You’ll recall from last week’s post I did a self-experiment to see if I could learn something about the interplay of exercise and ketosis, at least in myself. To understand this discussion, you’ll want to have read Part I of this post.
However, before getting to this, I want to digress and briefly address two unrelated issues:
- Some of you (about 67 or 68 as of this writing) have sent me various links to news reports released yesterday reporting on a study out of Harvard’s School of Public Health. I was planning to eventually write a post about how observational epidemiology is effectively at the heart of the nutritional crises we face – virtually every nutrition-based recommendation (e.g., eat fiber, don’t eat fat, salt is bad for you, red meat is bad for you) we hear is based on this sort of work. Given this study, and the press it’s getting, I will be writing the post on observational epidemiology next week. However, I’m going to ask you all to undertake a little “homework assignment.” Before next week I would suggest you read this article by Gary Taubes from the New York Times Magazine in 2007 which deals with this exact problem.
- I confirmed this week that someone (i.e., me) can actually eat too much of my wife’s ice cream (recipe already posted here –pretty please with lard on top no more requests for it). On two consecutive nights I ate about 4 or 5 bowls of the stuff. Holy cow did I feel like hell for a few hours. The amazing part is that I did this on two consecutive nights. Talk about addictive potential. Don’t say I didn’t warn you…
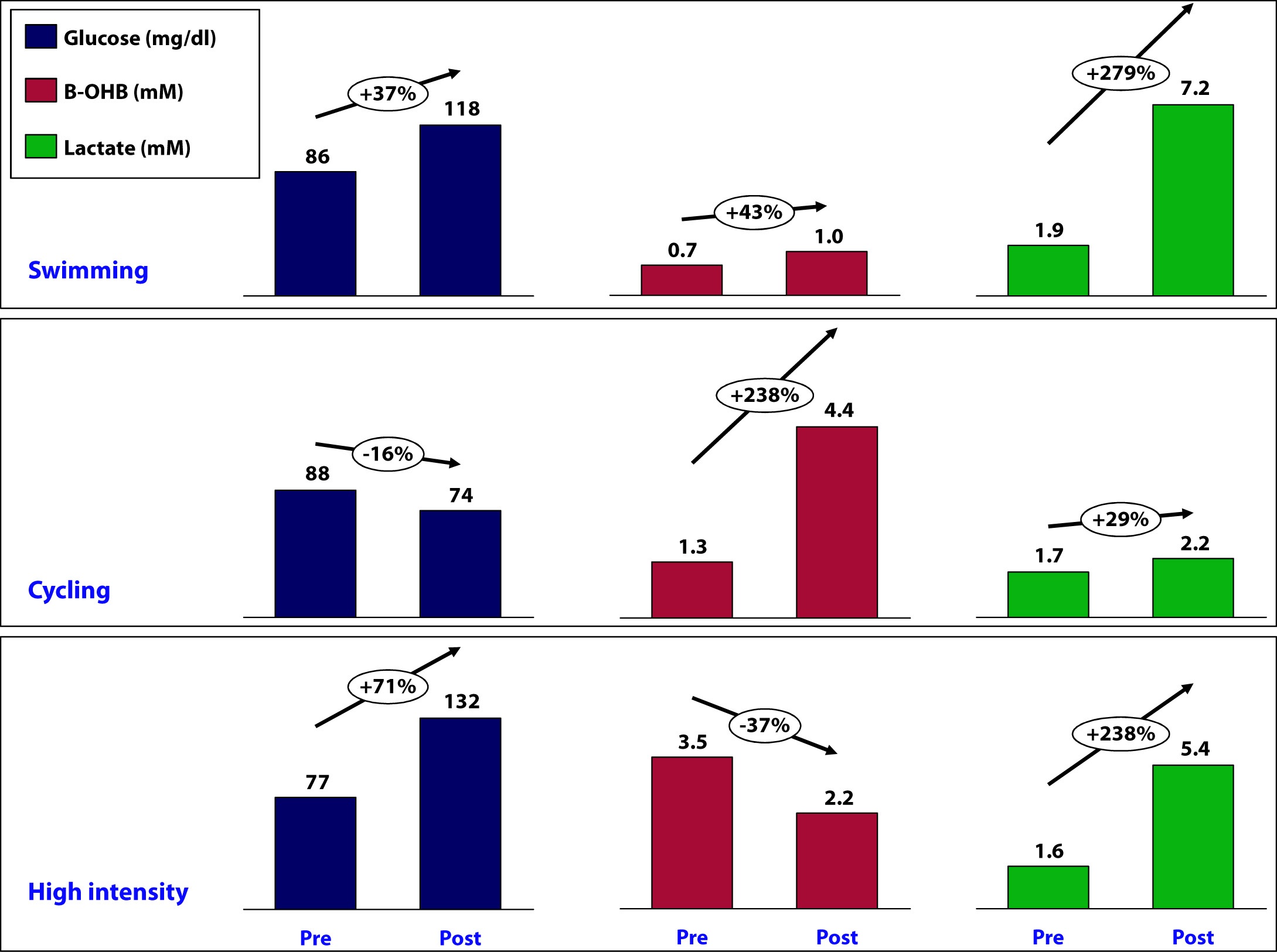
OK, back to the purpose of this post: How is ketosis impacting my ability to exercise? Here is the summary of the results from my personal experiment:
Let’s take a closer look at what may have been going on in each workout and see what we can learn.
Swimming
This workout probably produced the most lactate of the three workouts (we don’t know for sure because I only measured immediate pre- and post- levels without measuring in-workout levels). My glucose level rose by nearly 40% during this workout despite the fact that I did not consume anything.
How does this happen? Our bodies store glucose in the liver and in muscles in a “storage” form (a long chain of joined glucose molecules) called glycogen.
Whenever our bodies cannot access sufficient cellular oxygen, our metabolism shifts to a less efficient form of energy acquisition called anaerobic catabolism. During these periods of activity, we cannot oxidize fat or glycogen (i.e., use oxygen to harness the full chemical potential of fat or carbohydrate molecules). I will be writing in much more detail about these ideas in the next month or so, so don’t worry if these ideas seem a bit foreign right now. Just know that sometimes our bodies can convert fat or glucose to energy (efficiently), and sometimes we can only convert glucose to energy (inefficiently).
Because of my ketosis, and the metabolic flexibility that accompanies it, I only “require” that my body turn to glucose for energy under the most “stressful” forms of exercise – like I was doing a lot of during this workout. But keep in mind, my muscles CANNOT export one gram of the glucose they store, so any glucose in my bloodstream is either ingested (which I didn’t do) or coming from my liver, which CAN export glucose.
Furthermore, the stress of a workout like this results in my adrenal glands releasing a set of chemicals called catecholamines, which cause my liver to export even more of its stored glucose via a process called hepatic glucose output (HGO).
[As an aside, one of the major defects in type-2 diabetes is the inability of insulin to suppress HGO. In other words, even when not under the catecholamine stress that “should” lead to HGO, their livers constantly export glucose, which contributes to elevated blood glucose levels. The very popular drug, metformin, used often in type-2 diabetes, blocks this process.]
While I did experience a pretty large rise in lactate (almost 3x), my ketones still went up a bit. This could imply a few things:
- Elevated lactate levels do not directly inhibit beta-hydroxybutyrate (B-OHB)
- Mild elevations in glucose do not directly inhibit B-OHB
- Mild elevations in glucose do not directly inhibit B-OHB, if insulin is being suppressed (as is the case during vigorous exercise)
- B-OHB was suppressed, but we are only appreciating the net effect, which was a small increase (i.e., because of my MCT oil and activity, B-OHB levels were rising dramatically, but the rise was blunted by some other factor, such as HGO, insulin, and/or lactate)
More questions than answers from this workout, so on to the next workout.
Cycling
Despite this being a tough ride at several points, on average it was less stressful than the other two workouts and I spent the greater fraction of time in my aerobic to tempo (zone 2 to zone 3) zones.
A ride like this, however, is a great example of the advantages of improved metabolic flexibility that accompanies nutritional ketosis. My average heart rate during this 6 hour ride was 141. Prior to becoming ketotic, at a HR of 141 my respiratory quotient (RQ) was about 0.98, which meant I was almost 100% dependent on glycogen (glucose) for energy. Today, at a HR of 141 (with the same power output), my RQ is about 0.7 to 0.75, which means at the same HR and same power output as prior to ketosis, I now rely on glycogen for only about 10% of my energy needs, and the remaining 90% comes from access to my internal fat stores.
This is an important point. I will devote future posts to this topic in more detail, but I wanted to use this opportunity to mention it.
So what happened physiologically on this ride?
- My glucose levels fell, probably because I was slowly accessing glycogen stores for peak efforts (once my HR reaches 162 I become 50% dependent on glycogen) throughout the ride (e.g., peak climbing efforts, hard sections on flats), but my liver was not “called on” to dump out a massive amount of glucose in response to a catecholamine surge (and if it was, at some point during the ride, that amount of glucose had been used up by the time I was finished).
- B-OHB levels increased by about 2.5x – to 4.4. mM, which is pretty high for me. My highest recorded B-OHB level was 5.1 mM (also after a long ride). This confirms what my RQ data indicate — my body almost entirely relies on fat oxidation for energy for activity at this intensity. In the process, B-OHB is generated in large quantities, both for my brain and also my skeletal muscles (e.g., leg muscles). In reality, cardiac myocytes (heart muscle cells) also “like” B-OHB more than glucose and probably also access it when it is abundant.
- Lactate levels by the end of the ride were effectively unchanged though. Based on “feel,” I suspect I hit peak lactate levels of 8 to 10 mM on this ride during peak efforts, but I had ample time to clear it.
A few observations:
- I consumed 67 gm of carbohydrate on this ride (of which 50 gm was Generation UCAN’s super starch), yet this did not appear to negatively impact my ability to generate ketones. Technically, we can’t be sure this is the case, since I would have needed a “control” to know this (e.g., my metabolic and genetic twin doing and eating everything the same as I did, but without the consumption of super starch and/or without the bike ride). It’s possible that super starch did slightly inhibit ketosis and that my B-OHB level would have been, say, 5.0 mM instead of 4.4 mM. Metabolic studies of super starch show that it has a minimal impact on insulin secretion and blood glucose levels, hence the name “super” starch.
- Whatever impact peak levels of lactate production and hepatic glucose output had during the ride, they seem blunted by the end of the ride (and the ride did finish with a modestly difficult 1.4 mile climb at 6-7% grade, which I rode at a HR of about 150).
Since neither lactate levels nor glucose levels (nor insulin levels by extension) were elevated, I can’t really draw any conclusion about whether one factor, more than any other, suppressed production of B-OHB, so on to the next workout.
High intensity training
This sort of workout spans the creatine-phosphate (CP) system and the anaerobic energy system, and probably involves the aerobic energy system the least. I’ll write a lot about these later, but for now just know the CP system is good for very short bursts of energy (say 10-20 seconds) and recall the previous discussion of aerobic and anaerobic catabolism. In other words, this is the type of workout where my nutritional state of ketosis offers the least advantage.
- This workout saw the greatest increase in glucose level, about 70%. It is important to recall that during this workout I ingested water with a small amount of branched chain amino acids (BCAA’s – valine, leucine, isoleucine) and super starch, about 4 gm and 10 gm, respectively. I do not believe either accounted for the sharp rise in blood glucose and, again, I believe hepatic glucose output in response to a strong catecholamine surge attributed to this increase.
- Lactate levels also rose, though probably less so than during a peak swim effort. This suggests more of the effort in this workout was fueled by the CP system (versus the anaerobic system, which probably played a larger role in the swim workout).
- This was the only workout that saw a fall in B-OHB levels, which now offers some insight into what might be impacting B-OHB production.
Contrasting this workout with the swim workout draws a pleasant contrast: both saw a similar rise in lactate, but one saw twice the rise in blood glucose. In the former, B-OHB was unchanged (actually rose slightly), while in the latter, B-OHB fell by over a third.
This suggests – but certainly does not prove – that it is not lactate per se that inhibits ketone (B-OHB) production, but rather glucose and/or insulin. It is possible the BCAA played a role, and if I was thinking straight, I would not have consumed anything during this workout to remove variables. But I have a very hard time believing 3 or 4 gm of BCAA could suppress B-OHB. When you see hoof prints in the sand, you should probably think of horses before you think of zebras.
Conversely, there is some evidence that lactate promotes re-esterification of fatty acids into triglycerides within adipose cells. What does that mean in English? High levels of lactate take free fatty acids and help promote putting them back into storage form. This would prevent free fatty acids from making their way to the liver where they could be turned into ketones (e.g., B-OHB). In other words, we may be missing this effect because of my sampling error – I only sampled twice per workout, rather than multiple times throughout the workout.
So what did I learn, overall?
I think it’s safe to say I did not definitively answer any questions, which is not surprising given the number of confounding factors, lack of controls, and sample size of one. However, I think I did learn a few things.
Lesson 1
The metabolic advantages of nutritional ketosis seemed most apparent during my bike ride, evidenced by my ability to access internal fat stores across a much broader range of physiologic stress than a non-ketotic individual. (More on this in Lesson 4.)
Lesson 2
The swim and high intensity dry-land workouts suggested that my state of nutritional ketosis did not completely impair my ability to store or export hepatic glucose. This is a very important point! Why? Because, it runs counter to the “conventional wisdom” of low-carb (or ketotic) nutrition with respect to physical performance. We are “told” that without carbohydrates we can’t synthesize glycogen (i.e., we can’t store glucose). However, those who promote this idea fail to realize that glycerol (the backbone of triglycerides) is turned into glycogen, along with amino acids, not to mention the 20 to 40 gm of carbohydrates I consume each day (since my brain doesn’t need them). We know muscles still store glycogen in ketosis, as this has been well studied and documented via muscle biopsies by Phinney, Volek, and others. But, my little self-experiment actually adds a layer to this. Because muscle can’t export glucose (muscle lacks the enzyme glucose-1-phosphatase), we know that the increase in my blood glucose was accounted for by HGO – my liver exporting its glycogen. In other words, ketosis does not appear to completely impair hepatic glycogen formation or export. Again, we’d need controls to try to assess how much, if any, hepatic glycogen formation and/or export is inhibited. It’s hard to make the argument that being in ketosis is allowing me to swim and do high intensity training with greater aptitude, and as I’ve commented in the past, I feel I’m about 5-10% “off” where I was prior to ketosis for these specific activities, but at the same time, I could be doing more to optimize around them (e.g., spend less time on my bike which invariably detracts from them, supplement with creatine which may support shorter, more explosive movements), which I am not.
Lesson 3
Consuming “massive” amounts of super starch (50 gm on the ride), did not seem to adversely affect my ketotic state. My total carbohydrate intake for that day, including what I consumed for the other 18 hours of the day, was probably close to 90 gm (50 gm of super starch plus 40 gm of carbs from the other food I ate). This suggests one or two possibilities:
- Because of the molecular structure of super starch (I’ll be discussing this in the future, so please hold questions) and the concomitant metabolic profile that follows from this structure, it may not inhibit ketosis like other carbohydrate, and/or
- During periods of profound physical stress insulin secretion is being sufficiently inhibited that higher-than-normal amounts of carbohydrate can be tolerated without negatively impacting ketone production.
This is pretty straightforward to test, even in myself. I just haven’t done so yet.
Lesson 4
While it’s probably the case that my liver has less glycogen (i.e., stored glucose) at any point in time, relative to what would be present if I were eating a high-carb diet, it’s not clear this matters, at least for some types of workouts. Why? Take the following example:
- Someone my size can probably store about 100 gm of hepatic (liver) glycogen and about 300 gm of muscle glycogen at “full” capacity. This represents about 1600 calories worth of glucose – the most I can store at any one time.
- Before I was ketotic, my RQ at 60% max VO2 (about 2,500 mL of O2 per min consumption) was nearly 1.00, so at that level of power output (a pace I can hold for hours from a cardiovascular fitness standpoint) I required 95% of my energy to come from glycogen. So, how long do my glycogen stores last? 2,500 mL of O2 per minute translates to about 750 calories per hour, so I would be good for about 2 hours and 15 minutes on my glycogen stores.
- Contrast this with my ketotic state. Let’s assume my glycogen stores are now only half what they were before. Muscle biopsy data suggests this is probably an overly conservative estimate, but let us assume this to be the case. Now I only store 50 mg of hepatic glycogen and 150 gm of muscle glycogen, about 800 calories worth of glucose.
- In ketosis, my RQ at 60% max VO2 is 0.77 (at last check), telling me I am getting only 22% of my energy from glucose and the remaining 78% from fat. So, how long do my depleted glycogen stores last? Nearly 5 hours. Why? Because I barely access glucose at the SAME level of oxygen consumption and the same power output.
I know what you’re thinking…why is this an advantage? Just consume more glucose as you ride! It’s not that simple, but you’ll have to wait until my upcoming post, “What does exercise have to do with being in the ICU” to find out.
Going back to the black sheep example I open Part I of this post with, we know that at least one person in nutritional ketosis seems to make enough liver and muscle glycogen to support even the most demanding of his energetic needs.
Photo by Troy Oldham on Unsplash






Doc,
First off, thank you for all the information you provide. I’m a Type-2 Diabetic and have struggled with weight and have now read and implemented this low-carb way of life, which is really showing progress. I take Lantus, metformin, and meal time Humalog, if necessary. I really enjoy high intensity cross-training, however it does elevate my glucose considerably. Over the long haul is this going result in the inability to be in ketosis through out the day or am I not understanding the HGO concept? I don’t want to be injecting unnecessary insulin through out the day and overall I’m trying to eat my way off my meds if that makes sense. Again, thank you for your time and information. By the way, I live in the Rio Grande Valley and we really need some resources for the Diabetes and Obesity epidemic down here!!!
Great post!
Do you think it is possible to get into a state of ketosis on a plant-based diet? It seems like consuming <50g/day of carbs on a vegan diet without mostly relying on commercial products (and tofu) will be significantly harder… (one cup of any random legume typically has 40+ grams of carbs, and without legumes it's pretty hard to get enough protein and iron). What are your thoughts about this? If you know any good sources, I'd greatly appreciate them.
Yes, but probably high in N-6 and relatively low calorie.
Dr. Attia:
Many thanks for your fantastic blog, and for your sacrifice of time to maintain it!
I wish I could post pictures so you could appreciate my pre-keto/pre-Attia-blog-reading self with the current incarnation.
July 2013, at age 46: female, PCOS, metabolic syndrome, Hashimoto’s, chronic anemia due to multiple fibroids the size of boulders, height 5’7″, weight 230. Exceptional diet by conventional standards: 80% organic, no fried foods, no processed foods, no “cheap carbs, no meat of any kind excepting fatty fishes like wild sardines, wild salmon, wild halibut, and longline-caught albacore, omega-3 eggs, quinoa, steel-cut oats, brown rice, barley, faro, etc., and the spectrum of vegetables and fruits.
Began reading your blog, became inspired, and found a doctor who would give me iron infusions so I could find enough energy to get motivated, and moving, and then found a trainer and joined a gym. Two years later, July 2015: metabolic syndrome completely reversed. Hb1ac 5.1, glucose levels consistently in the mid 80s. I occasionally eat beef, pork, duck, lamb, etc., but try to stick to my fishes and occasional shellfish, and get my fats from avocado, evoo, coconut oil, eggs, and nuts. I attempt to keep my carbs <50g by eating zero grains and virtually zero fruit, and sprinkle in leafy greens and vegetables wherever possible, although I have to cook most vegetables to reduce goitrogenic effects. Weight 150. Gym 6-7 days per week, mostly strength training with HIIT and bootcamp workouts 3 times per week. Still rolling despite Jan 2014 ovarian cancer diagnosis following surgery to remove 12.5cm mass covering right ovary; diagnosis was incorrect—corrected to widespread endometriosis//mass was endometrioma. Also still rolling despite Feb 2014 melanoma diagnosis and subsequent wide excision surgery.
No current meds except iron infusions. Here's my current concern: I took a peek online at my blood work performed prior to a recent iron infusion, and was surprised to note that my creatinine was 1.2 and corresponding GFR was 48, BUN = 25. I began drinking lots of water, and had them re-check. On the re-test, I had them fax my results, and GFR (89) and creatinine (.70) had straightened out, but my BUN was 22 and my BUN/Creatinine Ratio was 31.4, so the brunt of whatever imbalance I am experiencing had obviously shifted from my kidneys to my liver. I freaked out a bit, and had the establishment fax over my labs from visits in March, May, and the two recent (July), and compared all four, and it appears some/all of these numbers have been in the red from time to time over the course of these last few months, with no comment from the doc/nurse/lab. It appears they only run the test to use my LOW iron/ferritin levels as argument so my insurance company will pay for the $5000 infusion, and pay no notice to the other numbers?
Question: is it possible that my keto diet could have put me here? Or is iron more likely to blame? Too much protein? Or simply a factor of massive monthly blood loss from my cycle? Is a nephrologist my next move?
I am doing so well and feeling so good, and am so disappointed and worried that I may have damaged vital organs, all under the nose of physicians??
Do you accept patients from Memphis, TN? 🙂
Many thanks in advance for any response anyone might have, and have more numbers I can post if additional detail will assist—-
sam
Just want to thank you for all of your honest experiments and reporting. At 56 years old I started a keto food program 14 days ago and passed .5 mmol/L after 5 days and have risen to ~2.2 depending on the time of day/exercise. What is fascinating is that I came home from a group ride last weekend feeling good with my glucose at 61 mg/dL while at the same time ketones were 2.6. I would normally be sitting on the curb at that glucose level. Also experimented with a big Thai meal with white rice and went from 2.2 morning to .4 morning to test my ability to cheat. Another thing, just that one meal changed the whole character of my sleep (as suggested by a sleep app graph) from deep almost motionless sleep to a modestly fitful but deep sleep. If I go back 12-14 days on the app graphs this fitful pattern shows up again. I think it is possible that keto eating might improve circadian adjustment, I now have a hard time staying up late and I wake up an hour earlier on average. Still pushing out the no carbs (road) cycling endurance. Probably take another four weeks to be full power plus at the end of a long ride. Thanks. Good stuff.
Bill
This kind of tweaking and physiological self-experimentation is why I spent nearly 3 years in ketosis. Just so cool to see what happens at the boundaries.
Peter,
When using MCTs would you recommend coconut oil or a specific MCT oil. Also would taking MCTs bring you out of ketosis since it does not illicit an insulin response.
Thanks
Hi Peter,
I must say i am enjoying the huge amount of information on your site – even though a lot of it is totally over my head! Anyway i am experimenting with a ketogenic diet in the hope of completing a long distance ironman triathlon in June. The thought of avoiding all the gastric upset that i have suffered in previous races is most appealing but i am confused as to what i should consume during the race – now obviously the aim is to stay in fat burning mode for the duration of the race but is there a limit to how much race carbs one should eat. Looking at other endurance athletes who follow a ketogenic diet e.g Pete Jacobs and an ultra runner whose name escapes me both seem to consume huge amounts of carbs during race – which must take them out of ketosis yet it does not seem to affect them adversely? Or would you advise me to simply stick to UCAN super starch (despite the disgusting chalky taste) and fat from say nuts and even 85%cocoa chocolate? Have you any advice or guidance and are you still in ketosis?
With thanks Ed
So wait, just to make things really simple:
Can the athletic advantages of being in ketosis AND being on a high carbohydrate diet be achieved, simultaneously, if one is on a high carb diet, whilst also taking a ketone supplement? The one I’m referring to is KetoCaNa (or KetoForce). https://prototypenutrition.com/ketocana.html
PS: Thank you so much for your posts. They’ve actually helped me study a lot more for my Biology assessments without me even realizing it (got my first A star 3 weeks ago!).
Nice!
Hi Peter,
I’m SO glad I came across your blog. I’ve been on a LCHF lifestyle for about 4 months now and I’ve lost 11.5kg with more to come. I am so happy with my life and in the best shape of my life at 43. I do a daily (fasting) 12-minute HIIT workout first thing in the morning 5 days per week and I was very concerned about muscle loss when I read about ‘cannibalizing your muscles’ on other blogs that push the HCLF lifestyle and all kinds of strange ‘carb-loading’ permutations being required to not lose muscle when you are in ketosis. If I understand you correctly, one can still build muscle and lose fat while on LCHF? I do seem to have lost some bulk, but my sense is that it’s probable adipose tissue in the muscle which is being used when I am in ketosis, so I just need to carry on with my existing regime.
Thanks so much for a brilliant blog- you have won a fan for life! Strength to you.
In general, without anabolic agents, it’s tough to gain muscle and lose fat simultaneously. They tend to move together. But it can be done…requires very careful nutrition and training (and good genes).
Peter I love the enthusiasm but you can’t do sincere science with a sample size of one or draw any meaningful conclusions…
which why he has repeatedly, explicitly stated as much. Thanks though.
Hi Peter. Thanks so much for your blog and all the information it contains. I’ll also have to thank Tim Ferris for introducing you on his podcast.
Sorry to bother you with a question, but I really can’t think of who else to ask. I’m 55, fit and healthy. I also have two parents with Alzheimer’s disease. I’ve recently begun a ketogenic diet and I’m going to try to get a script for Metformin (not because of any metabolic indicators). Can you think of any reason why this would be a bad or terrible idea?
Thanks,
Andrew
I came back to your blog after reading about this guy who apparently clears lactate by having a “high alkaline” diet. What are your thoughts? Google “Dean Karnazes”. Multiple articles state that they did a lactate threshold test, and had to give up after more than an hour, because he didn’t accumulate lactate.
Nothing to do with alkalinity of diet. It has to do with lactate transporters on cells.
Im not too active (22 year old male.)..I walk alot nothing crazy. I eat about a bundle of kale which is the extent of my carbs. I do eat about 100 grams of protein through organ meats (cheaper). Will this really effect my ketone levels if i eat a good amount of saturated fat? Also does it matter if i consume that protein all at once? Will that effect if my chooses to burn the amino acids over the fatty acids? or does that happen simultaneously? I made sure to look at all the comments before so i dont ask a repeated question. Thanks Dr.
Peter,
Thank you for taking the time to make the information you provide understandable to us non-medical lay persons! I am able to understand and apply the information you present in a way that hundreds of hours reading medical report findings have never produced. I liken it to trying to learn algebra without knowing arithmetic.
On to a more specific question… I recently completed a 5-day water fast with a full metabolic / blood / urine round of testing and a couple of the results surprised me and I am hoping you can provide some insight into the results in light of water fasting for 5-days?
Component Your Value Standard Range Flag
Proinsulin 34.0 1.5-14.9 uIU/mL H
Insulin, Free 14.5 1.5-14.9 uIU/mL
Albumin 4.8 3.2-4.7 g/dL H
Total Bilirubin 1.2 0-1.1 mg/dL H
Total cholesterol 177 0-200 mg/dL
Triglyceride 237 0-150 mg/dL H
HDL cholesterol 28 mg/dL L
LDL Calculated 102 0-100 mg/dL H
Cholesterol to HDL Ratio 6.3 0-4.98 H
LDL:HDL Ratio 3.64 1.00-3.50 H
VLDL (Calculated) 47 4-30 mg/dL H
Sincerely,
Robert A.
I have been in ketosis for 2 months and have a few questions, I struggle to get into / maintain the +1.5 optimal zone. [I’m generally eating 30-40g carbs, 70-100g protein]
1. Does your body improve over time, ie if I keep doing what I’m doing can I expect my ketone score to go up?
2. It seems I’m sensitive to the amount of protein I consume. It looks like I need to keep below 85g maybe less. (I’m 57Kg 10% body fat so that puts the protein level right at the lower end). I weight train with heavy weights, trying to build mass (which I find hard) I worry re having such low protein. Should I, or do you require less protein when in ketosis?.
3. What type exercise (HIT training, heavy weight training, low level endurance, high level endurance etc.) is best for increasing the my ketone level score to help get me in / stay in the optimal zone
Any answers greatly appreciated
Is there anyway that your decrease in ketones during the high intensity exercise could be due to you using the ketones for energy?
That probably accounts for much of it.
Hi Peter,
Not sure if you are still monitoring this but just in case…
Just looking at the charts it appears that there is a reduction in lactate with an increase in ketone metabolization.
I came here via a google search looking for this information because last Friday I had an unusual experience in my swim workout. I usually start off with 4-500 yard warmup and in that initial swim I almost always go through a lactate cycle in my upper arms between 200 and 300 yards.
On Friday I did two 500s followed by 10 5 100 IMs followed by another 500 and never hit a lactate cycle. I had been consuming 2-3 tablespoons of mtc oil per day for the last week. Earlier in the week I did two 1-1.5 mile lake swims while camping. I always look forward with some trepidation to the discomfort of the lactate interruption and was very surprised to not encounter it. In addition I have an snp that suggests that I will not have success trying to extend the lactate cycle.
So my question is can mtc/ketosis help to avoid lactate/lactic acidosis. This was a one time sample but it was as I said very surprising.
I’m 72 diagnosed T2D then changed to delayed onset hyperglycemia. My last 3 a1cs were 5.5 5.5 5.4 and my fasting is usually about 108. No meds other than supplements though I am considering metformin and perhaps a fibrate for LDL due to rs1800206 though the evidence for coronary risk doesn’t appear that high and an angiogram earlier this year showed 20% and 30% blockages.stenoses with minimal lumen damage which I think at 72 is not bad.
Mike
Apparently mtc consumption enhances gluconeogenesis in rats so perhaps that is delaying the lactic acidosis which seems to be still happening. https://www.jnimonline.com/article/S2352-3859(15)00005-5/fulltext
Hey man, thank you for all of this. I’ve been back and forth searching like crazy for some legitimate source of info on this subject and your posts here are beyond what I thought I would find.
Question: I box and do jiu jitsu 3 days a week (Tues, Thurs, Sat). Because of my schedule and the gym’s schedule I do a full afternoon of training on those days (3 to 4 hours each day). It’s pretty intense, live sparring things like that. My first question is, in your opinion, what is the most optimal diet for this type of training (Keto, low-carb, or carb-loading)? If just low-carb, how many grams of carbs roughly? I hear a lot of 100-150g but i understand that degrades my fat-burning efficiency. I’d rather be fully Keto if possible.
My second question: I come from a high-carb/low-fat upbringing. I’ve studied diet most of my life. I truly believe in everything you’ve written here. But since I don’t eat dairy I really have few fat options I feel. Basically all I can gather for fat intake is from Eggs, Beef, Avocados, Olive Oil, Coconut Oil, and Nuts. Once I lay out the math with a 2500-3000 cal diet at even, say 1g of protein per bodyweight which may be on the high side, only 50g of carbs, that leaves a heck of a lot of calories to meet my daily requirement. So my question is, should I truly be eating that much fat? Also since carb intake is next to nothing, and most good fats are either part of my protein sources or from oils, I feel like the physical meal sizes would be such small portions of food and lots of oils which are simply liquids.
I don’t mean that to sound like a challenge to your obvious expertise on the subject, quite the opposite. I’m simply trying to wrap my head around it. The science is very logical. But considering the quantity of food I’d eat on a predominantly carb diet, I’m having trouble actually taking that science and implementing it into daily meals. I apologize for the length. And again I appreciate your site I can’t say it enough! Thank you
I am interested in what you think is the best adaptation for high lactate demand events? Both the 200 IM swim and the 800m run are about two-minute events. You comment that your ketosis adaption took around 12 weeks. Can you estimate your performance on a SAD diet vs. a ketosis diet? Are there any studies in humans comparing sugar to fat fuel?
Hard to see keto offering an advantage for ~2 min events.
Can you suggest any high-intensity strength training exercises that maximizes 2b fibers in us 40+ old folgies?
Peter – Thank you for your excellent post and self-experimentation! Your experience with the fluctuations in glucose and ketones match my own, and your explanations match a lot of what I’ve read. Your explanations and honest interpretations are outstanding. The reason I came back to your post is because I was diagnosed as Type 1 diabetic a few months ago, and what you’d call the ketogenic diet makes it much easier to manage (i.e. small inputs of carbohydrate mean smaller doses (and thus mistakes) with insulin). I’ve been able to perfect my management except in one realm: high intensity exercise. I noticed that your glucose went up to 132 when you were lifting weights, but of course, during this test you ate some stuff. There aren’t many non-diabetics measuring their blood sugars – and even fewer who are also athletes, so I’m curious: how high can your blood glucose go from intense exercise? Well over 130? It’s been a long time since you’ve done this post, so I assume you’ve gathered more data. Mine can increase from 85 to 190 in 6 minutes of high intensity – with no food. My definition of high intensity would be trying to run a sub 5 minute mile, so a big muscle group and no resting like you get in weight lifting. If you think about that, it’s an amazingly rapid “dump” from the liver into the bloodstream. My curiosity is: does a healthy person also experience this same hyperglycemia? Everything I read says if you go over 130, you’re diabetic… I’m curious about this because I am trying to optimize my performance for 5 minute events. If the blood glucose is shooting upwards, it seems that it would be beneficial to have more insulin on board so that the liver’s dump could be utilized instead of “wasted.” Furthermore, having high blood sugar could potentially decrease performance as well. Injecting insulin before a workout is scary, though, because you could potentially have dangerous hypoglycemia. I’ve been using a Dexcom G5 CGM to try and maintain glucose at 85. It’s very helpful, but unfortunately runs about 20 minutes behind a fingerstick.