If you’re reading this, you probably know that I’m obsessed with longevity. But to really understand longevity, you must understand metabolic health, insulin resistance and, by extension, one of its end-results: type 2 diabetes (T2D). Though my medical practice does not focus on type 2 diabetes, I have taken care of several patients with T2D over the past few years. When I was in medical school I was taught many things about T2D, but one stands out most: T2D is incurable, I was told. Once you have it, you’ve always got it, and the best one can do is “manage” it as a chronic—but irreversible—condition.
But is this really true? Asked another way, is T2D reversible?
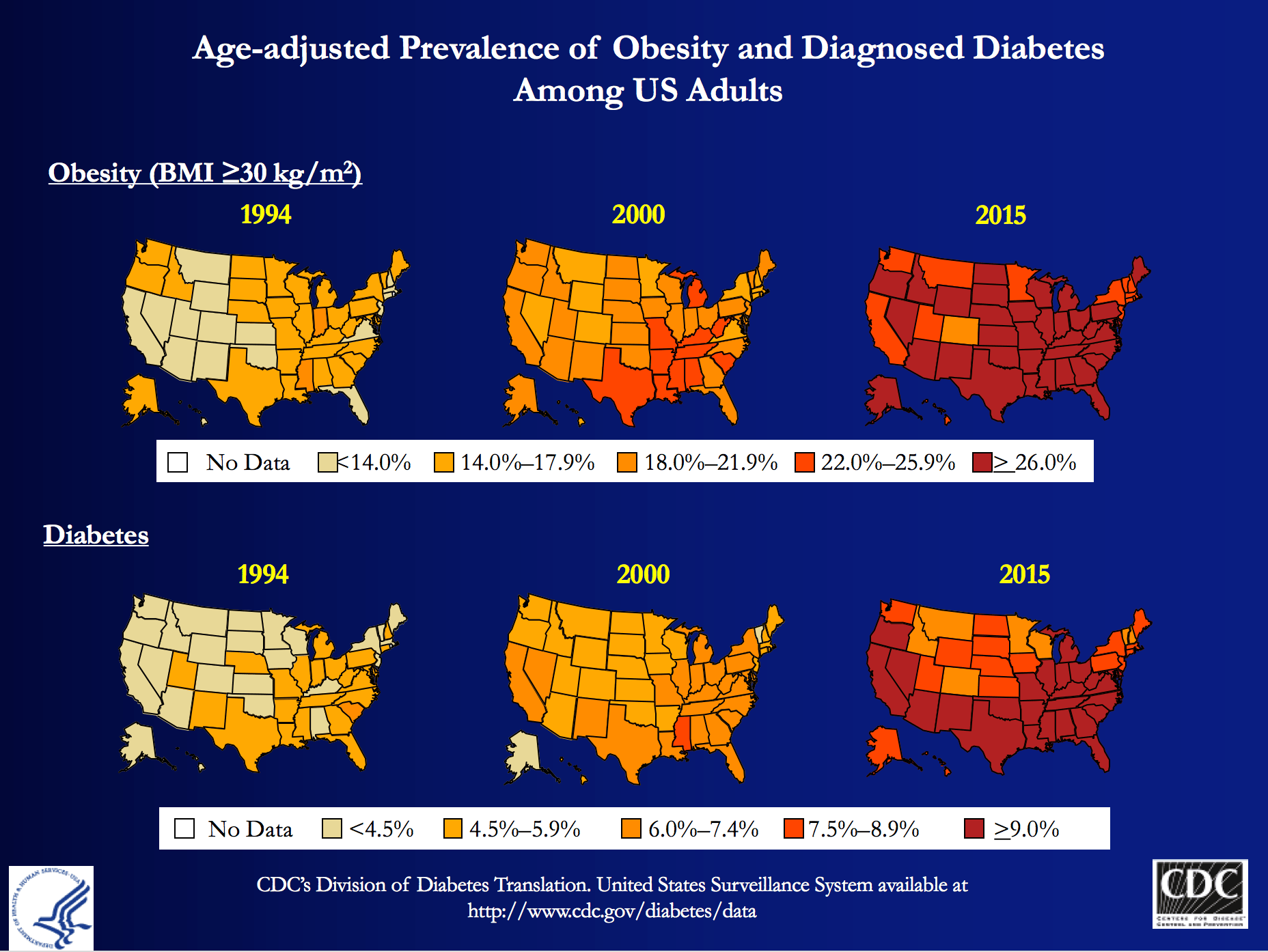
My obsession is partly due to my personal journey to better metabolic health, which I’ve documented elsewhere on this blog, and spoken about publicly. But those facts alone, don’t fully explain why I wanted to be involved with Virta Health (I’ll get to them shortly). T2D is a massive societal problem that has the potential to literally bankrupt countries: More than 29 million Americans have T2D and more than 80 million are pre-diabetic. And whether you view it through the lens of population health, or the lens of an individual patient, T2D is perhaps the biggest healthcare challenge of our generation.
At the population level, T2D costs Americans more than $300 billion per year: one of every three Medicare dollars is spent on T2D, and one of every six healthcare dollars is spent on T2D. At the individual level, patients and payers (employers and insurance companies) spend thousands of dollars (often more than $10,000) in annual expenses for medications and procedures with significant side effects, and much higher risk of developing cardiovascular disease, cancer, Alzheimer’s disease, blindness, amputation and kidney disease.
The traditional approach—which is clearly not working—is to “manage” this chronic condition with medications and the ever-ubiquitous “eat-less-avoid-fat-exercise-more” lifestyle interventions. At best, this approach only slows down the progression of the disease. Furthermore, many diabetes drugs have their own side-effects and diabetes management has a dismal diabetes reversal rate of about 1%. To date, the only clinically proven way to reverse T2D has been bariatric surgery, which is costly and not without risk. If one great thing has come from bariatric surgery, besides the obvious help to those have been successfully treated, it is that any physician or scientist paying attention to the results can’t help but notice that the reversal of T2D in these patients post-operatively seems uncoupled from their weight loss. In other words, adiposity, while correlated with T2D, is not likely the cause.
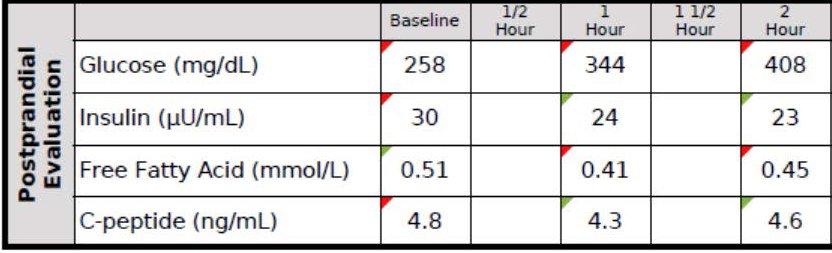
Every doctor has his (or her) “Patient 0”—the one who really got him (or her) thinking. I’d like to introduce you to mine, RB. When I met RB, he was a 37 year-old Mexican man with a family history of T2D who had a “high” glucose level on a screening blood test. His two-hour oral glucose tolerance test (OGTT) is below.
You don’t have to read these for a living to see this isn’t ideal. As you can see, his fasting glucose was 258 mg/dL and his fasting insulin, 30 uU/mL. When given 75 g of glucose, his glucose rose to 344 mg/dL at 60 minutes and 408 mg/dL at 120 minutes, all the while his insulin level fell from 30 to 24 to 23. These numbers alone confirm the diagnosis of T2D. But if we needed more evidence, his HbA1C was 9.7%, corresponding to an average blood glucose of 232 mg/dL (today the diagnosis of T2D is defined by HbA1C >= 6.5%, but I much prefer to use OGTT).
Ordinarily, for a patient with this degree of disease and beta-cell fatigue, I would have opted for at least two drugs, metformin (cheap) and a DPP4 inhibitor (not cheap) and most doctors would have gone straight to insulin, as well. However, due to the patient’s financial circumstances, we opted to only use metformin and dietary modification. The patient worked very long hours in construction and, frankly, was pretty much exercising all day, so there was no way adding more exercise to his day was going to work. If we were going to fix him, it had to be through nutrition. I spoke with one of my mentors, Dr. Naji Torbay, a remarkable endocrinologist who has the largest diabetes reversal program in Dubai and Lebanon, about this case. Even he thought it would be tough, but he’d reversed cases like this, so we gave it a shot.
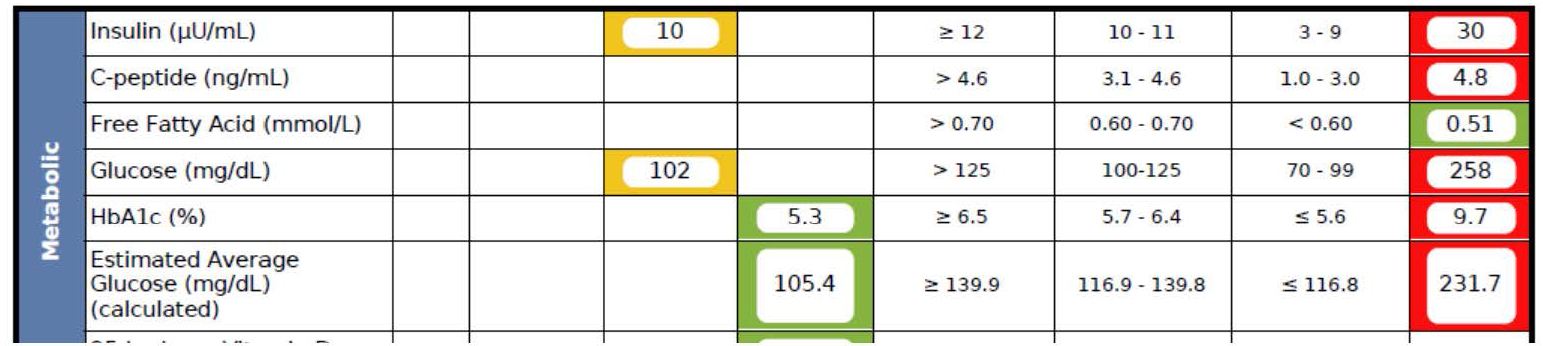
What happened over the next 5 months surprised me, as even I did not anticipate the alacrity of RB’s reversal. Below is a snap shot of RB’s labs from March 1, 2016 about 5 months after the OGTT, above. On the right side you can see the results from September 28, 2015, including the HbA1C of 9.7%, the fasting glucose of 258 mg/dL, and the fasting insulin of 30 uU/mL (HOMA-IR calculated at 19.1).
As you can see, the HbA1C fell to 5.3%—that’s even below the threshold of pre-diabetes—and the fasting glucose and insulin fell to 102 and 10, respectively (HOMA-IR calculated at 2.5).
RB doesn’t have diabetes any more. RB will avoid the amputations that destroyed the lives of his family. RB will not die prematurely from heart disease in his 50s. RB got a new lease on life.
If you think I’m telling you this story to impress you, you’re mistaken. Countless doctors (though not enough) know how to do what I did with RB—it’s actually simple biochemistry, and if a former surgeon like me can learn it, certainly anyone can, as long as one has the ability to frequently and safely manage medications and guide necessary behavior change. But sadly, most people like RB don’t have this option, and even if I and countless other doctors devoted the rest of our lives to helping everyone like RB out there, we could not put a dent in this problem, which is where Virta Health comes in.
Disclosure: I am an advisor to Virta Health and I have invested in the company, because I believe their approach is the best one to solve this problem—not the other way around.
Is it possible to deliver systematic diabetes reversal results (like the case above) safely, sustainably, and at scale among average diabetics?
Of course, even with the correct biochemical/nutritional approach, there are number of challenges to make T2D reversal possible at scale:
- Eliminating diabetes medications safely requires day-to-day (not monthly) careful adjustments by a physician. This is not how physicians work and would not be cost-efficient.
- Anything nutrition related requires a very high degree of individualization based on health status, lifestyle preferences and other life circumstances. For the 1% DIY’ers (who probably disproportionally read blogs like this one) any extreme approach can work, but at a population level, it won’t be enough.
- Both the patient and physician would need near real-time biomarker (e.g., CGM) data to adjust meds and the overall intervention. [By the way, I get asked all the time—mostly on Twitter—what CGM is…for those about to ask, here you go.]
- All behavior change and lifestyle interventions have failed at scale because only a small fraction of the population is able to DIY through complex decisions in today’s environment and life circumstances. This would require a near real time “personal coach” who can address any situation (e.g., family struggle, travel, new job, holidays).
It appears that we may be a step closer to somebody solving this challenge. Today, the first results of a T2D reversal clinical trial were published in the Journal of Medical Internet Research that show a promising new way to look at T2D: it is reversible in a large percentage of average patients, safely and sustainably. The trial was conducted by Virta Health, an online diabetes reversal clinic, which uses technology and artificial intelligence to solve the above mentioned care delivery challenges. The entire intervention is managed by physicians and the nutritional approach is based on highly individualized carbohydrate restriction and nutritional ketosis (which I’ve written about extensively in the past and throughout this blog).
The trial took place in Lafayette, IN, in partnership with Indiana University Health. A total of 262 women and men with T2D enrolled in the Virta Clinic. Average age was 54 (Stdev: 8); BMI 40.8 (Stdev: 8.9) and two-thirds of the patients were female. The trial will continue for at least two years, and data from the first 70 days were published today.
After just ten weeks:
- 56% of the diabetics enrolled achieved an HbA1C below the diabetic range (6.5%), while eliminating hypoglycemic medications
- Almost 90% of insulin users had it either completely eliminated (close to 40%) or reduced
- Mean body mass reduction was just over 7%, which is quite significant, but also shows that diabetes can be reversed before massive weight loss (i.e., it’s not the obesity that causes type 2 diabetes, which is consistent with the gastric bypass literature)
- Patient completion rate was >90%, which is remarkably high in an outpatient-based intervention.
- Reported feelings of hunger decreased from the pre-trial level (this seems to be a strong indication that will-power driven caloric restriction was not a factor in weight loss)
- Importantly, there were no serious adverse events, no incidence of symptomatic hypoglycemia, and no incidents of ketoacidosis.
The trial is ongoing with one-year data expected to be published shortly.
Yes, this is only one clinical trial and 70 days is not very long, but these data force us to consider that there is another way to look at T2D: it is not a chronic condition that gets progressively worse. With the combination of the right science and technology, it can be reversed at scale and among average diabetics. Clearly we need to look at the long-term success, and see many more patients succeed safely, but this is more promising than anything I have ever seen. I’ve seen some of the preliminary 1+ year analysis and the results look very impressive. I look forward to sharing them as they become publicly available.
If you are interested, you can learn more about Virta and their diabetes reversal science here. I’m excited to be a very small part of this organization and I look forward to the day when every patient with T2D at least has the chance to try an approach that can potentially reverse their condition.





Boom
No…… KBoom
Peter – great to see this happening . I am a family doc and have been trying to do this on my own sans software and tech. Looking forward to hearing more about and from Virta .
Soon as you mentioned Indiana I thought Sara Hallberg could be in on this . Saw her on the website along with Volek and Phinney . These are the folks I learned LCHF methods and approaches from.
Thanks for the update.
We front line, conventional structure practices need all the help and encouragement we can get. – very much like the “average ” patient
Thanks again
Mike
Great to hear, Mike. Sara et al. have done excellent work, and this is only the beginning.
Agree with Mike completely, I’m also a family doc and have been able to cure diabetes in the motivated patient with similar recommendations. Its incredibly gratifying to achieve such results especially at very low cost for my patients. Thanks for all sharing this article and thanks for all you do!
Thanks for the article, Peter.
I am wondering, I’ve seen plenty of people go low-carb and reduce their HbA1C, blood glucose levels and so on and say they’ve “reversed diabetes”. However, T2D is basically carbohydrate intolerance, can a low-carb diet fix it? If these people started eating lots of carbs again, would their problems come back? If you need to stay on a low-carb diet for the rest of your life, I don’t think you’ve cured/reversed diabetes.
On another note, since you’re mentioning bariatric surgery, here’s a few studies. They suggest bariatric surgery affects intestinal microbiota, intestinal barrier permeability and thus how many bacterial endotoxins (LPS) get through into the bloodstream to cause inflammation. There might be a very strong connection between gut microbiota/plasma LPS and diabetes.
https://www.ncbi.nlm.nih.gov/pubmed/23835694 – Plasma lipopolysaccharide LPS is closely associated with glycemic control and abdominal obesity: evidence from bariatric surgery. reduced LPS levels after bariatric surgery were directly correlated with a reduction in HbA1c. Our findings support a hypothesis of translocated gut bacteria as a potential trigger of obesity and diabetes, and suggest that the antidiabetic effects of bariatric surgery might be mechanistically linked to, and even the result of, a reduction in plasma levels of LPS.
https://www.ncbi.nlm.nih.gov/pubmed/27228236 – Bacterial Lipopolysaccharide, Lipopolysaccharide-Binding Protein, and Other Inflammatory Markers in Obesity and After Bariatric Surgery. LPS and LPB decrease after bariatric surgery. LPS receptor CD14 and mRNA expression toll-like receptor 2 (TLR2) and toll-like receptor 4 (TLR4) also reduce following surgery. Changes in LPS and LPS components after bariatric surgery are shown to be linked to the surgical technique of the procedure and restriction of caloric intake
https://www.ncbi.nlm.nih.gov/pubmed/24713521 – Bariatric surgery significantly decreased the serum level of LBP. Serum LBP levels were higher in obese patients than in the normal weight patients (49.9±15.7 vs 25.2±7.5 ?g/mL) at baseline and significantly decreased to 35.1±22.6 ?g/mL after bariatric surgery.
Commenting about microbiota , i would like to know Dr Attia’s viewpoint . I had to do some study on the subject and most of the articles i read were comming to the same conclusion, when you eat mostly vegetables, cerals and short amounts of meat , the Bacteriodetes increase over Firmicutes and on the contrary , experiments eating only meat, chease and animal products increase the Firmicutes which are found in obese people. More variety of species are found in the “green” diet also
I have been 2 years on ketosis and everytime i try to give up fat and add up more vegetables (sound healthy,uh?) I gain some weight. I lost 22 pounds with the keto diet very easily, but what about my microbiota, what does it prefere for luch?
i would appreciate your comment Dr.
carnivourus vs green https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3957428/
Study with Burkina Fasso Vs Italian Kids https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2930426/
Longer discussion. I’m not especially impressed, though, at the causal relationship.
I am also curious if it is necessary to make a distinction between reversal and remission of type 2 diabetes. I had been under the assumption that long-term/permanent remission is possible but that reversal is not. I assume reversal would imply normal blood sugar even when eating more carbs then in ketosis (although less than SAD diet)?
Great stuff. If I may, I just wanted to point out to those folks that state that diabetes cannot be reversed, I’d encourage them to look up the words “reverse” and “cure” in the dictionary. Reversal is not the same as cure. The word “reverse” is associated with a temporary state, whereas “cure” is associated with a permanent state. As a type II diabetic following a low-carb way of eating, my diabetes has been reversed, but not cured. Were I to abandon a low-carb way of eating and go back to a high-carb Standard American Diet, my reversal would stop, and the disease would progress once more.
So diabetes can be reversed with a low-carb diet, with the reversal dependent upon one’s adherence to a low-carb way of eating. I hope this helps clarify the matter for some folks!
Bro –
You complete me. I’m happy to see you post more and get out on the Interwebz with some hustle. Have you looked at Roy Taylor’s research on the PSMF (protein sparing metabolic fast) / Ketogenic crash diet?
He’s written some interesting stuff, people are even able to get back to moderate carb diets once they are done. Here’s a 6 month follow up from his crash diet:
https://care.diabetesjournals.org/content/early/2016/02/24/dc15-1942.short
Hi Dr. Attia, I believe you previously commented on preferring to build a small number of Ferrari’s with your nuanced longevity work vs. undertake the challenge of more population-based health. If that’s accurate, has your mindset shifted and any particular trigger for such a shift?
No change.
Fascinating. I love this. Did they look into mechanism of action here…upregulated glucose transport or pancreatic cell regeneration or anything like that in this study?
Not in this study.
Hi Ben,
IIRC – which I may not – Ludwig remarked in one of his many talks that once the insulin is normalized & the inflammation stays down, some folks actually do heal at both beta cell & hypothalamus. Others for unknown reasons aren’t that lucky. Maybe you could get him to talk more around his thoughts & experience with this and what the mechanism could be.
George J… The University of Mass Med Centre… ooops… “Center” did a study not long ago that showed that a MODERATE amount of ? cell stress signals them to “proliferate”.
I SUSPECT that if you reduced “Standard American Diet” stressors beyond simply glycemic load, such as wheat (which, oddly, has a higher glycemic index than sugar/glucose) and were stringent in sticking to a Nutrient Dense, Ancestral Diet (I did not want to say “paleo diet” per se) but walked a tightrope between Ketogenic and a modest-carb load then the “stress” might be… hmmm… optimal, possibly, maybe?
All very interesting, Peter! Thank you.
Hi Peter,
Great success for RB.
1. I wanted to ask if an OGTT was done post intervention as OGTT doesn’t look good while in ketosis for many folks?
2. For diabetics, perhaps there is no other choice than ketosis, however, as you have said not everyone responds well to ketosis, have you come across non-diabetic folks whose glucose tolerance gets worse with dietary fat especially saturated fats? If so what’s the counter strategy?
Thanks
1. OGTT was done in ketosis
2. Longer response needed…but can’t do now.
Im also in the camp of having really high blood glucose while being on ketosis (fasting glucose alway higher than non-fasting, another oddity). Count me interested on any answers you might have…
Hi Peter,
What’s your opinion, or what resource would you point me to regarding the following about prediabetes?
(patient is a 36yr, normal weight individual (5’9/160lbs). A1C 5.6%, fasting between 98-105. Post-prandial numbers range from 120-170 depending on carb amount. 23andme showed the TCF7L2 gene). Fairly sedentary lifestyle, though hits the gym 2x a week for light cardio (20min) + some lifting. Eats lower carb, but not super low carb. (Maybe 120g per day?). First noticed the high fasting at age 28 and A1C seems to have been stable since then.
1. In prediabetes, are beta cells already dead, or is it still simply a state of insulin resistance?
2. For someone this young-ish, would you jump on metformin early? 2 endos recommended “just watching it”.
3. Do you believe it’s actually fully reversible, or only temporary? (Reading the articles you’ve posted now for more info)
There is of course room here for more exercise that can help, but there are obviously other genetic factors influencing things as well.
The next thing I plan to try is some 2-3 day fasts per Dr Longo.
I have a very similar situation. Just 3 days of IF (8 hr feeding window, with a little coffee but no food making it 10 hr) brought me to normal FBG (80-85) reliably in 3 days (from 95-108). Something Rhonda Patrick said about the body expectIng 12 hr downtime clicked with me, as i was only consuming very small amount of food outside say 10hours but over years of that apparently even this small shift has done a lot. It’s been about 2 months and I am planning to look at postprandial soon.
Hello Peter,
I enjoyed your visit on Patrick O’Shaughnessy’s podcast. When discussing caloric intake/disposal, your referenced an “oral glucose tolerance” test as one the five important tests people should have run. What are the other four tests?
Thanks,
Matt
Lp(a)-P, LDL-P, IGF, apoE genotype, but so many more, of course…
I’m excited to see what these guys roll out. One question about the study, though. What’s the deal with CRP?!
Would Virta be able to help Type 1 diabetes patients?
You’ll need to ask them.
One quick comment, Peter. I noticed you made a couple references to the chicken-and-egg problem when it comes to diabetes vs. body fat/obesity. Does it really matter which causes the other? Just about any successful treatment for T2D will reduce body fat to some degree, and weight loss will improve insulin resistance and lower blood sugars in diabetics without any other treatment (unless you consider caloric restriction itself the treatment). It seems like a moot point to argue one way or the other regarding which causes which, because they are so tightly interrelated. Maybe it’s interesting from a biochemistry perspective, but I think it’s somewhat of a distraction from the real issues. I’m not asking this question rhetorically – perhaps there is a reason why it is important to make the argument whether body fat increases insulin resistance or whether insulin resistance leads to increased body fat. In my opinion it could be one or both depending on the individual. I just don’t see the reason for distinction when the treatment in both cases is so similar.
I think it does matter because while your observation is correct–most people lose weight when resolving IR/T2D–the cause/effect confusion results in many patients being told to lose weight via methods with lousy efficacy (eat less, exercise more vs. eat less of certain foods…).
Given your knowledge today, would you have made the same decision to do a surgical residency at Johns Hopkins? As I am learning late in life, sleep deprivation has many bad consequences, more noticeable in the short term (reduced fine motor skills, memory loss, poor decision making), but also longer term (weight gain, hypertension, depression). If not for yourself, how would you mentor or advise a younger engineering or medical student on what would be a healthier career choice than slogging through a medical residency? Asking for a friend! I’ve enjoyed your blog and video and podcasts.
Impossible to say.
I look forward to the economic implication analysis hinted at in the second to last paragraph of the JMIR report. Needed to achieve widespread adoption and spur competition. In the works?
I wonder what MED of support team (and other overhead and back-end costs) will be possible in coming years. How much of the necessary adjustments can be diverted to automatic algorithms, and how much will still require a clinician? On a related note – some experienced T2DM pts largely manage their own insulin dosages and check in with their docs here and there – surely that is a more dangerous proposition than taking care of one’s own BHB and blood glucose with the help of a smart app. What kind of supervision taper can be expected?
Anywho, exciting stuff. Thanks for the write-up. Saw Dayspring’s tweet, read the paper, glad to see an insider’s view.
The answer is simple: we have to get off our butts and move more through the day, say NO to processed junk food and take a few core supplements like vitamin d3 and k2 and probably magnesium. It’s really that basic. Unfortunately,
too many are addicted to crap living.
I don’t think RB could have moved much more, Jay…
Can you get any more granular wrt to RB’s treatment by you?
Did you manage RB’s glucose with CGM? Did you see him every 48h?
Did you inform what to and what not to eat?
Do you think he could have achieved this success via diet alone? Is it more about having that constant cheerleader influence (ie Peter Attia – sort of a kinder Gunnery Sergeant Hartman).
No CGM, just frequent finger stick. Very clear dietary recommendations, consistent with this paper.
I must be confused…why are insulin levels decreasing as blood glucose levels rise if the patient is insulin resistant? Shouldn’t he be producing MORE insulin to cope with the glucose load given for the test?
Yes, he should have, but in late state T2D the beta cells get fatigued.
As someone who sells a DPP4, this brings great joy to me. I’m constantly harping on diet/exercise but the reality is the patients aren’t receiving the correct information. From obese endocrinologists to Dietician’s still preaching low fat I don’t see this improving much. Many of the clinical trials that support these agents both in the DPP4 class and outside the class are extremely weak. Most data shows on average a one point drop in A1C accompanied with a slew of side effects you have mentioned along with many others. It’s encouraging to see yourself and a company like virta showing strong results and sharing the truth. Keep up the outstanding work Peter.
Thank you, Sam.
Great post.
Love the “link” to explain the CGM!
A not-so-subtle hint.
So glad someone got that… If I had a dollar for every time I was asked.
Were RB’s excellent numbers at 5 months while still on metformin? I’ve heard of some people taking metformin just for a longevity benefit, even with no obvious blood sugar issues.
My own n=1:
I was informed that I was prediabetic, weighed about 200 lbs, fasting blood sugar around 100, AIC around 6.4. I went on a low carb ( but probably not ketogenic) diet and lost about 40 lbs. While I was losing weight, my AIC and fasting blood sugar were pretty good. Fasting blood sugar got down to maybe 85-90, and I had a few AIC readings in the 5.5-5.7 range.
However….. once my weight loss stopped (I hit the dreaded plateau), my fasting blood sugar drifted back up toward 100, and my AIC drifted back up to 5.9 – 6.0. In retrospect, it seems like it was the calorie deficit that really helped. Once my weight loss stopped, it seems like my liver still wanted to pump out too much glucose. So I’ve wondered if a low dose of metformin might be something to consider (knowing of course that you can’t offer me medical advice).
As a post script: I did drift off the low carb diet, and eventually regained most of the weigh. Some came back as fat, some as muscle, largely from following the Starting Strength program. With the weight regain, my numbers have gotten slightly worse, but not as bad as they were before I was doing the heavy barbell work.
Yes, still on metformin at 5 months.
I’m sure this program works, but I suspect it’s not cheap. How many insurers would pay for it?
I think a simpler approach would be for physicians to buy loaner CGMs. Patients would pay only for sensors. If a patient had real-time feedback on the effect of various foods, even without 24/7 counseling, I think it would make a big difference.
Right away would be too soon. Most people are in shock when they get the Dx. But after a couple of weeks they should be ready for a CGM. They wouldn’t use it forever, just for a month or so to work out a good diet for themselves. Then perhaps for a few weeks later if they weren’t making progress.
Another approach would be “diabetes buddies,” assigning newbies to a patient who had had success. I suggested this to the local CDE, and he said, “I don’t have time to do that.” How much time would it take?
I think it’s sad that so many fitness people are using CGMs when the people who really need them can’t afford them.
I’ve becone a cynic. No wait! I’ve always been a cynic.
It’s a hell of a lot cheaper than having diabetes. Cost of administering the program is about 20-25% the cost of average medical cost for a patient with T2D.
Peter, I agree 100% that having high BG is more expensive in the long run than some treatment that would result in long-term remission. Sadly, insurance companies don’t agree. When people change insurance plans, the cost for the treatment that company A paid for may produce savings for company B. And insurance companies don’t care about your health. They just care about their bottom line.
Obviously, single payer would eliminate this problem, but with the current administration, we’re heading toward no payer.
I think Virta will be working to change this.