If you’re reading this, you probably know that I’m obsessed with longevity. But to really understand longevity, you must understand metabolic health, insulin resistance and, by extension, one of its end-results: type 2 diabetes (T2D). Though my medical practice does not focus on type 2 diabetes, I have taken care of several patients with T2D over the past few years. When I was in medical school I was taught many things about T2D, but one stands out most: T2D is incurable, I was told. Once you have it, you’ve always got it, and the best one can do is “manage” it as a chronic—but irreversible—condition.
But is this really true? Asked another way, is T2D reversible?
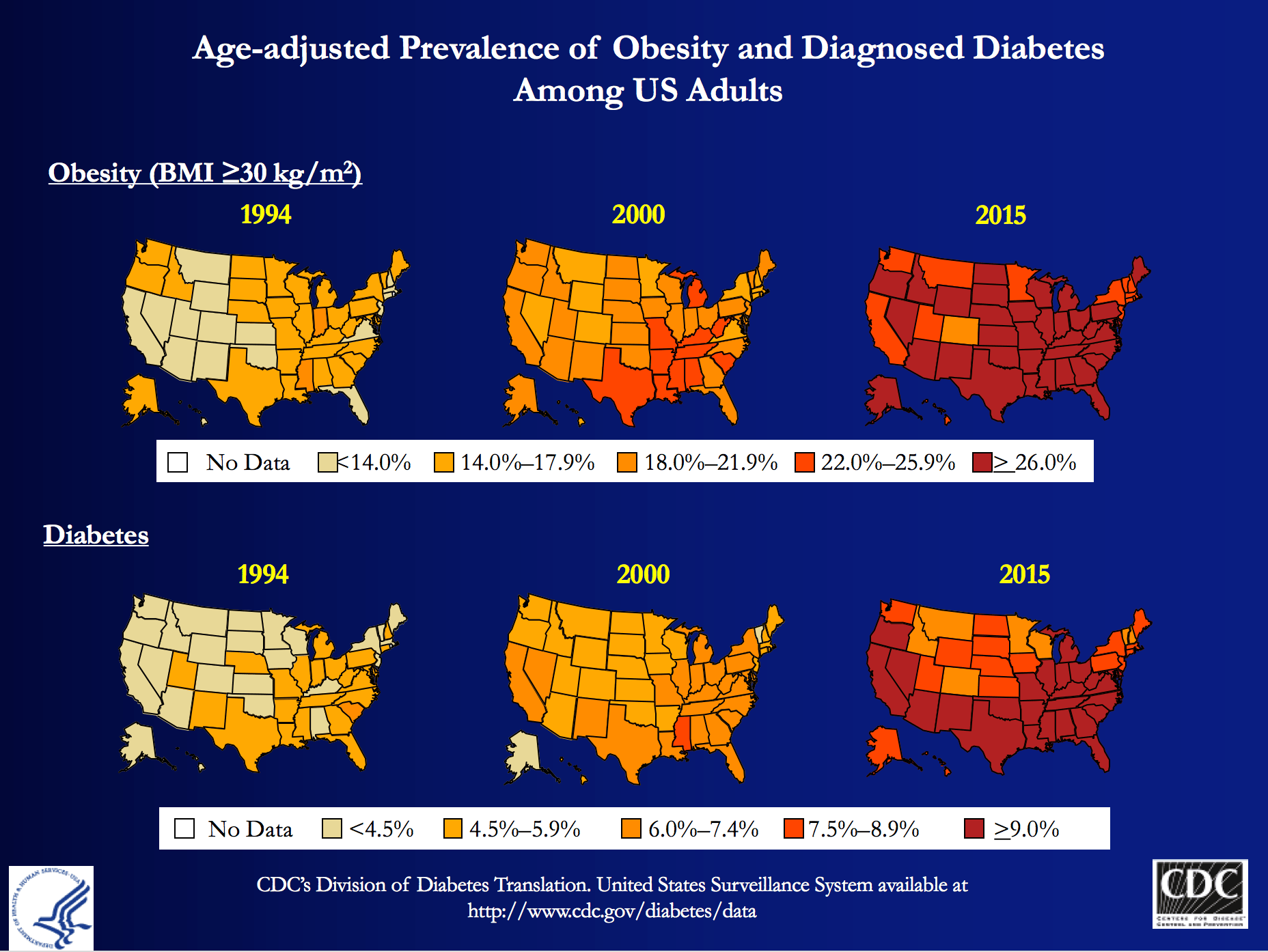
My obsession is partly due to my personal journey to better metabolic health, which I’ve documented elsewhere on this blog, and spoken about publicly. But those facts alone, don’t fully explain why I wanted to be involved with Virta Health (I’ll get to them shortly). T2D is a massive societal problem that has the potential to literally bankrupt countries: More than 29 million Americans have T2D and more than 80 million are pre-diabetic. And whether you view it through the lens of population health, or the lens of an individual patient, T2D is perhaps the biggest healthcare challenge of our generation.
At the population level, T2D costs Americans more than $300 billion per year: one of every three Medicare dollars is spent on T2D, and one of every six healthcare dollars is spent on T2D. At the individual level, patients and payers (employers and insurance companies) spend thousands of dollars (often more than $10,000) in annual expenses for medications and procedures with significant side effects, and much higher risk of developing cardiovascular disease, cancer, Alzheimer’s disease, blindness, amputation and kidney disease.
The traditional approach—which is clearly not working—is to “manage” this chronic condition with medications and the ever-ubiquitous “eat-less-avoid-fat-exercise-more” lifestyle interventions. At best, this approach only slows down the progression of the disease. Furthermore, many diabetes drugs have their own side-effects and diabetes management has a dismal diabetes reversal rate of about 1%. To date, the only clinically proven way to reverse T2D has been bariatric surgery, which is costly and not without risk. If one great thing has come from bariatric surgery, besides the obvious help to those have been successfully treated, it is that any physician or scientist paying attention to the results can’t help but notice that the reversal of T2D in these patients post-operatively seems uncoupled from their weight loss. In other words, adiposity, while correlated with T2D, is not likely the cause.
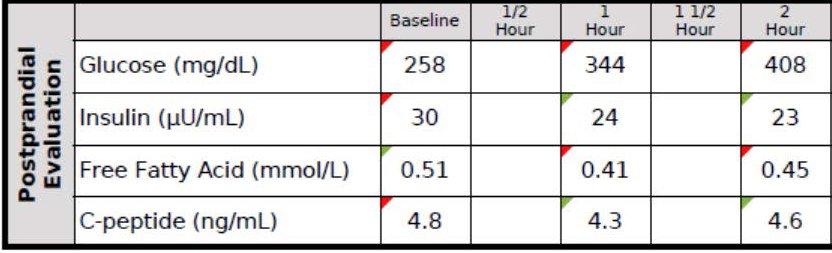
Every doctor has his (or her) “Patient 0”—the one who really got him (or her) thinking. I’d like to introduce you to mine, RB. When I met RB, he was a 37 year-old Mexican man with a family history of T2D who had a “high” glucose level on a screening blood test. His two-hour oral glucose tolerance test (OGTT) is below.
You don’t have to read these for a living to see this isn’t ideal. As you can see, his fasting glucose was 258 mg/dL and his fasting insulin, 30 uU/mL. When given 75 g of glucose, his glucose rose to 344 mg/dL at 60 minutes and 408 mg/dL at 120 minutes, all the while his insulin level fell from 30 to 24 to 23. These numbers alone confirm the diagnosis of T2D. But if we needed more evidence, his HbA1C was 9.7%, corresponding to an average blood glucose of 232 mg/dL (today the diagnosis of T2D is defined by HbA1C >= 6.5%, but I much prefer to use OGTT).
Ordinarily, for a patient with this degree of disease and beta-cell fatigue, I would have opted for at least two drugs, metformin (cheap) and a DPP4 inhibitor (not cheap) and most doctors would have gone straight to insulin, as well. However, due to the patient’s financial circumstances, we opted to only use metformin and dietary modification. The patient worked very long hours in construction and, frankly, was pretty much exercising all day, so there was no way adding more exercise to his day was going to work. If we were going to fix him, it had to be through nutrition. I spoke with one of my mentors, Dr. Naji Torbay, a remarkable endocrinologist who has the largest diabetes reversal program in Dubai and Lebanon, about this case. Even he thought it would be tough, but he’d reversed cases like this, so we gave it a shot.
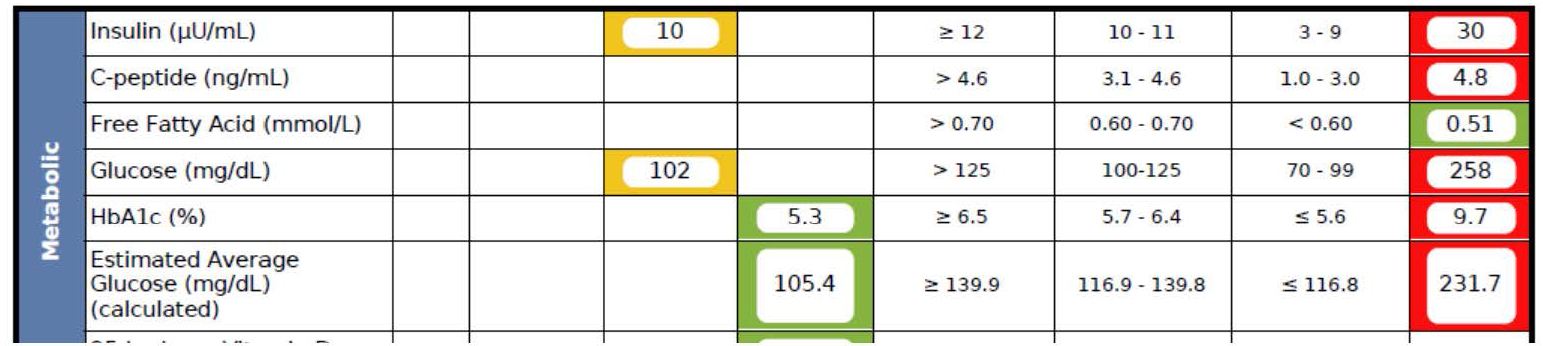
What happened over the next 5 months surprised me, as even I did not anticipate the alacrity of RB’s reversal. Below is a snap shot of RB’s labs from March 1, 2016 about 5 months after the OGTT, above. On the right side you can see the results from September 28, 2015, including the HbA1C of 9.7%, the fasting glucose of 258 mg/dL, and the fasting insulin of 30 uU/mL (HOMA-IR calculated at 19.1).
As you can see, the HbA1C fell to 5.3%—that’s even below the threshold of pre-diabetes—and the fasting glucose and insulin fell to 102 and 10, respectively (HOMA-IR calculated at 2.5).
RB doesn’t have diabetes any more. RB will avoid the amputations that destroyed the lives of his family. RB will not die prematurely from heart disease in his 50s. RB got a new lease on life.
If you think I’m telling you this story to impress you, you’re mistaken. Countless doctors (though not enough) know how to do what I did with RB—it’s actually simple biochemistry, and if a former surgeon like me can learn it, certainly anyone can, as long as one has the ability to frequently and safely manage medications and guide necessary behavior change. But sadly, most people like RB don’t have this option, and even if I and countless other doctors devoted the rest of our lives to helping everyone like RB out there, we could not put a dent in this problem, which is where Virta Health comes in.
Disclosure: I am an advisor to Virta Health and I have invested in the company, because I believe their approach is the best one to solve this problem—not the other way around.
Is it possible to deliver systematic diabetes reversal results (like the case above) safely, sustainably, and at scale among average diabetics?
Of course, even with the correct biochemical/nutritional approach, there are number of challenges to make T2D reversal possible at scale:
- Eliminating diabetes medications safely requires day-to-day (not monthly) careful adjustments by a physician. This is not how physicians work and would not be cost-efficient.
- Anything nutrition related requires a very high degree of individualization based on health status, lifestyle preferences and other life circumstances. For the 1% DIY’ers (who probably disproportionally read blogs like this one) any extreme approach can work, but at a population level, it won’t be enough.
- Both the patient and physician would need near real-time biomarker (e.g., CGM) data to adjust meds and the overall intervention. [By the way, I get asked all the time—mostly on Twitter—what CGM is…for those about to ask, here you go.]
- All behavior change and lifestyle interventions have failed at scale because only a small fraction of the population is able to DIY through complex decisions in today’s environment and life circumstances. This would require a near real time “personal coach” who can address any situation (e.g., family struggle, travel, new job, holidays).
It appears that we may be a step closer to somebody solving this challenge. Today, the first results of a T2D reversal clinical trial were published in the Journal of Medical Internet Research that show a promising new way to look at T2D: it is reversible in a large percentage of average patients, safely and sustainably. The trial was conducted by Virta Health, an online diabetes reversal clinic, which uses technology and artificial intelligence to solve the above mentioned care delivery challenges. The entire intervention is managed by physicians and the nutritional approach is based on highly individualized carbohydrate restriction and nutritional ketosis (which I’ve written about extensively in the past and throughout this blog).
The trial took place in Lafayette, IN, in partnership with Indiana University Health. A total of 262 women and men with T2D enrolled in the Virta Clinic. Average age was 54 (Stdev: 8); BMI 40.8 (Stdev: 8.9) and two-thirds of the patients were female. The trial will continue for at least two years, and data from the first 70 days were published today.
After just ten weeks:
- 56% of the diabetics enrolled achieved an HbA1C below the diabetic range (6.5%), while eliminating hypoglycemic medications
- Almost 90% of insulin users had it either completely eliminated (close to 40%) or reduced
- Mean body mass reduction was just over 7%, which is quite significant, but also shows that diabetes can be reversed before massive weight loss (i.e., it’s not the obesity that causes type 2 diabetes, which is consistent with the gastric bypass literature)
- Patient completion rate was >90%, which is remarkably high in an outpatient-based intervention.
- Reported feelings of hunger decreased from the pre-trial level (this seems to be a strong indication that will-power driven caloric restriction was not a factor in weight loss)
- Importantly, there were no serious adverse events, no incidence of symptomatic hypoglycemia, and no incidents of ketoacidosis.
The trial is ongoing with one-year data expected to be published shortly.
Yes, this is only one clinical trial and 70 days is not very long, but these data force us to consider that there is another way to look at T2D: it is not a chronic condition that gets progressively worse. With the combination of the right science and technology, it can be reversed at scale and among average diabetics. Clearly we need to look at the long-term success, and see many more patients succeed safely, but this is more promising than anything I have ever seen. I’ve seen some of the preliminary 1+ year analysis and the results look very impressive. I look forward to sharing them as they become publicly available.
If you are interested, you can learn more about Virta and their diabetes reversal science here. I’m excited to be a very small part of this organization and I look forward to the day when every patient with T2D at least has the chance to try an approach that can potentially reverse their condition.





Hi, Peter.
56% reversal vs the 1% typical? Those are impressive results!
Question: When someone under NK or VLCHF diet (T2-diabetic or otherwise) is about to do an OGTT only ONCE, would you typically recommend them to get out of ketosis 3 days earlier? Yes, this would avoid a “false pre-T2D” result as happened with your organ-donating friend. But doesn’t it also masks the “actual data”? The underlying questions seems to be: which results would lead to a more reliable interpretation, and whether results under NK could be correctly “translatable” to the not-under-NK ranges.
Occurred to ask me because you recommended to your friend to stop for 3 days to see the “normal” results, but RB did it under NK. What is the rationale of when to pick one or the other?
Tough question and in my limited experience depends on physical activity. For someone like RB (i.e., very active b/c of his job), they do fine on OGTT without carb re-feed. For those less active, typically 3 days of 100-150 g/day CHO is needed to avoid the artifact “physiological insulin resistance.”
Once you saw improved results in RB’s test results did you take him off of metformin? What’s your opinion on metformin as a prophylactic with regards to T2D and more broadly, life extension. Thank you.
Depends on patient. Sometimes quick taper off; sometimes on for life.
Hi Dr Attia,
As a shiny new physician and someone who comes from an athletic background myself, I think what you are talking about super exciting. I have one question about your proposed challenges though…why would patients following these rigorous lifestyle changes need CGM? I am assuming you are worried about hypo’s? is this a legitimate concern with lifestyle changes? also, dont we know from plenty of previous studies that tighter BG control leads to more adverse outcomes in diabetics? Great reading, and thanks!
Actually, in T2D patients not on insulin I don’t worry about hypo as much as using the CGM to teach the patient about the relationship of meal to BG.
I think the tighter BG control adverse outcomes have much more to do with concomitantly more aggressive medication use, not with the BG per se.
Well, Doc – you finally got on a topic I had to address. My n=1 experience tended to match your experience with RB almost point-by-point. I was in pretty serious financial straits, morbidly obese, Dx of T2DM ca.2005. Couldn’t afford the Dr.’s visits to pay for my glimperide Rx renewals, and started digging into lifestyle changes that might help. I was taking prerequisite courses for entry into nursing school, and my prof for A&P was lecturing on fatty acid metabolism. She started discussing the relationship between triglyceride storage in adipocytes and insulin, and I had my own little epiphany on the matter – namely, what if the T2DM and the obesity were being driven by the same metabolic defect? As often happens, life sidetracked my flash of insight, but about a year and a half later I revisited the idea long enough to get as far as a controlled short-term self experiment. I tried a cabohydrate-restricted diet for 24 hours, and when I pushed myself into temporary hypoglycemia at hour 18 via dietary intervention alone
I knew I was on to something. Fast forward to the present: completed the first round of nursing school with honors, HbA1c webt from 7.4 at initial Dx to a most recent one of 5.1, FBG typically in the mid-80’s to mid 90’s, weight loss of 125 lbs. and a lipid profile that even managed to surprise my PCP (HDL of 81, Triglycerides 85, LDL 95 & Total cholesterol of 190). In short – basically, I just saved my own life. So, yeah I’d say that management of T2DM is feasible, but reversal? Really, only time will tell.
Very cool, Dave.
This last comment, about using CGM to teach the patient surprised me. I went on keto in 2012 after starting to read your blog and also started reading some stuff and seeing video by Dr. Richard Bernstein. Buying a cheap meter and test strips at big box stores is so easy and inexpensive that I always advise people just to do that, so unless they are on lots of insulin and have to worry about hypos it seems that this would be far easier than a CGM.
I have considered starting a low-carb/keto support group locally though to be able to help people through the initial difficulties and to advise them to talk to a low-carb friendly physician if necessary.
The sad thing is that CGM’s are not typically covered for pre-diabetes when a
I am a Finnish MD and done for years among other things work with DM 2 patients. I have more than 2000 patients who are drug-free remission. It’s not a big deal, only what they need is bit right type info. I wrote a book how to do it and more people have access to the same situation only reading the book. I also have a Clinic in net and it is easy to operate through it. Inkinen is an engineer from Finland and “borrowed” the idea. I think this should be in the hands of professionals and not to give amateurs to spoil the thing.
Antti – I think there are an impressive collection of professionals (PhD’s, MD’s, Surgeons like you) involved in Virta Health. Why not join them instead of complaining they borrowed your idea and are not professionals. I don’t think you were the first to come up this idea.
Just curious… I’m I just a weird outlier or is it common to see fasting insulin INCREASE after being ulc for an extended period of time? My diet was tight. Ate this way for over 3 years. Lost well for over a year, maintained the second, weight slowly started creeping up 3rd year. Ingrated med Dr ran a bunch of labs and my fasting insulin was up to 16!!!! Tsh was at the top end of normal. I creased carbs *some* (60-80 range) and it is back down below 10. Problem is I felt better with it lower. This range is hard and everything has to be measured/weighed. And I’m grumpy hungry. So question… is the common and is there a way to get balance? Ulc is how I had planned to eat for the rest of my life.
Fasting insulin alone can be misleading. When extreme changes (like my patient here), it’s helpful, but no value in seeing change from 95 to 105–cortisol can easily do this. Reaven showed fasting insulin more closely correlated with steady-state plasma glucose (gold standard for IR) than HOMA-IR–implying fasting glucose actually *hurts* the calculation in non-diabetics.
Have you seen this from last spring? Doc L. directed me me to it. Will be interesting to see what else they might glean from working on proving it.
Medical Hypotheses 93 (2016) 87–92
Fructose surges damage hepatic adenosyl-monophosphate-dependent
kinase and lead to increased lipogenesis and hepatic insulin resistance
Alejandro Gugliucci
Peter,
Tracking BG 24×7 teaches one a hell of a lot about the effects various actions, foods, etc. on blood glucose. Not that I need to tell you. ?
The cost of the more sophisticated monitors make it prohibitive for most, though.
About a year ago I started wearing a CGM sensor from Freestyle, called the Libre. Lasts 2 weeks, costs less than $50 locally and can be read with a smartphone. Purely a monitoring device but perfect for 99% of use cases.
I’m not T1 or 2 but use it as a ‘fuel gauge’ for training and to check effects of various foods, supplements, etc. A great source of data! ?
The ADA has a new CEO. Meet the new CEO, same as the old CEO. The basic philosophy is go with whatever the USDA recommends.
One of two things are going on here. Either the ADA cannot admit that they have been giving horrible advise for decades, or they are just placating their Big Pharma donors (like the king of insulin – Eli Lilly), or their Big Packaged food donors, who make billions off of diabetes. It’s one or the other, or perhaps both.
Can I call the ADA a criminal organization?
Yes
I am a healthcare professional and work to help patients manage their diabetes. I have been following a ketogenic diet since locating your blog in October, with great success. While I am not currently encouraging my patients to follow a ketogenic diet, this is all very interesting to me, and I applaud the efforts toward researching this topic. I’m hopeful that one day this will be an ADA standard of practice for diabetes management.
One nagging questions comes to mind: are we truly observing ‘reversion’, or is this ‘remission’? I would be interested to see the effects of a high-CHO diet following this state of ‘remission’. Since restricting CHO intake is reducing pancreatic B-cell stress, when we reintroduce the stressor aren’t we back in the same boat? I have seen, first-hand, how diet/exercise/medication compliance results in a reduction of insulin/medication requirements (by de-stressing the pancreas and improving insulin sensitivity). Inasmuch, we never tell patients their diabetes is ‘gone’–even if they have a “normal” A1c/fasting BG, as there is still the baseline pancreatic insufficiency (in most cases) which usually resurfaces when challenged.
So, is DM2 ever ‘reversed’ or are we just removing the stressor and placing the patient in ‘remission’? Could this perhaps be based on the extent of their disease?
I would obviously love to hear that reversal is possible, I just am not making the connection…any insight/explanation would be helpful.
Dr. Attia,
Would you say ALT (SGPT) or AST (SGOT) are decent indicators of whether one has fatty liver? I was watching a Dr. Lustig video where he said ALT was a good indicator of fatty liver disease. If so, what numbers on those tests would be concerning to you? Thanks.
Yes, but not always. ALT/AST can be in the mid-20s with NAFLD present and can be in the 50’s or higher without. Like Rob (and we’ve discussed this at length), I believe “normal” LFTs are in the 20s or lower, despite the current reference ranges.
How do I get an appointment at Attia Medical?
Does anyone know?
?
https://www.dimensionsmagazine.com/news/art3.htm
Dr Naji Torbay, who treats people with weight problems at the American University Hospital, prescribes amphetamines as part of an overall diet plan but never for long periods.
Any thoughts?
Yes, but too nuanced for a comment.
So what’s the bottom line. Is ketogenic diet only option for people with diabetes and prediabetes? Is it good enough just to en whole foods or just lower carbs to some extenc bt not near ketosis threshold?
Hi Peter,
What was the Metformin dosage for RB?
1,000 BID.
Thank you for your work with Virta! My brother is T2D and I have pre-diabetes. We’re both using low carb to reduce and control this, although not successful yet in a reversal. Many of my close female relatives in their late 70s are developing MCI, dementia and a cluster of close relatives have died from pancreatic cancer. Would love to see work on Type 3 Diabetes and genetic links.
Another OBSERVATIONAL study came out today with news screaming scary headline “Is going gluten-free giving you diabetes? New study links diet with the disease.” Sigh. A whole 13% increase too. Meaningless.
“Gluten-free diets adopted by growing numbers of health-conscious consumers enhance the risk of developing Type 2 diabetes, scientists have warned.
A major study by Harvard University suggests that ingesting only small amounts of the protein, or avoiding it altogether, increases the danger of diabetes by as much as 13 per cent.
The findings are likely to horrify the rising number of people who are banishing gluten from their daily diet, encouraged by fashionable “clean eating” gurus such as Jasmine and Melissa Hemsley.”
“The study was observational, meaning participants reported their gluten consumption.”
https://www.telegraph.co.uk/science/2017/03/09/gluten-free-diet-boosts-diabetes-risk-major-study-suggests/
Hi Peter – I also enjoyed your podcast with Patrick O’Shaughnessy. Have you ever examined Type 1 Diabetes? Your comments on the podcast about examining gene markers and the impact on developing certain diseases intrigued me. The scientific community seems to be lacking in the area of diagnosing causes of Type 1 Diabetes. I am wondering if utilizing artificial intelligence and compute power (such as IBM’s Watson Health) has the potential for identifying the root cause of Type 1 Diabetes and could potentially lead to a cure. Any thoughts?
Thank you
FYI – I happen to be an ultra-runner (completing several 50 to 100 mile events) and there is an interesting trend in ultra-endurance events (which you are probably aware of) utilizing ketogenic diets to “force” the body into utilizing fat as a fuel source alternative to carbs.
T1D is a very different disease and I don’t have as much insight. See Jake Kushner at UT.
Dr. Bernstein Pioneered using a KD to manage his symptoms since the 1970’s. At 82, he likely the world,s oldest living T1 diabetic. His book “Diabetes Solution” goes into great detail on how to successfully treat T1D. He and many of his T1 patients keep their A1C in the 4’s. He also treats T2 diabetics. I am not diabetic, but have for many years been interested in the subject. I am still amazed how many of my friends and family, too who believe their doctors who tell them to shoot for a 7.0 A1C. I have given away many copies or Bernstein’s book over the years to T2 diabetics, and, not one has changed their behavior. It seems medication, eventually insulin, and a moderate carbohydrate diet with low fat, and low protein is fine with them. Dr. Bernstein was near death when he discovered a research paper where dogs with induced T1D were successfully treated with a strict fat and protein diet. At this time his wife a practicing doctor, managed to purchase a BGM only available at hospitals. Using the BGM DR. B determined that his blood sugar levels were wildly out of control. He eventually determined that his max amount of carbohydrate was about 22 grams per day. He went from death’s door to a full life using a KD and other practices along the way. It’s a truly inspirational story. Check out his website.
charles grashow March 10, 2017
https://www.dimensionsmagazine.com/news/art3.htm
Dr Naji Torbay, who treats people with weight problems at the American University Hospital, prescribes amphetamines as part of an overall diet plan but never for long periods.
Any thoughts?
Peter Attia March 10, 2017
Yes, but too nuanced for a comment.
Is that your way of avoiding the issue?
No, Charles, it’s my way of saying I don’t feel like writing another blog post right now. I hope that’s ok with you. If not, I’m happy to stay up all night tonight to work on it for you.
So snarky are we – yes – why not stay up all night? You might provide us with a valid reason why your mentor uses speed in his practice!
Would you all please be respectful, kind ( suprise!! he is a human being ), and appreciative toward this man: who has an all-in-constant-focus Career ; goes home to be the best Husband and Father he can be ; works out vigorously as an Athlete ; has the Needs we all have for rest, relaxation, fun, peace and solitude ; generously, has and is, in generousity, putting his knowledge, experience and critical thinking analysis of both aucourant information as well as replying to neophytes at their level out here ( no small feat ). Has it occured to you that he is possibly making the healthy, wise decision to pull back a bit ,for his own mental well being, from this time consuming project? Were he to stop entirely, yet leave the site up for our sakes, I would continue to feel only gratitude .
Kudos Dr. Peter Attia
My solution to Charles would have been to not post his second comment, but I Guess it just shows PA open to the discourse. I can respect a person or say they are great but it is not the same as endorsing everything they have ever done or said.