Want to catch up with other articles from this series?
- The straight dope on cholesterol – Part I
- The straight dope on cholesterol – Part II
- The straight dope on cholesterol – Part III
- The straight dope on cholesterol – Part IV
- The straight dope on cholesterol – Part V
- The straight dope on cholesterol – Part VI
- The straight dope on cholesterol – Part VII
- The straight dope on cholesterol – Part VIII
- The straight dope on cholesterol – Part IX
Previously we addressed these 3 concepts:
#1 — What is cholesterol?
#2 — What is the relationship between the cholesterol we eat and the cholesterol in our body?
#3 — Is cholesterol bad?
I want to thank folks for doing their best to resist the following two urges:
- Please resist asking me questions beyond the scope of this post. If it’s not in here, it will probably be in a subsequent post in this series.
- Please resist sending me your cholesterol numbers. Share your story with me and others, but understand that I can’t really comment other than to say what I pretty much say to everyone: standard cholesterol testing (including VAP) is of limited value and you should have a lipoprotein analysis using NMR spectroscopy (if you don’t know what I mean by this, that’s ok… you will soon). I can’t practice medicine over the internet.
Remember last week’s take away messages:
- Cholesterol is “just” another fancy organic molecule in our body but with an interesting distinction: we eat it, we make it, we store it, and we excrete it – all in different amounts.
- The pool of cholesterol in our body is essential for life. No cholesterol = no life.
- Cholesterol exists in 2 forms – unesterified or “free” (UC) and esterified (CE) – and the form determines if we can absorb it or not, or store it or not (among other things).
- Much of the cholesterol we eat is in the form of CE. It is not absorbed and is excreted by our gut (i.e., leaves our body in stool). The reason this occurs is that CE not only has to be de-esterified, but it competes for absorption with the vastly larger amounts of UC supplied by the biliary route.
- Re-absorption of the cholesterol we synthesize in our body (i.e., endogenous produced cholesterol) is the dominant source of the cholesterol in our body. That is, most of the cholesterol in our body was made by our body.
- The process of regulating cholesterol is very complex and multifaceted with multiple layers of control. I’ve only touched on the absorption side, but the synthesis side is also complex and highly regulated. You will discover that synthesis and absorption are very interrelated.
- Eating cholesterol has very little impact on the cholesterol levels in your body. This is a fact, not my opinion. Anyone who tells you different is, at best, ignorant of this topic. At worst, they are a deliberate charlatan. Years ago the Canadian Guidelines removed the limitation of dietary cholesterol. The rest of the world, especially the United States, needs to catch up. To see an important reference on this topic, please look here.
Concept #4 – How does cholesterol move around our body?
To understand how cholesterol travels around our body requires some understanding of the distinction between what is hydrophobic and hydrophilic. A molecule is said to be hydrophobic (also called nonpolar) if it repels water, while a molecule is said to be hydrophilic (also called polar) if it attracts water. I could spend a lot of time getting in to the nuances of these properties, but I think it’s best to just focus on the major issues. Think of your veins, arteries, and capillaries as the “waterways” or rivers of your body.
BONUS concept: Another important concept is that cell membranes are lipid bilayers (which are hydrophobic) as I wrote about last week. Hence, a hydrophilic substance cannot pass through lipid membranes. Substances that can pass through lipid membranes are said to be lipophilic. A substance that has both polar (hydrophilic) and nonpolar (hydrophobic) properties is called amphipathic. The fact that unesterified cholesterol (UC) is an amphipathic molecule is a crucial property for its location in cell membranes. CE in which the –OH group has been replaced by a long chain fatty acid is a very nonpolar or hydrophobic molecule.
If a molecule needs to travel from your gastrointestinal tract (A) to, say, a cell in your quadriceps muscle (B) it needs to get on the river and travel from point A to point B. Because blood is effectively water, (the “water” part of blood is called plasma, an aqueous solution with a bunch of “stuff” in it (e.g., red blood cells, white blood cells, other proteins, ions) there are two ways to move down the river – swim or hitch a ride on a boat.
If a molecule is hydrophilic, it can be transported in our bloodstream without any assistance – sort of like swimming freely in the river – because it is not repelled by water. Conversely, if a molecule is hydrophobic, it must have a “transporter” to move about the river because the plasma (water) wants to repel it. I know this seems like a strange concept, but if you think about it, you’ve already seen great examples in your day-to-day life:
Sugar and salt will easily dissolve in water. They are, therefore, hydrophilic. Oil does not dissolve in water. It is, therefore, hydrophobic.
By extension, a molecule of glucose (sugar) or sodium and chloride ions (salt), because of their chemical properties which I won’t detail here, will travel through plasma without assistance. A lipid will not.
All of this is a long way of saying that sterol lipids (of which cholesterol ester is the predominant form in plasma), because they are hydrophobic, need to be carried around our bloodstream. They can’t move from one place to the next without a protein transporting molecule.
In other words, cholesterol doesn’t exist in our bloodstream without something to carry it from point A to point B.
So what are these “transporting molecules” called?
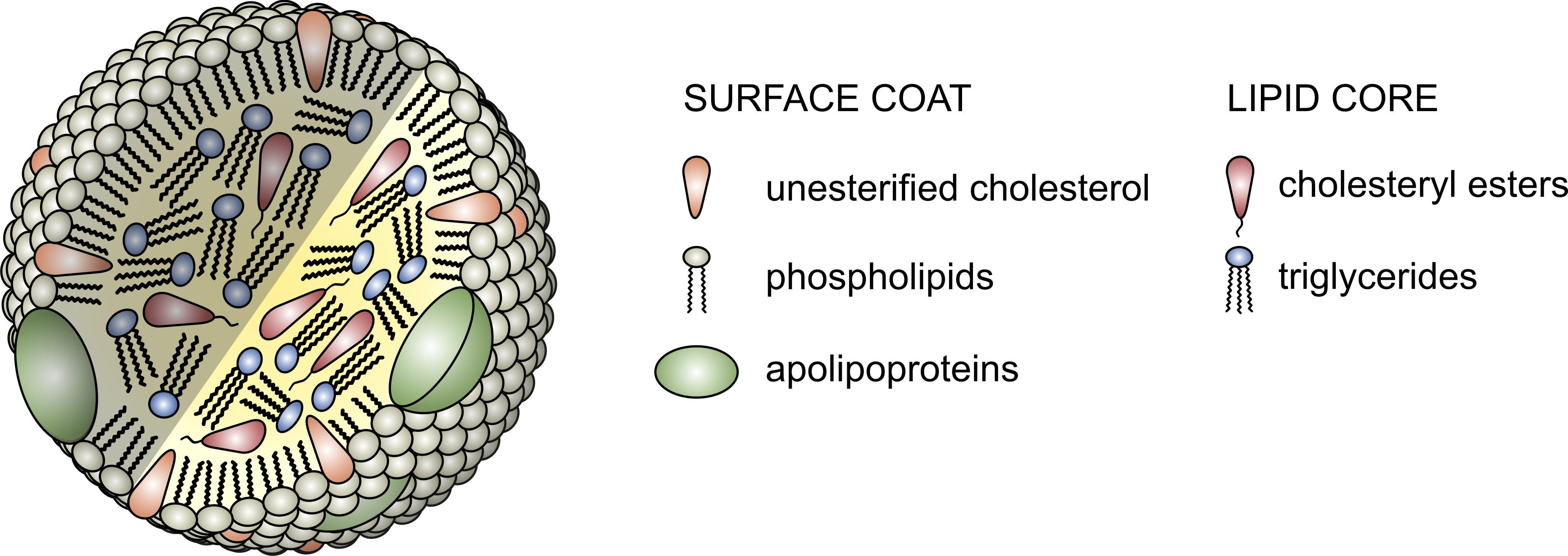
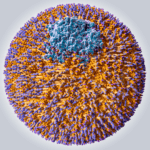
The proteins that traffic collections of lipids are called apoproteins. Once bound to lipids they are called apolipoproteins, and the protein wrapped “vehicle” that transports the lipids are called lipoproteins. Many of you have probably heard this term before, but I’d like to ensure everyone really understands their important features. A crucial concept is that, for the most part, lipids go nowhere in the human body unless they are a passenger inside a protein wrapped vehicle called a lipoprotein. As their name suggests lipoproteins are part lipid and part protein. They are mostly spherical structures which are held together by a phospholipid membrane (which, of course, contains free cholesterol). The figure below shows a schematic of a lipoprotein.
- Assisting in the structural integrity and solubility of the lipoprotein;
- Serving as co-factors in enzymatic reactions;
- Acting as ligands (i.e., structures that help with binding) for situations when the lipoprotein needs to interact with a receptor on a cell.
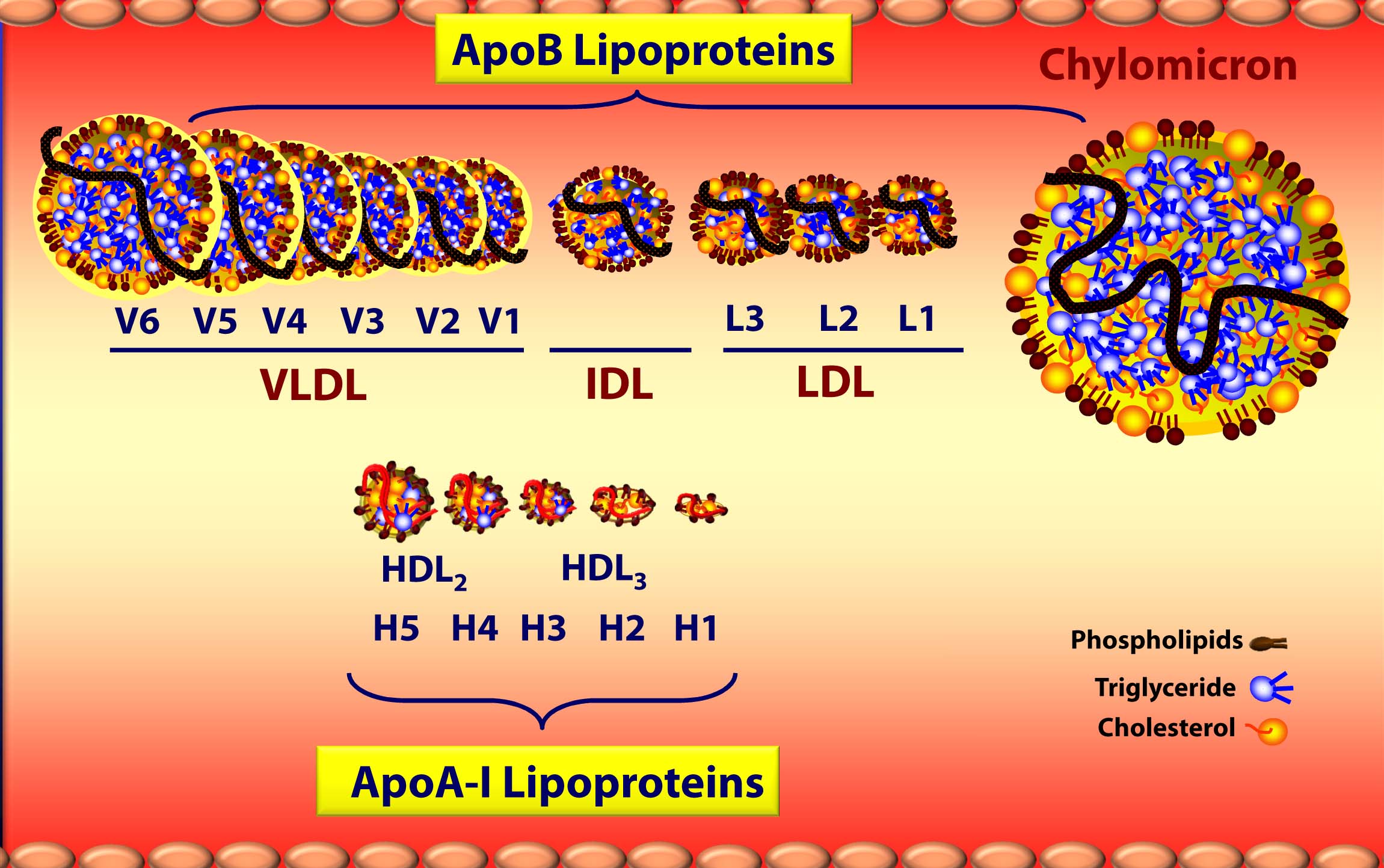
Apolipoproteins come in different shapes and sizes which determine their “class.” Without getting into the details of protein structure and folding, let me focus on two important classes: apolipoprotein A-I and apolipoprotein B. Apoprotein A-I (abbreviated apoA-I), which is composed of alpha-helicies, form lipoproteins which are higher in density. (The “A” class designation stems from the fact that apoA’s migrate with alpha-proteins in an electrophoretic field). Conversely, apoprotein B (abbreviated apoB), which is predominantly composed of beta-pleated-sheets, form lipoproteins which are lower in density. (The “B” class designation stems from the fact that apoB’s migrate with beta-proteins in an electrophoretic field.)
Virtually all apoB in our body is found on low-density lipoprotein – LDL, while most apoA-I in our body is found on high-density lipoprotein – HDL. Going one step further, the main structural apoprotein on the LDL is called apoB100 (though we often shorten this to just “apoB”), and there is only one apoB molecule per particle. It’s starting to come together now with “high” and “low” density lipoproteins, isn’t it?
But there’s actually more to it.
Everything I just described above deals with the structure and surface of the lipoprotein molecule – sort of the like the hull of the ship. But, what about the cargo? Remember what started this discussion. It’s all about transporting cholesterol (and lipids) which can’t freely travel in the bloodstream. The “cargo” of these ships, what they actually carry both on their surface [molecules of cholesterol and phospholipids] and in their core [cholesteryl esters (CE) and triglycerides (TG, or triacylglycerols)] is what we’ll now turn our attention to.
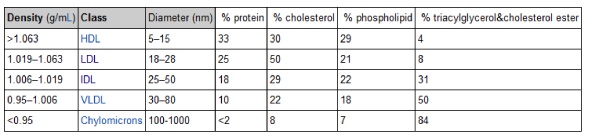
The ratio of lipid-to-protein in the lipoprotein structure determines its density – which is defined as mass per unit volume. Something that has a high density is heavier for a given volume than something with a low density. The table in this link (which I’ve also included below) shows the relative density of the five main classes of lipoproteins (from most dense to least dense) as they were originally discovered using ultracentrifugation: high density lipoprotein (HDL), low density lipoprotein (LDL), intermediate density lipoprotein (IDL), very low density lipoprotein (VLDL), and chylomicron.
Note the very subtle difference in density between the most and least dense lipoprotein – about 10 or 15%. Conversely, note the very large difference in diameter between each lipoprotein – as much as 2 orders of magnitude. Later in this series, when we start to talk about the volume of a lipoprotein particle, this difference will be amplified 1,000 times (because volume is calculated to the third power of diameter).
Below is a figure I’ve borrowed graciously from one of Tom Dayspring’s remarkable lectures which gives you a sense of the diversity of each of these classes of lipoproteins as well as the subclasses within each class. If this topic wasn’t confusing enough, there are actually multiple nomenclatures for the HDL subparticles. Originally, nomenclature was based on their buoyancy. Today nomenclature is based on the following methods, dependent on the technology used to measure them:
- Particle separation using gradient gel electrophoretic fractionation (deployed by Berkeley Heart Lab).
- Magnetic resonance assaying of lipid terminal methyl groups, called Nuclear Magnetic Resonance, or NMR (deployed by Liposcience).
- Two-dimensional gradient gel electrophoresis and apoA-I staining (deployed by Boston Heart Lab).
We’ll cover this later, but I want to point this out now to avoid (unnecessary) confusion in the figure below, which uses the first two of these.
A few things probably jump out as you look at this figure:
- ApoA-I lipoproteins (i.e., HDLs) are tiny compared to ApoB lipoproteins (i.e., VLDL’s, IDL’s, and LDL’s) [this figure is not actually to scale – the “real” difference is even more pronounced.]
- As a general rule (with pathological exceptions), as particles move from being larger to smaller, the relative content of triglycerides (TG) goes down while the relative content of protein goes up, hence the density change.
- Actual cholesterol mass is greatest in the LDL particle.
- Each specific lipoprotein has a different core make up – meaning the variable ratio of TG to cholesterol ester changes. A particle of VLDL has 5 times more TG than CE whereas a particle of LDL typically has 4 or more times more CE than TG (i.e., ratio > 4:1), and an HDL has 90-95% CE and < 10% TG in its core.
- The TG trafficking lipoproteins are chylomicrons from the intestine and VLDLs from the liver.
Deep breath. Anyone left wondering why this topic is NOT covered in medical school? I think I can conservatively say 95% to 99% of physicians do not know what you have just learned — not because they aren’t “smart,” but because this topic is simply not covered in medical school, and the pace at which the field is developing is too great for most doctors to keep up with.
Why is cholesterol concentration increasing and triglyceride concentration decreasing as lipoproteins progress from larger to smaller?
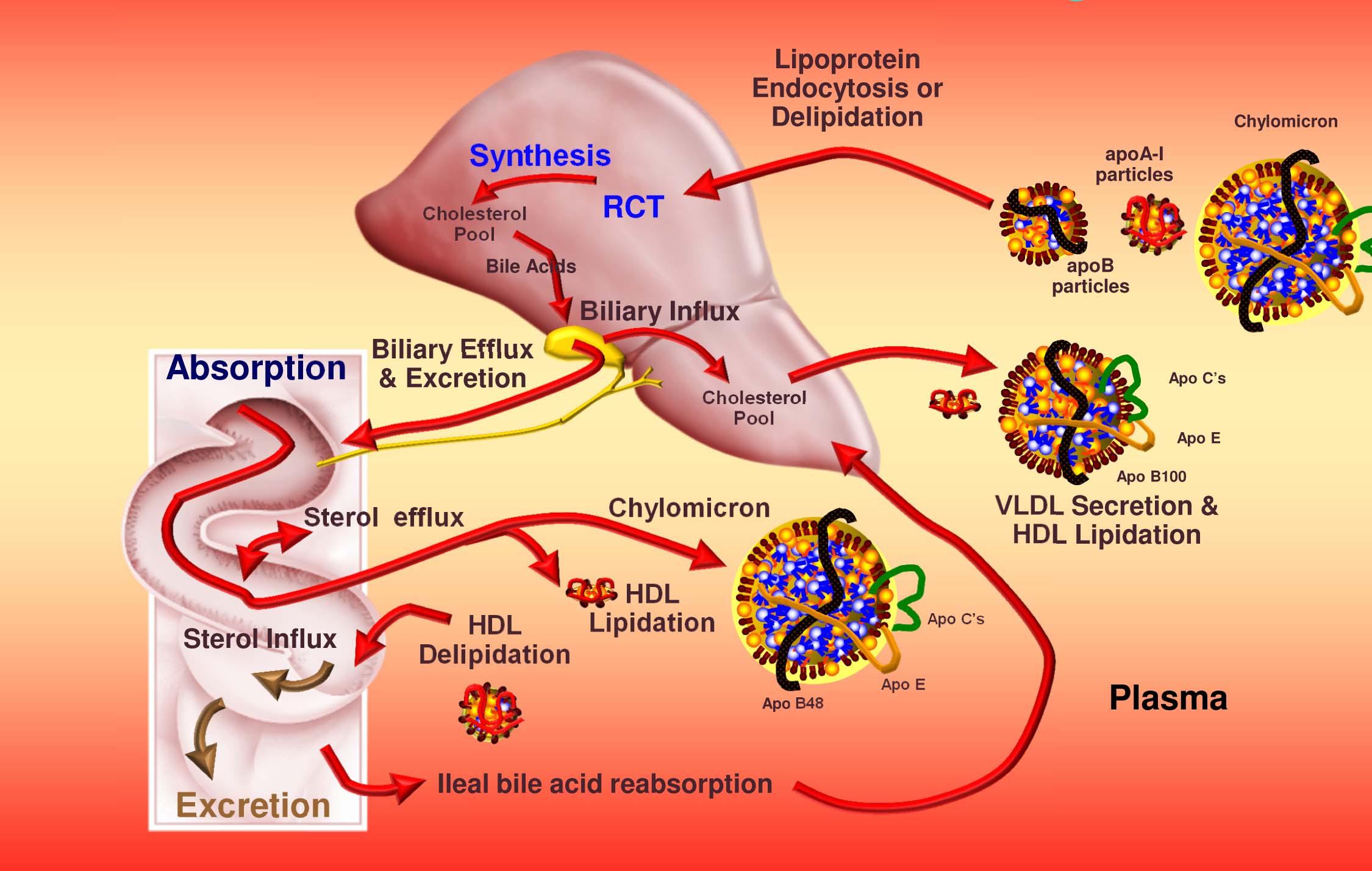
The liver exports VLDL which, after chylomicrons (used to get triglycerides to muscles and adipocytes and cholesterol from the gut to the liver) are the largest of the lipoprotein particles. VLDL particles “give up” some of their triglycerides in the form of free fatty acids and shrink as they also release surface phospholipids. Once a certain size or buoyancy is reached it is called a “VLDL remnant” and ultimately an IDL. Some (though not all) of the IDL particles undergo continued lipolysis to reduce in size and become the famous (or infamous) LDL particles. However, most of the IDL particles are actually cleared by liver LDL receptors and do not become LDL particles.
All along this process, the larger particles “shed” phospholipids and fatty acids and thus become cholesterol-rich. It is the LDL particle that is the ultimate delivery vehicle of cholesterol back to the liver in a process now called “indirect reverse cholesterol transport.” However, under certain circumstances the LDL will penetrate and deliver its cholesterol load to the artery walls. THIS IS EXACTLY WHAT WE DON’T WANT TO HAPPEN. (Sorry for the bold ALL CAPS – I know some of you may have fallen asleep by now, but I didn’t want anyone missing the punch line.) Because almost all cells in the body de-novo synthesize all the cholesterol they need, LDLs are not actually needed to deliver cholesterol to most cells.
The final important point I want to make about cholesterol transport is that it goes BOTH ways. Lipoprotein particles carry triglycerides and cholesterol from the gut and liver to the periphery (muscles and adipocytes – fat cells) for energy, cellular maintenance, and other functions like steroid creation (called “steroidogenic” purposes – remember the figure last week showing a cholesterol molecule and steroid molecule). Historically this process of returning cholesterol to the liver was thought to be performed only by HDL’s and has been termed reverse cholesterol transport, or RCT (you’ll need to subscribe — for free — to lecturepad.org to access this last link, which is well worth the time).
This RCT concept is outdated as we now know LDL’s actually perform the majority of RCT. While the HDL particle is a crucial part of the immensely complex RCT pathway, a not-so-well-known fact is that apoB lipoproteins (i.e., LDL’s and their brethren) carry most of the cholesterol back to the liver. In other words, the “bad” lipoprotein, LDL, does more of the cleaning up (i.e., taking cholesterol back to the liver) than the “good” lipoprotein, HDL!
The problem, as we’ll discuss subsequently, is that LDL’s actually do the bad stuff, too – they dump cholesterol into artery walls.
Let’s put this all together to summarize how cholesterol gets around our body
- Cholesterol and triglycerides are not soluble in plasma (i.e., they can’t dissolve in water) and are therefore said to be hydrophobic.
- To be carried anywhere in our body, say from your liver to your coronary artery, they need to be carried by a special protein-wrapped transport vessel called a lipoprotein.
- As these “ships” called lipoproteins leave the liver they undergo a process of maturation where they shed much of their triglyceride “cargo” in the form of free fatty acid, and doing so makes them smaller and richer in cholesterol.
- Special proteins, apoproteins, play an important role in moving lipoproteins around the body and facilitating their interactions with other cells. The most important of these are the apoB class, residing on VLDL, IDL, and LDL particles, and the apoA-I class, residing on the HDL particles.
- Cholesterol transport occurs in both directions, towards the periphery and back to the liver.
- The major function of the apoB-containing particles is to traffic energy (triglycerides) to muscles and phospholipids to all cells. Their cholesterol is trafficked back to the liver. The apoA-I containing particles traffic cholesterol to steroidogenic tissues, adipocytes (a storage organ for cholesterol ester) and ultimately back to the liver, gut, or steroidogenic tissue.
- All lipoproteins are part of the human lipid transportation system and work harmoniously together to efficiently traffic lipids. As you are probably starting to appreciate, the trafficking pattern is highly complex and the lipoproteins constantly exchange their core and surface lipids. This is a big reason why measuring how much cholesterol is within various lipoprotein species will in many circumstances be so misleading, as we’ll discuss subsequently in this series.
This was a bit of a tough one, so let’s stop there. Next week we’ll discuss how to actually measure cholesterol levels. In other words, if you’re looking at the river, with all its floating ships carrying their cargo, how do we measure the amount of cargo actually contained within the ships? Furthermore, is this the most important thing to be measuring? Ironically, it’s easier to measure the cargo in the ships, but more important to know the number of ships in the river. But now I’m getting ahead of myself.
P.S. Happy Birthday Dad (now I’ll know if you’re reading my blog!) [Originally posted on May 3, 2012]
Photo by JJ Thompson on Unsplash




I have benefited from increasing my fat for sure. A big however – it appears the foods you choose will certainly keep your body running. Are they healing? There are countless papers touting the benefits of plant food and their healing benefits. Fat from meat, heavy cream, salami, bacon and eggs…are not exactly repair foods.
Your diet does not seem healing at all….or is it?
Thx
What are the data supporting the healing nature of plant foods, or the absence of “healing” properties in animal products? By “data,” of course, I don’t mean epidemiological reports like the China Study, but rather actual science.
Agreed. I think we need to get away from the whole notion of foods as “nutraceuticals” – “healing benefits” of plants, “repair foods”, “harmful effects of animal fat”, etc. These are simplistic, outdated notions which just lead to fadism. In fact, human physiology is diverse enough that it can adapt to virtually any diet, so long as the essential micronutrient vitamins and minerals are provided (A, B, C, D, E, K, zinc, iron and a few other trace minerals).
Deficiency diseases are incredibly rare even in impoverished settings in Western countries. What is not so rare are diseases of overnutrition, in particular carbohydrate intolerance and excess. The question is whether replacing carbohydrates with SFA has a long-term beneficial effect on our overall cardiovascular and oncological health – I think the jury is still out on that. However, the surrogate markers look really promising (unfortunately, even diabetes is a surrogate marker, subject to an arbitrary cutpoint on the oral glucose tolerance test – a cutpoint which predicts risk for vascular events, incidentally – which is how it was chosen). I think there are some individuals who may be harmed by an excess of saturated fat and dietary cholesterol, but they are a small (yet still significant) minority. With carbohydrate replacement by fat, they will be less diabetogenic, dysmetabolic, hypertensive, and “inflamed”, but they might still develop the long-term consequences of dietary hyperlipidemia akin to that seen in genetic conditions like familial hypercholesterolemia and familial polygenic hyperlipidemia.
“…plant food and their healing benefits.”
Food is not medicine. Medicine is not food. Food is fuel. Proper fuel keeps you healthy.
Could you please list the “countless” papers (links will be acceptable)”touting” the benefits of plant foods and their healing benefits (redundancy alert)?
How do you KNOW that fats from meat, eggs, etc., are not “repair” foods? I and a lot of other people have found that they are (having stupidly avoided them for years on the advice of the USDA). On what scientific basis do you claim that they are not? (Dr. Attia asked pretty much the same thing, but he’s being polite. I don’t feel any such obligation, since he can delete my comment).
I always lump together POLITICS, RELIGION and FOOD. All three will get people crazy. I am no different – I want all the information…even the info I disagree with.
To say food is not healing counters most research I have looked at. There are vast amounts of research stating the healing benefits from food. “Food is not medicine. Medicine is not food.” Can you cure scurvy with an orange?
My question is exactly what you are asking me back – “Fat from meat, heavy cream, salami, bacon and eggs…are not exactly repair foods.
Your diet does not seem healing at all….or is it?” I have not found much stating this food repairs and heals – I may certainly be wrong here – I am simply looking for guidance.
I have increased my fat intake from 10% to 30% partly based on Dr Attia’s research. I am simply asking if this food heals and if there is research behind it?
Thank you again for all your positive contributions – I started experimenting with UCan with great results. I now train with the thought of not raising my insulin – it really seams to be working out well.
Apples
Boyer J, Liu RH. Apple phytochemicals and their health benefits Nutr J 2004; 3:5.
Jung M, Triebel S, Anke T, Richling E, Erkel G. Influence of apple polyphenols on
inflammatory gene expression. Mol Nutr Food Res 2009; 53(10):1263-80.
Wojdy?o A, Oszmia?ski J, Laskowski P. Polyphenolic compounds and antioxidant
activity of new and old apple varieties. J Agric Food Chem 2008; 56(15):6520-30.
Apricots
Enomoto S, Yanaoka K, Utsunomiya H, et al. Inhibitory effects of Japanese apricot
(Prunus mume Siebold et Zucc.; Ume) on Helicobacter pylori-related chronic gastritis.
Eur J Clin Nutr 2010; 64(7):714-9.
Fujita K, Hasegawa M, Fujita M, et al. [Anti-Helicobacter pylori effects of Bainiku-ekisu
(concentrate of Japanese apricot juice)] Nippon Shokakibyo Gakkai Zasshi 2002;
99(4):379-85. [Article in Japanese]
Bananas
Chow J. Probiotics and prebiotics: A brief overview. J Ren Nutr 2002; 12(2):76-86.
Rashidkhani B, Lindblad P, Wolk A. Fruits, vegetables and risk of renal cell carcinoma: a
prospective study of Swedish women. Int J Cancer 2005; 113(3):451-5.
Blueberries
Joseph JA, Shukitt-Hale B, Casadesus G. Reversing the deleterious effects of aging on
neuronal communication and behavior: beneficial properties of fruit polyphenolic
compounds. Am J Clin Nutr 2005; 81(1 Suppl):313S-316S.
Krikorian R, Shidler MD, Nash TA, et al. Blueberry supplementation improves memory
in older adults. J Agric Food Chem 2010; 58(7):3996-4000.
Paul S, DeCastro AJ, Lee HJ, et al. Dietary intake of pterostilbene, a constituent of
blueberries, inhibits the beta-catenin/p65 downstream signaling pathway and colon
carcinogenesis in rats. Carcinogenesis 2010; 31(7):1272-8.
Torri E, Lemos M, Caliari V, et al. Anti-inflammatory and antinociceptive properties of
blueberry extract (Vaccinium corymbosum). J Pharm Pharmacol 2007; 59(4):591-6.17
Broccoli
Kim HJ, Barajas B, Wang M, Nel AE. Nrf2 activation by sulforaphane restores the agerelated decrease of T(H)1 immunity: role of dendritic cells. J Allergy Clin Immunol
2008; 121(5):1255-1261.e7.
Le HT, Schaldach CM, Firestone GL, Bjeldanes LF. Plant-derived 3,3′-Diindolylmethane
is a strong androgen antagonist in human prostate cancer cells. Biol Chem 2003;
278(23):21136-45.
Li Y, Zhang T, Korkaya H, et al. Sulforaphane, a dietary component of broccoli/broccoli
sprouts, inhibits breast cancer stem cells. Clin Cancer Res 2010; 16(9):2580-90.
Murugan SS, Balakrishnamurthy P, Mathew YJ. Antimutagenic effect of broccoli flower
head by the ames salmonella reverse mutation assay. Phytother Res 2007; 21(6):545-7.
Carrots
Coleman AL, Stone KL, Kodjebacheva G, et al. Glaucoma risk and the consumption of
fruits and vegetables among older women in the study of osteoporotic fractures. Am J
Ophthalmol 2008; 145(6):1081-9.
Fernandes I, Faria A, Azevedo J, et al. Influence of anthocyanins, derivative pigments
and other catechol and pyrogallol-type phenolics on breast cancer cell proliferation. J
Agric Food Chem 2010; 58(6):3785-92.
Khachik F, Beecher GR, Smith JC Jr. Lutein, lycopene, and their oxidative metabolites in
chemoprevention of cancer. J Cell Biochem Suppl 1995; 22:236-46.
Nicolle C, Cardinault N, Aprikian O, et al. Effect of carrot intake on cholesterol
metabolism and on antioxidant status in cholesterol-fed rat. Eur J Nutr 2003; 42(5):254-
61.
Nurk E, Refsum H, Drevon CA, et al. Cognitive performance among the elderly in
relation to the intake of plant foods. The Hordaland Health Study. Br J Nutr 2010;
104(8):1190-201.
Garlic
Duda G, Suliburska J, Pupek-Musialik D. Effects of short-term garlic supplementation on
lipid metabolism and antioxidant status in hypertensive adults. Pharmacol Rep 2008;
60(2):163-70.
Gorinstein S, Jastrzebski Z, Namiesnik J, et al. The atherosclerotic heart disease and
protecting properties of garlic: contemporary data. Mol Nutr Food Res 2007;
51(11):1365-81.18
Yeh YY, Liu L. Cholesterol-lowering effect of garlic extracts and organosulfur
compounds: human and animal studies. J Nutr 2001; 131(3s):989S-93S.
Ginger
Ali BH, Blunden G, Tanira MO, Nemmar A. Some phytochemical, pharmacological and
toxicological properties of ginger (Zingiber officinale Roscoe): a review of recent
research. Food Chem Toxicol 2008; 46(2):409-20.
Alizadeh-Navaei R, Roozbeh F, Saravi M, et al. Investigation of the effect of ginger on
the lipid levels. A double blind controlled clinical trial. Saudi Med J 2008; 29(9):1280-4.
Park M, Bae J, Lee DS. Antibacterial activity of [10]-gingerol and [12]-gingerol isolated
from ginger rhizome against periodontal bacteria. Phytother Res 2008; 22(11):1446-9.
Priya Rani M, Padmakumari KP, Sankarikutty B, et al. Inhibitory potential of ginger
extracts against enzymes linked to type 2 diabetes, inflammation and induced oxidative
stress. Int J Food Sci Nutr 2010 Sep 28. [Epub ahead of print]
Goji Berry
Amagase H, Sun B, Borek C. Lycium barbarum (goji) juice improves in vivo antioxidant
biomarkers in serum of healthy adults. Nutr Res 2009 Jan; 29(1):19-25.
Amagase H, Sun B, Nance DM. Immunomodulatory effects of a standardized Lycium
barbarum fruit juice in Chinese older healthy human subjects. J Med Food 2009;
12(5):1159-65.
Cao GW, Yang WG, Du P.[Observation of the effects of LAK/IL-2 therapy combining
with Lycium barbarum polysaccharides in the treatment of 75 cancer patients]. [Article in
Chinese] Zhonghua Zhong Liu Za Zhi 1994;16(6):428-31.
Potterat O. Goji (Lycium barbarum and L. chinense): Phytochemistry, pharmacology and
safety in the perspective of traditional uses and recent popularity. Planta Med 2010;
76(1):7-19.
Green Tea
Cooper R, Morré DJ, Morré DM. Medicinal benefits of green tea: Part I. Review of
noncancer health benefits. J Altern Complement Med 2005; 11(3):521-8.
Dou QP. Molecular mechanisms of green tea polyphenols. Nutr Cancer 2009; 61(6):827-
35.
Mandel SA, Avramovich-Tirosh Y, Reznichenko L, et al. Multifunctional activities of
green tea catechins in neuroprotection. Modulation of cell survival genes, iron-dependent
oxidative stress and PKC signaling pathway. Neurosignals 2005; 14(1-2):46-60.19
Legumes
Itoh T, Furuichi Y. Lowering serum cholesterol level by feeding a 40% ethanol-eluted
fraction from HP-20 resin treated with hot water extract of adzuki beans (Vigna
angularis) to rats fed a high-fat cholesterol diet. Nutrition 2009; 25(3):318-21.
Kim JM, Kim JS, Yoo H, et al. Effects of black soybean [Glycine max (L.) Merr.] seed
coats and its anthocyanidins on colonic inflammation and cell proliferation in vitro and in
vivo. J Agric Food Chem 2008; 56(18):8427-33.
Yang Y, Zhou L, Gu Y, et al. Dietary chickpeas reverse visceral adiposity, dyslipidaemia
and insulin resistance in rats induced by a chronic high-fat diet. Br J Nutr 2007;
98(4):720-6.
Leafy Vegetables
Carter P, Gray LJ, Troughton J, et al. Fruit and vegetable intake and incidence of type 2
diabetes mellitus: systematic review and meta-analysis. BMJ 2010; 341:c4229. doi:
10.1136/bmj.c4229.
Hecht SS, Chung FL, Richie JP Jr, et al. Effects of watercress consumption on
metabolism of a tobacco-specific lung carcinogen in smokers. Cancer Epidemiol
Biomarkers Prev 1995; 4(8):877-84.
Kim SY, Yoon S, Kwon SM, et al. Kale juice improves coronary artery disease risk
factors in hypercholesterolemic men. Biomed Environ Sci 2008; 21(2):91-7.
Riby JE, Xue L, Chatterji U, et al. Activation and potentiation of interferon-gamma
signaling by 3,3′-diindolylmethane in MCF-7 breast cancer cells. Mol Pharmacol 2006;
69(2):430-9.
Mushrooms
Akihisa T, Franzblau SG, Tokuda H, et al. Antitubercular activity and inhibitory effect on
Epstein-Barr virus activation of sterols and polyisoprenepolyols from an edible
mushroom, Hypsizigus marmoreus. Biol Pharm Bull 2005; 28(6):1117-9.
Akramiene D, Kondrotas A, Didziapetriene J, Kevelaitis E. Effects of beta-glucans on the
immune system. Medicina (Kaunas) 2007; 43(8):597-606.
Gao L, Sun Y, Chen C, et al. Primary mechanism of apoptosis induction in a leukemia
cell line by fraction FA-2-b-ss prepared from the mushroom Agaricus blazei Murill. Braz
J Med Biol Res 2007; 40(11):1545-55.20
Lu X, Chen H, Dong P, et al. Phytochemical characteristics and hypoglycaemic activity
of fraction from mushroom Inonotus obliquus. J Sci Food Agric 2010; 90(2):276-80.
Wasser SP. Medicinal mushrooms as a source of antitumor and immunomodulating
polysaccharides. Appl Microbiol Biotechnol 2002; 60(3):258-74.
Onions
Arai Y, Watanabe S, Kimira M, et al. Dietary intakes of flavonols, flavones and
isoflavones by Japanese women and the inverse correlation between quercetin intake and
plasma LDL cholesterol concentration. J Nutr 2000;130(9):2243-50.
Kook S, Kim GH, Choi K. The antidiabetic effect of onion and garlic in experimental
diabetic rats: meta-analysis. J Med Food 2009;12(3):552-60.
Mayer B, Kalus U, Grigorov A, et al. Effects of an onion-olive oil maceration product
containing essential ingredients of the Mediterranean diet on blood pressure and blood
fluidity. Arzneimittelforschung 2001;51(2):104-11.
Wagner H, Dorsch W, Bayer T, et al. Antiasthmatic effects of onions: inhibition of 5-
lipoxygenase and cyclooxygenase in vitro by thiosulfinates and “Cepaenes.”
Prostaglandins Leukot Essent Fatty Acids 1990; 39(1):59-62.
Oranges
Heo HJ, Choi SJ, Choi SG, et al. Effects of banana, orange, and apple on oxidative stressinduced neurotoxicity in PC12 cells. J Food Sci 2008; 73(2):H28-32.
Jin YR, Han XH, Zhang YH, et al. Antiplatelet activity of hesperetin, a bioflavonoid, is
mainly mediated by inhibition of PLC-gamma2 phosphorylation and cyclooxygenase-1
activity. Atherosclerosis 2007; 194(1):144-52.
Kurowska EM, Spence JD, Jordan J, et al. HDL-cholesterol-raising effect of orange juice
in subjects with hypercholesterolemia. Am J Clin Nutr 2000; 72(5):1095-100.
Peppers (Capsicum)
Ahuja KD, Ball MJ.Effects of daily ingestion of chilli on serum lipoprotein oxidation in
adult men and women. Br J Nutr. 2006; 96(2):239-42.
Luo XJ, Peng J, Li YJ. Recent advances in the study on capsaicinoids and capsinoids. Eur
J Pharmacol 2011; 650(1):1-7.
Mori A, Lehmann S, O’Kelly J, et al.Capsaicin, a component of red peppers, inhibits the
growth of androgen-independent, p53 mutant prostate cancer cells. Cancer Res. 2006;
66(6):3222-9.21
Schumacher MA.Transient receptor potential channels in pain and inflammation:
therapeutic opportunities. Pain Pract 2010; 10(3):185-200.
Tomatoes
Bhuvaneswari V, Nagini S. Lycopene: a review of its potential as an anticancer agent.
Curr Med Chem Anticancer Agents 2005; 5(6):627-35.
Rodríguez-Muñoz E, Herrera-Ruiz G, Pedraza-Aboytes G, Loarca-Piña G. Antioxidant
capacity and antimutagenic activity of natural oleoresin from greenhouse grown tomatoes
(Lycopersicon esculentum). Plant Foods Hum Nutr 2009; 64(1):46-51.
Sedjo RL, Papenfuss MR, Craft NE, Giuliano AR. Effect of plasma micronutrients on
clearance of oncogenic human papillomavirus (HPV) infection (United States). Cancer
Causes Control 2003 May;14(4):319-26.
Silaste ML, Alfthan G, Aro A, Kesäniemi YA, Hörkkö S. Tomato juice decreases LDL
cholesterol levels and increases LDL resistance to oxidation. Br J Nutr 2007
Dec;98(6):1251-8.
Whole Grains
Murtaugh MA, Jacobs DR Jr, Jacob B, et al. Epidemiological support for the protection
of whole grains against diabetes. Proc Nutr Soc 2003; 62(1):143-9.
Lee SH, Chung IM, Cha YS, Park Y. Millet consumption decreased serum concentration
of triglyceride and C-reactive protein but not oxidative status in hyperlipidemic rats. Nutr
Res 2010; 30(4):290-6.
Okarter N, Liu RH. Health benefits of whole grain phytochemicals. Crit Rev Food Sci
Nutr 2010; 50(3):193-208.
Pa?ko P, Zagrodzki P, Barto? H, et al. Effect of quinoa seeds (Chenopodium quinoa) in
diet on some biochemical parameters and essential elements in blood of high fructose-fed
rats. Plant Foods Hum Nutr 2010; 65(4):333-8.
Slavin J. Why whole grains are protective: biological mechanisms. Proc Nutr Soc 2003;
62(1):129-34.
Anthony, have you read all of these studies? I’ll be honest with you, hell will freeze over and I will win the lottery before I will ever read a paper titled, “Epidemiological support for the protection of whole grains against diabetes.” I’m not blowing this off to be rude, but because it’s not possible for me to read and critique every study out there. That’s WHY I write this blog. I’m trying to teach YOU the principles of HOW to read them and to understand why they are of little to no value.
You’ve got some work ahead of you. I’d recommend starting with my post titled “Is red meat killing us?” Once you understand exactly these common flaws, I think you’ll have a better understanding of why I have little regard for this notion that plant diets are “healing.”
I have been studying diets for over 10 years (not in a lab but I read everything I can) – Agree to disagree on the plants front and the “benefits” from most meat, heavy cream, salami, bacon.
Blood work done every six – eight months.
Could not agree more with the controlling of insulin levels.
Thanks for the info! Looking forward to your future work.
Nothing wrong with differing views, of course. Just be sure to understand the WHY part of it. Always ask yourself, “Is the effect I’m seeing because I’ve added X, or because I’ve removed Y, or some combination of both?” All of the studies that “prove” plants are healing are not designed to answer this, so it’s very difficult to draw a conclusion. This problem is the essence of all nutrition science, but hopefully we’ll change it. Thanks for fostering the discussion.
“Can you cure scurvy with an orange?”
Of course. But if you were eating a traditional Inuit diet you wouldn’t get scurvy and you wouldn’t need the orange. Edible oranges are a cultivated crop that didn’t exist until about 2500 BCE. They weren’t available in Europe until after 1400 CE.Scurvy, though it had been known since ancient times, only became an issue when sailors on long ocean voyages had no fresh food of any kind, so oranges were the equivalent of a vitamin supplement.
The fact that you can use a plant as a treatment for something doesn’t mean that the plant is an essential preventive that must be included in the diet, otherwise we’d be trying to get more willow bark into our diet to prevent headaches.
This is actually a fantastic example, and one worth an entire blog post. I’ll add it to the ever-growing list… Thanks for flagging it. That said, I still have yet to a credible source of data to demonstrate the antioxidants in certain foods actually have any clinical impact on disease states. It’s always the same problem: Is it the presence of X or the absence of Y?
With out CONTROLLED experiments is it impossible to know. Enter NuSI….stay tuned.
Understanding what our species originally ate is the million dollar question. Our deficiencies “scurvy” could certainly be avoided by eating our “original” diet. I would argue that most diseases today are created by the very same reason scurvy was created – a lack of something or too much of something else (fast food as one example).
My argument has nothing to do with an orange – it has to do with when deficiencies are created via diet, stress, pollution etc we get sick. Fill those deficiencies in with proper food (My belief Green Food as part of it) we get better. I have seen absolutely miraculous healing via lifestyle changes (food, exercise, stress mgmt etc). We can all argue the finer points of my experiences which is OK. Me pushing my beliefs on Peter is only to get him to look at the big picture from my experiences (which is unfair)…but it was worth a shot:)
I would love to see good intelligence on what was available 10,000 years ago? Thx!
“I would love to see good intelligence on what was available 10,000 years ago?” As would I. Absent that, however, we need to use the best judgement we have today to make the best decisions we can.
Well even do there is a lot of baloney in nutritional science, there is no denying that what we eat, breath and drink has a great effect on our well being as we already know some can be pretty bad like excess fructose and sugar. There is no reason not to believe that some may be good for you including nutrient in good meat and other nutrients found in foods.
Flavonoid Compound Found in Foods and Supplements May Prevent the Formation of Blood Clots, Study Suggests
https://www.sciencedaily.com/releases/2012/05/120508124545.htm
“Rutin proved to be the most potently anti-thrombotic compound that we ever tested in this model,” says Flaumenhaft. Of particular note, rutin was shown to inhibit both platelet accumulation and fibrin generation during thrombus formation. “Clots occur in both arteries and in veins,” explains Flaumenhaft.
“Clots in arteries are platelet-rich, while those in veins are fibrin-rich. This discovery suggests that a single agent can treat and prevent both types of clots.”
Even with the use of existing anti-clotting therapies, such as aspirin, clopidogrel (Plavix) and warfarin (Coumadin), each year there are approximately 400,000 recurrent episodes among patients who previously experienced a stroke or heart attack, says Flaumenhaft.
“A safe and inexpensive drug that could reduce recurrent clots could help save thousands of lives,” he adds. “These pre-clinical trials provide proof-of-principle that PDI is an important therapeutic target for anti-thrombotic therapy, and because the FDA has already established that rutin is safe, we are poised to expeditiously test this idea in a clinical trial, without the time and expense required to establish the safety of a new drug.”
@ Anthony
how to tell which plant foods send the healing signal, and which don’t, and how to incorporate them into a LC diet:
https://www.jeffreybrauer.blogspot.com/2012/03/signaling-nutrigenomics-made-easy.html
Peter,
I’m so glad you are doing this series! I feel like you read my mind- I just received my lab work back from the doctor and my cholesterol is high. I have been working on eating a ketogenic diet, and so was confused if this was bad or not. My LDL is high, but HDL is even higher, so the doctor said I was safe. All this was so confusing and I was wanting to learn more about it, and suddenly… your blog post! Can’t wait for the next installments!
Part III should be ready tomorrow or Wednesday.
My HDL is high too – the highest my cardiologist has ever seen: 161. Yeah, HDL. They lab repeated it. My LDL is 151. He’s doing a more advanced cholesterol test, but also talking about statins.
Just wanted to say thanks for taking the time and effort to put these posts together and that I am now a regular reader of your blog! You do a great job at articulating some really tough concepts.
I hope your posts include how to increase de novo cholesterol synthesis within cells. (I presume that’s mostly a good thing?) 🙂
Hi Dr. Attia,
For the last 5-6 months, I switched over to a low carb (~50-75g/day) diet, mostly making up the calories with whey protein and lots of fats (olive oil, avocado, grass fed butter). I’m also supplementing with vitamin D and lifting weights 3x a week.
While a lot of clear markers improved, my total cholesterol and LDL jumped quite a bit, to levels that I believe you’ve mentioned you feel are high. (I’m male and I think you mentioned 220 as a reasonable limit)
What next tests or changes would you make if you were me?
Total cholesterol: 204 –> 238 * scares me the most out of all thee numbers. Most say this should be below 220.
HDL: 60 –> 70 * very nice improvement
Triglyceride: 104 –> 84 * very nice improvement
LDL: 123 –> 151 * big jump here. most docs hate to see this, but from what i’m reading LDL doesn’t mean very much – only particle size.
Triglyceride/HDL ratio: 1.73 –> 1.2 * this is considered the best predictor of cardiovascular disease. Very nice change here
Should I be worried about that 238 number?
Three letters…NMR.
Hi Dr. Attia:
Might be helpful for you to tell us what some of your mentors say about diet if cholesterol does not matter, or sat fats. This is what the Nat Lipid Assoc member dietician says in an online interview: fiber rich whole foods- fruit, vegs and whole grains! Substitute mono and poly fats for sat fat.
https://www.reachmd.com/xmsegment.aspx?sid=6548
They agree these guidelines are based on dogma not rigorous science.
At the top of Cho II it says 112 comments, but scrolling down I cannot get beyond #48
The 112 includes all of the sub-comments.
Dr. Attia, three weeks after a carotid endarterectomy my LDL-C has spiked. Is an increase in LDL-C a normal healing response to such surgery?
Good question. I do not know the answer.
Hello, again. I am curious to know your thoughts (if any), in a nutshell, about bulletproofexec.com? This site and the lifestyle it supports is quite Paleo in nature and also argues against high carbs/bad carbs. As always, thank you for sharing your knowledge, thoughts and inspiration!
I have not read it.
Any website that advocates adding a stick of butter to your coffee gets two thumbs up from me…
Peter – Interesting bit in the NYTimes today. Although they still don’t get it, there is some evidence in their model that points in the right direction, though they don’t seem to understand the cause/effect (e.g. insulin sensitivity/metabolic syndrome).
https://www.nytimes.com/2012/05/15/science/a-mathematical-challenge-to-obesity.html?_r=1&hpw
“That the conventional wisdom of 3,500 calories less is what it takes to lose a pound of weight is wrong. The body changes as you lose. Interestingly, we also found that the fatter you get, the easier it is to gain weight. An extra 10 calories a day puts more weight onto an obese person than on a thinner one.”
That IS interesting, although I don’t believe for one second they’ve succeeded in creating a “single equation” that can accurately predict anyone’s weight response. Starting with the flaw that their prized simulator overestimates the daily caloric intake that makes me weight-stable by about 1000 calories! (I wish…)
I think the statement “an extra 10 calories a day puts more weight onto an obese person than on a thinner one” is of the kind that makes Gary Taubes nuts.
Getting ready for Part IV by re-reading the series (and also took an initial stab at Dr. Dayspring’s cholesterol synthesis slides at Lecturepad).
A question which has bugged me from Part I and is related to this post as well is: why is cholesterol which is excreted via the biliary pathway reabsorbed? Is this just a product feedback thing, or does this only happen pathologically?
Ready for Part IV: Hit me!
Reabsorption is 100% necessary and normal. Only when out of balance is it a problem. Part IV coming soon…
Thank you for all you do, Peter. You’ve opened up a whole new area of interest & study for me – it’s absolutely fascinating. Also love Lecture Pad & the Lipid Center sites.
I have a question about point #4 in your information below the figure depicting the various sizes of lipoproteins. Should not the ratios of VLDL’s say (5:1) 5 times more TG to CE & LDL’s (4:1) 4 times more TG to CE, rather than saying CE to TG? I’ve just read something by Dr. Dayspring that said VLDL’s have 5 times more TG than CE.
In a VLDL particle TG is > CE; In an LDL particle, this is reversed. See the table in part II of this series. Let me know if I’ve misrepresented this fact somewhere.
I’d like to add additional information about cholesterol and you will find it here – https://articles.mercola.com/sites/articles/archive/2010/08/10/making-sense-of-your-cholesterol-numbers.aspx
I studied as a Medical Technologist and we were never taught any of this in Clinical Chemistry, which would have been very interesting to me. And I have to agree with the statement about doctors;I worked at JHH, and we taught alot of the doctors( residents).They are bombarded with so much information at once that it’s very hard for them to learn in a “crash course”. Being on both sides, as a transplant patient and a Med Tech, I have become more aware of my health.
Thank you, Dr. Attia.
Jay, I wonder if we ever overlapped when I was at Hopkins? I was there 2001 to 2006. Did lots of stuff on transplant with some great folks.
Maybe Peter, I was there 2000-2005, and worked in the Microbiology Lab; it’s a big place but possible. I met many great folks there as well.
I have a question. From your experience, would it be possible to have an effect on my lipid levels while being on the various meds for transplant? Just curious if might have a general idea.
Thanks, Jay.
I would suspect transplant meds can likely have an impact on lipid and lipoprotein levels, though I can’t confirm that off the top of my head.
Hi Peter,
Loving this series but I’m confused about statement 4 under the figure of different lipoproteins:
Each specific lipoprotein has a different core make up – meaning the variable ratio of TG to cholesterol ester changes. A particle of VLDL has 5 times more CE than TG whereas a particle of LDL typically has 4 or more times more CE than TG (i.e., ratio > 4:1), and an HDL has 90-95% CE and < 10% TG in its core.
Don't the ratios stated above mean that VLDL is 83% CE and 17% TG, and LDL would be 80% CE and 20% TG? Why would VLDL have more CE, if cholesterol concentration increases as the size of lipoprotein molecule decreases?
Great catch, Tina! Thank you. VLDL has 5 times more TG than CE. Corrected.
Peter,
Thank you so much for this series. It’s going to take many many re-reads to begin to comprehend all this even though you have a gift for making the complex comprehensible. I look forward to understanding this on a deeper level as fat and cholesterol have played a key part of my recovery from the damaging effects of celiac disease as well as the secondary complications of severe rheumatoid arthritis. I eat high fat and on most days eat upwards of at least two dozen raw eggs as a crucial part of my recovery. I am not a biochemist nor am I trained in the medical sciences and so I sometimes go off on poorly informed goose chase tangents of speculation. I wondered aloud to myself as others were trying to figure out the mechanism of cholesterol plaque deposition on artery walls if there might be some sort of similar mechanism to the phenomenon of leaky gut. I cannot even begin to propose a mechanism for why this might be. I do know that lectin content in food was contributing to my leaky gut syndrome allowing all sorts of things into my circulation when my gut damage was severe and my systemic inflammation was so out of control . Would there be some inflammatory response in the arterial walls that would mimic the loosening of junctions in the gut wall thus making arterial walls more susceptible to deposition of cholesterol plaques, perhaps even regardless of particle size (although I do suppose there would be a prevalence of small particles just by mechanical limitations?) I know that when systemic inflammation was widespread, I was experiencing what I was told was permanent joint damage and that by eating lots of eggs and coconut oil while being very low carb I have actually reversed the joint damage and my last dexa scan numbers were much better than baseline three years ago and follow up two years ago. The only thing that has my doctor worries is my LDL number.. which I am not at all concerned about. Funny, he kept on congratulating me for making such incredible progress in all markers (including being an inch taller at my last dexa scan) having great numbers all around and looking better and being able to do things like walk again.. but when he looked at the LDL number immediately went the statin route. I politely told him I was not at all interested since they keep arbitrarily moving the numbers lower and that I am just fine. He had no response other than to tell me to keep up the good work. Sorry to be long winded but I will try to study harder and come up with a hypothesis for the leaky arterial wall theory over time. Thanks again for your incredible contribution.
Hi Charles –
Just a thought, based on years of personal experience, that your celiac disease, “arthritis” and leaky gut may be related to chronic Lyme disease. I thought I had celiac disease, but when I got successfully treated for Lyme disease, it went away. I now live virtually carb-free at this point, but that’s a different story.
My two sons also had chronic Lyme for many years. Fortunately it appears to be in remission for the time being. If you do look into this, trust me when I tell you that the medical community’s approach to this devastating disease is no better than the convention wisdom regarding diet, blood lipids and heart disease. You have to do a lot of research to home in on the truth.
Good luck.
There is an error in your page’s code on line 336 column 1128. There quotation mark is on the wrong side of the semi-colon. For quick reference it is in the link that is prefaced with the words “you’ll need to subscribe — for free — to”. The error causes a full paragraph of the article to be hidden from the viewer.
Came here via Mark’s Daily Apple. I am liking this version much better than the summary on his site. When reading it on his I could tell that things were being cut short to make it fit into 2 posts, and the added information here is filling out the gaps that i perceived quite nicely. Thanks for this fantastic write-up.
Nice catch, Joseph! Thank you. Should be fixed now.
Semi-irrelevant question, but it bugs me and I’m hoping someone can answer. This whole lipoprotein thing is necessary because fat is insoluble in water. But — how do you explain milk? Cream in coffee? I pour whipping cream into my coffee, and it seems to blend in nicely to make a smooth, consistent light brown liquid. Yet if I’d poured olive oil into water I’d get these unsightly globules floating around like a lava lamp. What’s the deal with fat in milk?
The fat is protein bound. So the proteins, like albumin, act like the lipoproteins and proteins in our plasma.