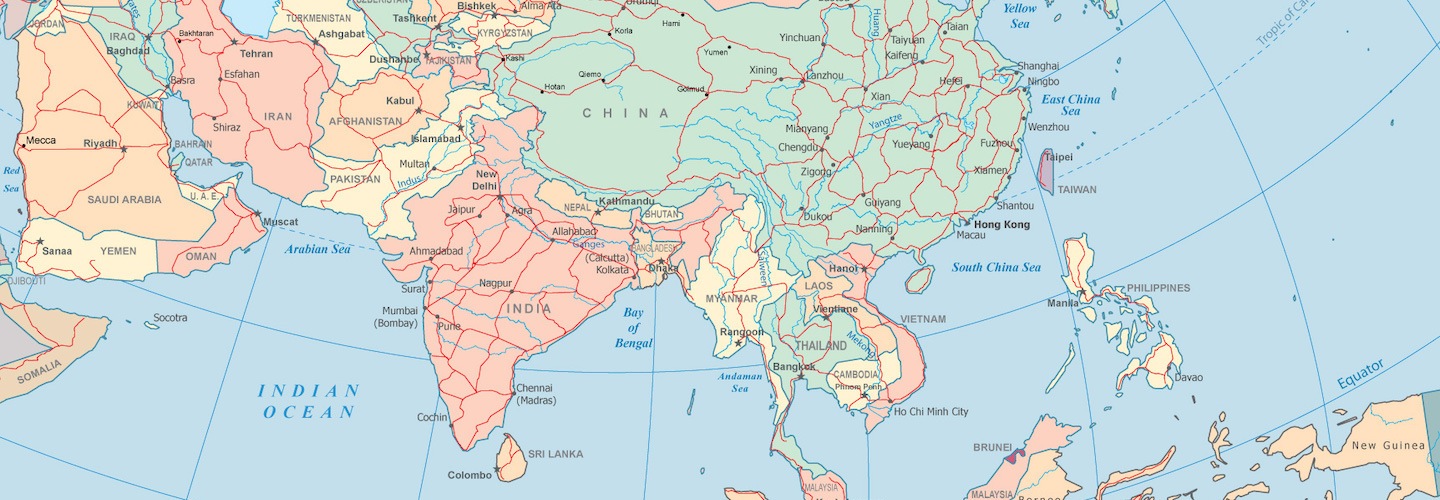
In this episode, Dr. Ronesh Sinha, a physician, author, and educator based in Silicon Valley, shares his many insights into metabolic illness that he has gleaned from his South Asian patient population. In this conversation we focus on hyperinsulinemia, insulin resistance, metabolic dysregulation, inflammation, blood pressure, obesity, etc. and ways to address them with nutrition, sleep, exercise, stress management, and more. We also take a deep dive into insulin resistant phenotypes, evolutionary theory and geographic determinants of insulin resistance which provides insight into the genetic architecture and pathophysiology of metabolic syndrome. Additionally, we discuss the surprisingly interrelated topic of stress, and how we might be inadvertently passing this on to our children, leading to mental and physical sickness down the road.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- How a stubborn case of insulin resistance connected Peter with Ronesh [7:15];
- Ronesh’s clinical treatment focus of metabolic illnesses in South and East Asian patient populations [8:45];
- The distinction between visceral fat and subcutaneous fat stores [15:00];
- Shortcomings of a body mass index (BMI) calculator for evaluating metabolic disease risk [17:15];
- Cortisol and blood glucose variability [28:30];
- Insulin’s role in elevated blood glucose: A symptom of metabolic syndrome [33:25];
- Mechanistic explanations of insulin resistance (there may be more than one) [35:15];
- Theories on origins and evolutionary reasons for insulin resistance [40:00];
- The inverse relationship between the amount of brown adipose tissue and rates of insulin resistance, and the role of climate in patterns and prevalence of insulin resistance [49:50];
- Vitamin D levels, hyperinsulinemia, and other effects [53:45];
- The evolutionary benefit of being able to turn fructose into fat (and the price we are now paying for it) [58:00];
- The VO2 max relationship to insulin resistance and familial metabolic health [59:30];
- Using zone 2 fitness test to evaluate mitochondrial performance [1:01:15];
- Exercise for long-term functional health [1:06:00];
- Lifestyle changes to improve insulin resistance and other metabolic phenotypes [1:14:00];
- Is PCOS a manifestation of insulin resistance? [1:21:00];
- The impact of stress on adiposity, and Peter’s treatment regimen for overweight females resistant to typical nutritional approaches [1:23:45];
- How a culture of achievement and expectations can lead to undue stress, unhappiness, and health problems in our children (a Silicon Valley case study) [1:35:00];
- The negative impact of devices and social media on children [1:48:45];
- How you can help yourself, your family, and your community without being an MD or PhD [1:55:00]; and
- More.
How a stubborn case of insulin resistance connected Peter with Ronesh [7:15]
How Peter and Ron connected:
- Peter had a patient from India who had an unusually stubborn case of insulin resistance
- There was something about it that looked a little different from the usual hyperinsulinemia (there was an “impressive degree” of inflammation)
- This particular case led Peter to Ron’s book, The South Asian Health Solution
- Peter and Ron eventually connected (thanks to an introduction by Mark Sisson)
Ronesh’s clinical treatment focus of metabolic illnesses in South and East Asian patient populations [8:45]
- In medical training, diabetes and cardiovascular disease case studies are typically African American, Caucasian, history of smoking, etc.
- Based in the Bay Area/ Silicon Valley, East and South Asian heritage were predominant population with early onset or family history of diabetes
- Realized there was a gap in resources between how physicians are educated and the populations most afflicted with metabolic diseases (e.g., insulin resistance, diabetes, cardiovascular disease)
- Decided to create East and South Asian population-specific educational materials and protocols
- Around the same time, Ronesh personally developed metabolic syndrome
- Prompted him to step outside nutrition guidelines and look more closely at insulin resistance
- He was following low fat, low-calorie model diet (eating meat, fish, healthy starch Bengal-style diet of his heritage)
- Gradually tinkered with personal and patient macronutrient meal composition
- Tracked triglycerides (TGs) between making changes
- Patients had high carbohydrate diet
- Relationship between carbohydrate (CHO) and fat revealed that high triglycerides (a.k.a: blood fat) were not reduced by a low fat diet
- Cut down on dietary CHO and prescribed more liberal dietary fat intake
- By contrast, African American patients can present with normal TGs and have diabetes
- Prompted Ronesh to look at patient habitus …
{end of show notes preview}

Ronesh Sinha, M.D.
Dr. Ronesh (Ron) Sinha, author of The South Asian Health Solution, runs a medical consult practice focused on preventing and reversing insulin resistant conditions in predominantly Asian Indians, who have some of the highest rates of type 2 diabetes and early heart disease in the world. He also designs corporate health education and wellness programs for major Silicon Valley companies like Oracle, Amazon, Google and more. More recently he has been focusing his energy on teaching busy families how to achieve better mental and metabolic health through talks/workshops at schools and corporations and online programs.
Instagram: @roneshsinhamd
Twitter: @roneshsinha





The Randle Cycle must be adhered to or insulin resistance will follow. This is why low fat vegans can lower their blood sugars and high fat carnivores can also lower their blood sugars even though these diets are completely different from each other. Everything else is happening downstream (hyperinsulinemia & fatty liver). Everyone is trying to fix the downstream symptoms ignoring the fact that the mitochondria can’t efficiently burn fatty acids and glucose at the same time causing the body to park this energy in the blood (triglycerides & blood sugars). Choose your energy source (fat/glucose) and stick with it.
Take a look at the work of Andy Galpin here https://www.andygalpin.com/ . He argues in favor of the concept of metabolic flexibility . I am not a physiologist but rather a primary care doc so I naturally gravitate to the idea of flexiblity.
Perhaps some of the folks that get stuck in IR have a metabolic/genomic disability – they cannot switch very well .
Thanks Peter and Ronesh for taking on a very important area with lots of application to primary care .
What a timely topic! Thanks Peter and Ronesh for a stimulating discussion. I have struggled with this malady within my own family members – not to mention my own proclivity towards IR.
Ronesh’s generosity in providing a wealth of information on his website is greatly appreciated. I’ve bought his book and have recommended him to all my physician colleagues from the subcontinent. There is a real dearth of good information out there and this podcast was very helpful. Thank you both again.
What’s the name of the “…really good sleep supplement out there that contains vitamin D” that Peter mentions?
Thanks!
I second this
I was curious about the interaction of diet and ethnic background. I feel this was not touched on enough in the podcast. I live in India for work and notice huge obesity problems. I also notice people are not eating a traditional diet. Often there are multiple sources of carbohydrates (rice, breads etc) rather than just one, and the also high amounts of refined oils are used. In addition people eat Indian sweets daily when once they were just eaten at festivals. Culturally, also being fat seems to be a sign of wealth. Curious to know thoughts about the current indian diet vs traditional.
Any updates on that sleep supplement that’s really good the one that has the additional vitamin D that they did not really like about it
Very interesting, I fall into the native American category as a member of the Cherokee tribe and I know we have some of the highest levels of diabetes of any ethnic group, which includes myself. I’ve experimented with a handful of different eating programs but have had the most benefit from a carnivore diet. Lowered my a1c from 7.8 to 5.9 , FYI interested hearing your comments on a1c.