to be a new awakening behind the medical community…” —Peter Hotez, M.D., Ph.D.




Have you watched the BBC “virtual pandemic” entitled Contagion? It appears somewhat prophetic.
Question: is there ANY possibility that it was already in US prior to January 2020?
Hoping to see what response you get to this question Gina a I have been curious about this as well.
My son was ill in mid-late January and thought he had the flu…even after the worst of the symptoms passed he experienced shortness of breathe which I thought a bit out of the ordinary when compared to times I’ve had influenza. He is currently a smoker and perhaps this is why he had the shortness of breath but I wonder.
Certainly people were traveling in and out of China and to other parts of the world including here before it was even known what they were dealing with there…so with the current thinking regarding it’s ability to spread I would think it to be highly unlikely that it just recently arrived here.
Look forward to learning more on this as well…
“Hoping to see what response you get to this question Gina a I have been curious about this as well.
My son was ill in mid-late January and thought he had the flu…even after the worst of the symptoms passed he experienced shortness of breathe which I thought a bit out of the ordinary when compared to times I’ve had influenza.”
I personally know a few people that had this same experience, and almost everyone I speak to knows of more people with these experiences at the end of last year. What will be interesting to watch for in the coming times are if these people have any immunity to covid2.
Peter and Peter,
Thank you for an enlightening discussion.
Here in Christchurch, New Zealand at Canterbury Health Laboratories, the turnaround time for results from swabs in our lab is 6 hours if the swab can be received by 11am. I’m keen to find out what kits we’re using.
I found your podcast of 19/03/2020 really informative. I founded it balanced and brought attention to points not mentioned in the media whether in the States or Europe. There are many people at the moment who feel vulnerable and in search of valid information. Your podcast has helped to fill this shortage
Peter & Team,
Thank you for your focus on Covid19. I’ve been following your work for about a year, stimulated by your published talks and interviews on lo carb and longevity, and was excited when you started your podcast.
You strike the balance with your insights and your questons between deep information and accessibility that I appreciate.
In this time of uncertainty, you’re providing an important public service.
Peter,
I’ve been intending to write for months now. I need to go back to my notes to confirm when I first stumbled across you. It would have been a Dan Harris podcast. Thanks to Dan for that. So many things I appreciate… love of science, accurate communication, Feynman, Formula 1, relentless drive to get things right, fitness, on and on… Right now – more than ever – just want to say thank you for all that you do. I am sure that you are feeling immense pressure right now to provide accurate information. Thank you.
Here is my question… this may have been addressed, so I apologize if this has been addressed elsewhere. When individuals are being tested.. Let’s use drive up testing as an example, I have not seen how the health care workers are decontaminating themselves between tests. Are individuals putting themselves at risk by getting tested? Clearly the healthcare workers need to protect themselves, but are you aware of healthcare workers inadvertently transmitting COVID-19 during testing. To expand on this, it doesn’t seem reasonable that they would change clothes everytime the health care worker is exposed. I’m assuming that they change gloves each time, but have not seen this covered.
You see people wearing gloves, but I’m guessing some people don’t understand that wearing gloves doesn’t necessarily protect you. There is a deeper process that people need to understand about why how gloves should be used. For example – walking around wearing gloves all day isn’t necessarily going to protect you if you’re still touching your face.
Anywhooo. Please take care. Thanks for everything. I have some thoughts I’ve wanted to share for a potential podcast on how people learn. More important things now, so I’ll save that for a future day.
RGS
Just curious if anyone is using/trialing N-Acetylcysteine in COVID-19?
Marc Seigel, M.D. did report a small hospital trial with NAC in which there was some success getting patients off ventilators, and preventing them from going on the vent in the first place. It is uncertain as to whether or not NAC inhibits viral replication, but as the rate-limiting amino acid for the synthesis of glutathione (faster-acting than taking a glutathione supplement itself), it logically follows that NAC could possibly act as a potent antioxidant to quench the cytokine storm in conditions such as ARDS. NAC has been tested in many human infectious diseases as well as many chronic inflammatory conditions.
I think even the most sensible of us have overstated the danger. Unless we consider the self inflicted damage to the economy. Best article I have read is below.
https://www.statnews.com/2020/03/17/a-fiasco-in-the-making-as-the-coronavirus-pandemic-takes-hold-we-are-making-decisions-without-reliable-data/?fbclid=IwAR0neJxO9Mpa01kEVb2_BwUBhEPUqWOlXgfiB1e14kpcRSavl7ilCk51ozw
From my observations and reading between the lines, SARSCoV2 is really very similar to an airborne illness, but official channels are avoiding that term, referring to aerosols…why is this?
If it is airborne………it induces well deserved panic.
There was a lot of good info, but in the early section when Peter asked what is the rate-limiting-step in dealing with this, they seemed out-of-touch by saying it’s the doctors and nurses.
The rate-limiting-step is clearly PPE, which is already on critical shortage and being severely rationed. We’re using unsafe levels of PPE even now, and the CDC is recommending bandannas and scarves for when we run out of masks completely. Seriously.
The lack of proper PPE is the reason the doctors and nurses will get sick, and also the #1 reason doctors and nurses are disillusioned. It all starts with the unpreparedness of our system and the unsafe circumstances in which we’re currently working (which are about to get worse).
In Arlington Tx, that has been my experience as well. And 10 day turnaround on testing, if you can get it. My ENT office (6 docs) is basically paralyzed by lack of testing and PPE. Turning away anyone with a sniffle or a fever (which is every ENT patient this time of year). And half staff because of quarantines for the same. My colleagues in the ER have the same problems.
It is droplet spread.
Aerosols can be generated by procedures, but for the most part n95 shouldnt be required?
If pt has a surgical mask, or even used good cough hygiene….that should greatly cut down on any transmission.
Michael: Yes, I think that many people don’t realize that aerosols are a lot smaller than droplets. Sneezes are not aerosols; they are droplets which, heavier than air, fall to the ground before they get farther than 6 feet.
Thank you Dr. Attia for your knowledge, flexibility, and insight during this time. We have especially benefited from your interviews with Dr. Hotez. Gratitude, thanks, ❤️❤️
Why is there never any data on the context of young people entering the ICU? We hear numbers like “32” and “26”, but are there comorbidities at play, like obesity, smoking, etc?
I wonder about that as well. If you pay close attention the media is VERY selective about what they do and don’t report.
It’s like they want to make sure people are scared so that they continue to take self-isolation seriously.
Look around and you’ll see other media sources telling a better, more accurate picture.
Like the fact that Italy’s death toll is so high is because most of the deaths come form a specific region with lots of older people who smoke a lot and where the air is very polluted and they also have underlying health conditions. But most of the time you hear reporters mention Italy and infer that the same thing will happen in the rest of the world. Not even close.
Is anyone looking to determine if there is any connection with the severity of illness based on the pharmaceuticals the patient is taking. Everything I have seen indicates the majority of deaths have been in those with comorbidities which typically also means a fair amount of pharmaceutical interventions being used on an ongoing basis. Also mention was made of mortality in younger age groups appearing to be higher here in the US…is it possible our patient population is on pharmaceuticals that are in some way affecting the CNS’ ability to deal with the virus. Even NSAID’s affect the CNS. In my elementary way of communicating this… the way I see it these medications are tricking the body into thinking it is doing something it is not or bypassing something the body would normally be doing or blocking something that the body typically does. Is anyone looking at that aspect and whether there may be some common denominator?
There’s absolutely no question that American children are on more pharmaceuticals than their international counterparts. How would this translate to higher mortality from viruses? I am thinking that perhaps one reason could be that many medications deplete zinc, which is crucial to antiviral immunity: https://academic.oup.com/advances/article/10/4/696/5476413
? Here is a very long list of medications that deplete zinc:
https://pennstatehershey.adam.com/content.aspx?productid=107&pid=33&gid=000728
I notice that NSAIDS are on the list of meds that deplete zinc. This may part of the reason why French physicians have sent out the message that NSAIDS make CoV infection worse. Indeed, the deadly second wave of Spanish Flu has been blamed partly on Aspirin, the 1st NSAID which was new at the time. Not knowing that (1) it suppresses immunity like steroidals do, and (2) it is toxic at high doses, the Army Surgeon General and JAMA made the recommendation to give very high doses of aspirin to Spanish Flu patients. The the infamous steep death spike of occurred immediately afterward. https://academic.oup.com/cid/article/49/9/1405/301441
Educational, focused, forthright, and honest.
https://www.biorxiv.org/content/10.1101/2020.03.13.990226v1.article-info
mentioned around 34 minutes on immunity and reinfection
Dear Peter
Thank you for your brilliant information
Elliot Fink
Dear Peter
Thank you for your brilliant information
Elliot
Do you think there is any hope that an at-home finger prick test for antibodies will be developed soon? It seems to me essential to know who has immunity.
https://www.3blumin.com/
Do you think We could use the above UV sanitizer to sanitize our Mask we are in front line and desperate for answer .