If you’re reading this, you probably know that I’m obsessed with longevity. But to really understand longevity, you must understand metabolic health, insulin resistance and, by extension, one of its end-results: type 2 diabetes (T2D). Though my medical practice does not focus on type 2 diabetes, I have taken care of several patients with T2D over the past few years. When I was in medical school I was taught many things about T2D, but one stands out most: T2D is incurable, I was told. Once you have it, you’ve always got it, and the best one can do is “manage” it as a chronic—but irreversible—condition.
But is this really true? Asked another way, is T2D reversible?
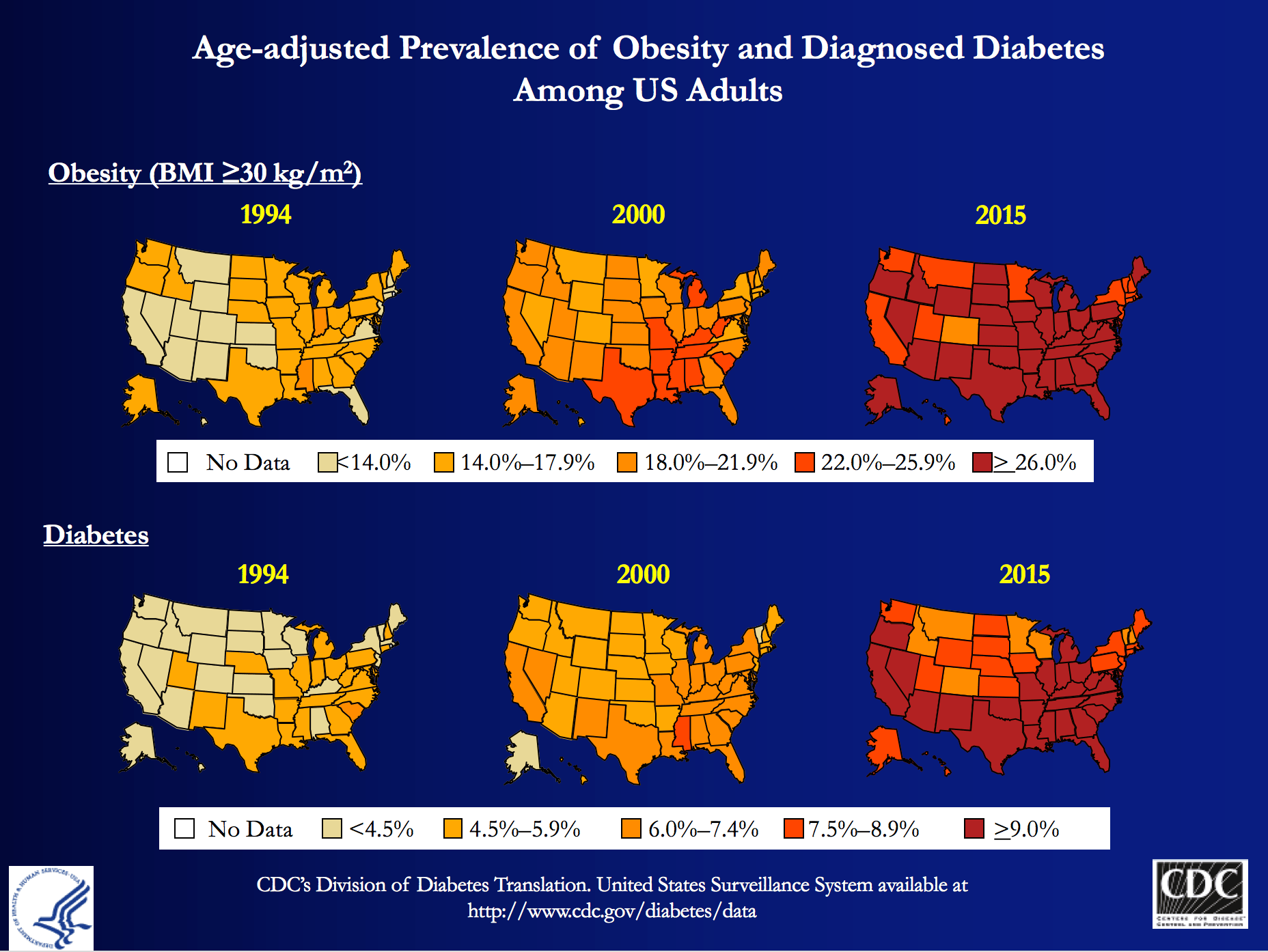
My obsession is partly due to my personal journey to better metabolic health, which I’ve documented elsewhere on this blog, and spoken about publicly. But those facts alone, don’t fully explain why I wanted to be involved with Virta Health (I’ll get to them shortly). T2D is a massive societal problem that has the potential to literally bankrupt countries: More than 29 million Americans have T2D and more than 80 million are pre-diabetic. And whether you view it through the lens of population health, or the lens of an individual patient, T2D is perhaps the biggest healthcare challenge of our generation.
At the population level, T2D costs Americans more than $300 billion per year: one of every three Medicare dollars is spent on T2D, and one of every six healthcare dollars is spent on T2D. At the individual level, patients and payers (employers and insurance companies) spend thousands of dollars (often more than $10,000) in annual expenses for medications and procedures with significant side effects, and much higher risk of developing cardiovascular disease, cancer, Alzheimer’s disease, blindness, amputation and kidney disease.
The traditional approach—which is clearly not working—is to “manage” this chronic condition with medications and the ever-ubiquitous “eat-less-avoid-fat-exercise-more” lifestyle interventions. At best, this approach only slows down the progression of the disease. Furthermore, many diabetes drugs have their own side-effects and diabetes management has a dismal diabetes reversal rate of about 1%. To date, the only clinically proven way to reverse T2D has been bariatric surgery, which is costly and not without risk. If one great thing has come from bariatric surgery, besides the obvious help to those have been successfully treated, it is that any physician or scientist paying attention to the results can’t help but notice that the reversal of T2D in these patients post-operatively seems uncoupled from their weight loss. In other words, adiposity, while correlated with T2D, is not likely the cause.
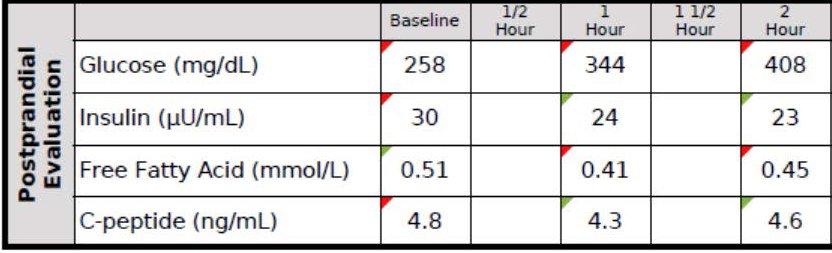
Every doctor has his (or her) “Patient 0”—the one who really got him (or her) thinking. I’d like to introduce you to mine, RB. When I met RB, he was a 37 year-old Mexican man with a family history of T2D who had a “high” glucose level on a screening blood test. His two-hour oral glucose tolerance test (OGTT) is below.
You don’t have to read these for a living to see this isn’t ideal. As you can see, his fasting glucose was 258 mg/dL and his fasting insulin, 30 uU/mL. When given 75 g of glucose, his glucose rose to 344 mg/dL at 60 minutes and 408 mg/dL at 120 minutes, all the while his insulin level fell from 30 to 24 to 23. These numbers alone confirm the diagnosis of T2D. But if we needed more evidence, his HbA1C was 9.7%, corresponding to an average blood glucose of 232 mg/dL (today the diagnosis of T2D is defined by HbA1C >= 6.5%, but I much prefer to use OGTT).
Ordinarily, for a patient with this degree of disease and beta-cell fatigue, I would have opted for at least two drugs, metformin (cheap) and a DPP4 inhibitor (not cheap) and most doctors would have gone straight to insulin, as well. However, due to the patient’s financial circumstances, we opted to only use metformin and dietary modification. The patient worked very long hours in construction and, frankly, was pretty much exercising all day, so there was no way adding more exercise to his day was going to work. If we were going to fix him, it had to be through nutrition. I spoke with one of my mentors, Dr. Naji Torbay, a remarkable endocrinologist who has the largest diabetes reversal program in Dubai and Lebanon, about this case. Even he thought it would be tough, but he’d reversed cases like this, so we gave it a shot.
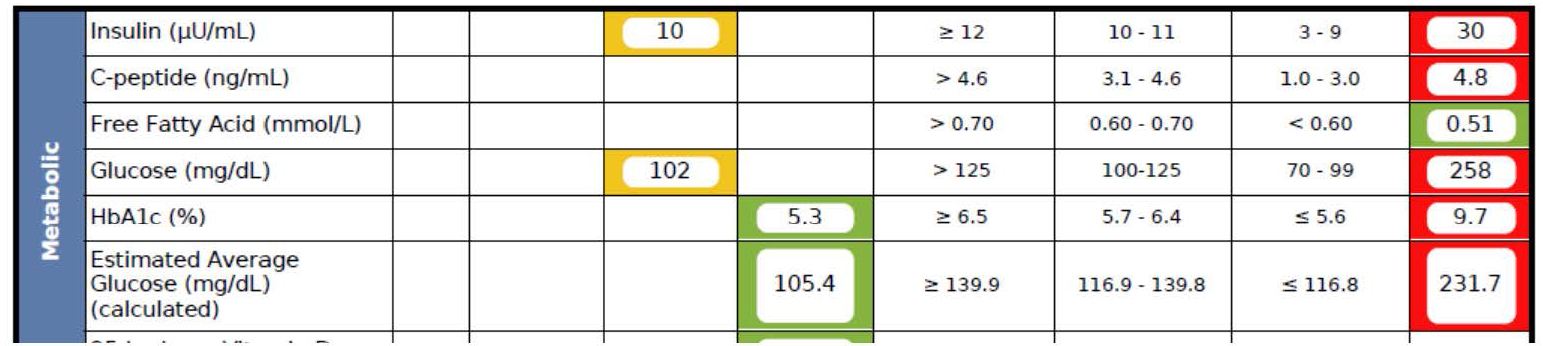
What happened over the next 5 months surprised me, as even I did not anticipate the alacrity of RB’s reversal. Below is a snap shot of RB’s labs from March 1, 2016 about 5 months after the OGTT, above. On the right side you can see the results from September 28, 2015, including the HbA1C of 9.7%, the fasting glucose of 258 mg/dL, and the fasting insulin of 30 uU/mL (HOMA-IR calculated at 19.1).
As you can see, the HbA1C fell to 5.3%—that’s even below the threshold of pre-diabetes—and the fasting glucose and insulin fell to 102 and 10, respectively (HOMA-IR calculated at 2.5).
RB doesn’t have diabetes any more. RB will avoid the amputations that destroyed the lives of his family. RB will not die prematurely from heart disease in his 50s. RB got a new lease on life.
If you think I’m telling you this story to impress you, you’re mistaken. Countless doctors (though not enough) know how to do what I did with RB—it’s actually simple biochemistry, and if a former surgeon like me can learn it, certainly anyone can, as long as one has the ability to frequently and safely manage medications and guide necessary behavior change. But sadly, most people like RB don’t have this option, and even if I and countless other doctors devoted the rest of our lives to helping everyone like RB out there, we could not put a dent in this problem, which is where Virta Health comes in.
Disclosure: I am an advisor to Virta Health and I have invested in the company, because I believe their approach is the best one to solve this problem—not the other way around.
Is it possible to deliver systematic diabetes reversal results (like the case above) safely, sustainably, and at scale among average diabetics?
Of course, even with the correct biochemical/nutritional approach, there are number of challenges to make T2D reversal possible at scale:
- Eliminating diabetes medications safely requires day-to-day (not monthly) careful adjustments by a physician. This is not how physicians work and would not be cost-efficient.
- Anything nutrition related requires a very high degree of individualization based on health status, lifestyle preferences and other life circumstances. For the 1% DIY’ers (who probably disproportionally read blogs like this one) any extreme approach can work, but at a population level, it won’t be enough.
- Both the patient and physician would need near real-time biomarker (e.g., CGM) data to adjust meds and the overall intervention. [By the way, I get asked all the time—mostly on Twitter—what CGM is…for those about to ask, here you go.]
- All behavior change and lifestyle interventions have failed at scale because only a small fraction of the population is able to DIY through complex decisions in today’s environment and life circumstances. This would require a near real time “personal coach” who can address any situation (e.g., family struggle, travel, new job, holidays).
It appears that we may be a step closer to somebody solving this challenge. Today, the first results of a T2D reversal clinical trial were published in the Journal of Medical Internet Research that show a promising new way to look at T2D: it is reversible in a large percentage of average patients, safely and sustainably. The trial was conducted by Virta Health, an online diabetes reversal clinic, which uses technology and artificial intelligence to solve the above mentioned care delivery challenges. The entire intervention is managed by physicians and the nutritional approach is based on highly individualized carbohydrate restriction and nutritional ketosis (which I’ve written about extensively in the past and throughout this blog).
The trial took place in Lafayette, IN, in partnership with Indiana University Health. A total of 262 women and men with T2D enrolled in the Virta Clinic. Average age was 54 (Stdev: 8); BMI 40.8 (Stdev: 8.9) and two-thirds of the patients were female. The trial will continue for at least two years, and data from the first 70 days were published today.
After just ten weeks:
- 56% of the diabetics enrolled achieved an HbA1C below the diabetic range (6.5%), while eliminating hypoglycemic medications
- Almost 90% of insulin users had it either completely eliminated (close to 40%) or reduced
- Mean body mass reduction was just over 7%, which is quite significant, but also shows that diabetes can be reversed before massive weight loss (i.e., it’s not the obesity that causes type 2 diabetes, which is consistent with the gastric bypass literature)
- Patient completion rate was >90%, which is remarkably high in an outpatient-based intervention.
- Reported feelings of hunger decreased from the pre-trial level (this seems to be a strong indication that will-power driven caloric restriction was not a factor in weight loss)
- Importantly, there were no serious adverse events, no incidence of symptomatic hypoglycemia, and no incidents of ketoacidosis.
The trial is ongoing with one-year data expected to be published shortly.
Yes, this is only one clinical trial and 70 days is not very long, but these data force us to consider that there is another way to look at T2D: it is not a chronic condition that gets progressively worse. With the combination of the right science and technology, it can be reversed at scale and among average diabetics. Clearly we need to look at the long-term success, and see many more patients succeed safely, but this is more promising than anything I have ever seen. I’ve seen some of the preliminary 1+ year analysis and the results look very impressive. I look forward to sharing them as they become publicly available.
If you are interested, you can learn more about Virta and their diabetes reversal science here. I’m excited to be a very small part of this organization and I look forward to the day when every patient with T2D at least has the chance to try an approach that can potentially reverse their condition.





Peter
Totally unrelated but are you available for a consult on a biotech company? If interest please email me. Many thanks and sorry to everyone for clogging this space.
Sorry, Van…my plate is really full.
Hello Dr. Attia,
I am very excited to follow Virta Health’s progress! I am wondering if you are aware of -and more significantly – are you able to speak about any pressure you and/or any colleagues may be feeling from “Big Pharma” in response to a very patient friendly – non- pharmaceutical based reversal of T2D?
Thanks and best of luck!
no worries. thanks very much for coming back. sorry to stuff the comments box. BTW really appreciate the stuff you put out there for people. wish you all the best, van
Hi Dr. Attia,
Any suggestions or can you refer me to articles/videos that you consider helpful in preventing Dawn Phenomenon?
Thank you!
Dean
No, but I wonder if it’s cortisol-mediated.
I don’t know what Cortisol-mediated means but I’m about to start researching it. Thank you!
Hi Peter,
I came across some analysis of studies that claimed/showed that LCHF diets raise blood glucose because insulin was not being excreted to reduce it. This seems to be a major arguing point for low fat and/or vegan proponents. Does *this sort* of high blood sugar (seemingly not an effect of insulin resistance) pose any health risks? Does avg. blood sugar become lower the longer you’re on a LCHF diet? Also, I can’t figure out why blood sugar would be so high on a ketogenic diet, when you’re eating low carb and lower protein.
I did several keyword searches on your site, but can’t find any place that you’ve addressed this. If you have, or know of a good video or article answering this question, please feel free to point me in that direction in lieu of writing an answer. Whether you can answer my question or not, thanks so much for posting your articles over the years! I came across you, your site, fasting, ketogenic and LCHF diets due to Tools of Titans (fyi) and couldn’t be more stoked!
With LCHF studies always check the following: what species? What is the actual dietary composition of the “LC” part?
Very interesting this article, you explained very well about it, I do not understand very well about it, but after my uncle died of diabetes I am interested in this subject, and your article came to calm very well.
Hello Dr., I watched several of your videos about dietary fat and ketosis, and I must thank you because this really changed my life. I lost from 110kg to 85kg, and being a science lover it was your videos that convinced me that low-carb is the way to go. My blood works are great, and I reference you whenever a discussion about this topic ensues.
Thank you from Portugal.
Hi Dr Attia, I’ve been doing keto for last 11 months ( properly testing glucose and ketones only the last 4 weeks . ) I see my morning glucose level is 5.6 , after I eat breakfast ( eggs , cheese , ) it’s 4.8 . I’m 44 years old and train weights 5 times a week , currently 5.11 and 84.8 kg at 9% bodyfat . I’ve lost 22 kg on this diet .
What’s your take on the Prof Longo’s latest publication in ‘Cell’? Its premise is so transformational, it’s being discussed by nutritional biologists, biogerontologists, and stem cell scientists.
The title is, “Fasting-Mimicking Diet Promotes Ngn3-Driven ?-Cell Regeneration to Reverse Diabetes.” In plain English, it means that a specific, temporary low-calorie diet activates pre-natal gene codes to grow beta or ?-cells.
I agree with you a slow low carb / ketogenic approach is an effective management protocol for T2DM having implemented this diet in multiple patients. HBA1C doesn’t lie either. I can tell imediately if the patient has been following the programme or not.
But this new paper indicates that T1DM can be reversed with consecutive implementation of the fasting mimicking diet for 3 months. This raises some interesting propositions. If we can stimulate Beta cell regeneration in the pancreas, what is the diet FMD doing to other organs? Is it all SIRT gene enabling? Is this RepleniSENS? and does it induce ApoptoSENS?
If you believe the paper, and follow with its premise, then do we need to implement this protocol in our overall geronprotection regime?
Hello Peter. As a PhD student of biology the JMIR Diabetes research you linked to above really pisses me off.
How can one claim to perform a medical dietary study where the important part of the methods is purely behavioral – “eats fats to satiety”. No statistical reports whatsoever on the actual composition of individual diets, hence chance of reproducibility. No negative controls (a baseline is not a control for an interventional study). One can publish in “JMIR” as one may as well simply publish on the blog, how am I supposed to evaluate this study anyway…? This is a blunt at-your-face demonstration of how financial interests may corrupt scientific ethics, wouldn’t you agree?
This is not meant to be the definitive statement on the topic. It’s called a pilot study.
Hi Dr. Attia. I’ve been in the anti-sugar camp for a while now, and I generally don’t worry about how much fat (both plant fat and animal fat) I consume. So, I’m curious to know what you think about Dr. Michael Greger’s (author of How Not to Die) position that insulin resistance is caused by a high-fat diet (which leads to increased fat levels in the blood, which in turn leads to increased fat levels inside muscle cells). https://nutritionfacts.org/video/what-causes-insulin-resistance/
This isn’t just academic curiosity. I’ve been prediabetic for a long time and I’m trying hard to avoid type 2 diabetes.
Thank you
There’s a difference between physiologic and pathologic insulin resistance (IR).
A high-fat diet–or fasting (i.e., a zero-fat diet)–can lead to IR in muscle, sparing more glucose for the brain in the short-term.
A high-fat diet–or fasting–can reduce IR, and a low-fat diet can increase IR, in the long-term.
IR locally can help partition more fuel globally.
IR can save life (starving, rapid blood loss), create life (pregnancy), and take life (T2DM and other chronic conditions). It can be both a normal physiological response and a pathological condition.
Peter thank you so much for sharing the wealth of knowledge from your personal journey and research.
Really a very rich and very good text
Anybody read Mark Hyman’s recent book “Eat Fat, Get Thin”? He mentions Dr. Attia on one page, concerning NUSI.
Any positive or negative opinions? It’s obviously written for the layman, like me.
Mark Hyman is a gifted communicator . He also oversees a marketing empire of information for patients . He advances many interesting ideas regarding nutrition , most of which are in the book “Eat Fat”. However, he also pushes ideas about vaccines and “complementary medicine ” that I just cannot agree with – see his website .
BTW, Mark did a web conference he called a “fat Summit ” that features an interview with Peter. In that , I think you can gain a sense of how Mark emphasizes marketing over knowledge. I have not listened to that piece in several months but my memory is that Marks questions to Peter just were not very well thought out.
I guess no one’s read Hyman’s latest book. While it’s heavily LC/HF,
his final stance is what he calls the ‘Pegan’ diet; the best of the Paleo + Vegan.
Surprisingly, he comes down hard on dairy, claiming that it contributes to obesity, diabetes, heart disease, dementia, and cancer.
He limits dairy to grass-fed butter, or ghee.
Sorry, Michael; I just read your reply. Thanks!
New study claims a 3 times higher risk of stroke from drinking one diet soda a day, but somehow no increased stroke risk at all from drinking a sugary soda a day. Also “prior studies have linked diet soda intake to stroke risk.”
https://www.sciencedaily.com/releases/2017/04/170420162254.htm
It’s a behavioral study (followed 4000 people for 10 years from the Framingham Heart Study’s Offspring and Third-Generation cohorts. Probably safe to disregard?
I wanted to add that I found some of the previous behavioral (not controlled) studies showing increased risk of stroke from drinking diet soda. They also found no increased risk from drinking sugary soda:
2015: 30% increase in CVD events including stroke and MI in those drinking 2+ diet sodas a day (study of 60,000 women): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4371001/
2012: 43% increase in stroke in those drinking diet soda daily. No increase in those drinking sugary soda. (study of 2564 adults in Northern Manhattan Study):
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3514985/
Is there a certain number of behavioral studies where one could say she needs to change her habits (if she were drinking a diet soda a day for example)?
Also, I heard you say once that you drink a diet soda every once in a while. How often?
Thanks.
Probably…who drinks diet soda?
People with diabetes, haha. I know I heard you say in a video you have one every once in a while, maybe it was just once a year, not sure. So you never drink them now?
Exactly… I still prob drink half a diet coke a month. Or not.
Hi Peter,
Per your recommendation, I painstakingly got my doctor to include some extra lab values during my annual physical. Unfortunately, he went so far as saying these lab values are unnecessary and that research scientists/doctors who hype up these values are engaging in what he called “mental masturbation”. lol
Anyhow, it turns out that my Lp(a) value is very high at 126. I’m only 32 but my dad had a severe stroke when he was relatively young (late 40s, early 50s). Should I be concerned at my age? It doesn’t look like there is anything I can do other than wait for the apo(a) antisense drug.
Also, I just want to say thanks for blogging about your self experimentation and being honest about their being no one-size-fits-all approach to diet and health. I really appreciate the nuance in your perspectives and it’s been interesting to see you change opinions over the years.
Also, my wife is a 3rd year med student at NYMC and we live in Stamford. If you are ever taking on new patients in the NYC/Westchester area, please let us know…
AJ, you should absolutely be seeing a lipidologist who understand why this should not be ignored.
Thanks Peter — do you have anyone you can recommend in Fairfield/Westchester County?
Check with Richard Bernstein.
Also, I read that niacin is sometimes used to lower Lp(a). Would it be a good idea to take niacin at my age?
It does, but it has not shown efficacy in reducing events.
Dr Attia, I couldn’t find a lipidologist with that name in the Northeast. I did find a doctor with that name who runs a diabetes practice in Mamaroneck, NY. I called his office and they said he only takes patients who have read his book and have diabetes.
Are you referring to a different Richard Bernstein? I don’t have diabetes but rather slightly elevated LDL and a very high Lp(a) value of 126 nmol/L.
Appreciate your help, Peter. Thanks.
I thought you were looking for a diabetologist. Look at NLA site for lipidologist.
Hi Peter,
Have you done any research on the effects of ketosis on circadian disruption and/ or do you know anyone who has? Shift workers are susceptible to T2D, cardiovascular disease, obesity and metabolic disease. I wonder if a ketogenic diet would be a good prevention to disease, but also, as new evidence is showing circadian disruption mutes gene recognition, would a ketogenic diet help boost energy by activating AMPK? Have you ever heard of Metformin used for shift workers? Can it be used for prevention and performance?
Thanks for your comments if you have time.
Neil
Hi, Peter! Quick question… is there a nutrition degree/ diploma/ certification program that you would readily recommend to Nutritional Therapists looking to further their knowledge? My own search has been frustrating as most programs I’ve come across are centered around textbooks citing studies that are decades old. Are there any cutting edge nutrition programs out there based on the latest science?
I don’t know… sorry.
Hi Peter.
First, thank you for sharing your knowledge and passion.
I have two questions about your IHMC lecture and your RQ during your metabolic chamber experience.
1. What would have been the likely your RQ graph during 3 hours bike ride instead of 45 minutes?
I observed that within 45 minutes your RQ fell from ca. 0.88 to ca. 0.83 meaning a fall from ca. 60% carbs energy to
ca. 45% energy from carbs.
2. Let’s assume that you eat ( within 5-10 min) a bar of milk chocolate on “empty liver”. 60g of refined carbs but still within liver glycogen capacity. And just after that you begin your bike ride with the load of 200 watts. What will be the likely RQ graph within 3 hours in that case? Refined carbs, although within glycogen liver capacity, will surely raise insulin and inhibit lipolysis immediately…
I’m trying to estimate and optimize my fat loss rate and amount of needed carbs, setting out boundary cases. I’m very well adapted for fat burning.
Once more thank you for all.
Dr. Attia, I apologize in advance for posting a comment so wildly off topic from this blog entry, but having just discovered your work I am desperate to connect and cannot find a more general mailbox or portal —
I am a lupus patient coming off of long-term steroid therapy after repeated flares and am dealing with many of the side effects you’d expect, in addition to still having to manage lupus and do what I can to keep it in remission. There is no sound medical guidance for how to manage nutrition for lupus patients, except for a proliferation of nonsense and snake oil related to “anti-inflammatory” diets, and I am advised by my team of medical professionals to avoid “extreme” elimination diets. Despite that advice, I believe it is because of my longtime avoidance of wheat and added sugars that I avoided diabetes and prediabetes during and after 5 years of high-dose prednisone. But I believe and hope I could do more via nutrition to manage my symptoms and perhaps reduce the load of multiple medications that I still must take.
So — do you have any experience with or advice related to autoimmune disorders in general, lupus in particular, or any referrals you could suggest in the Los Angeles area? Or could you just offer some reassurance that a keto diet is worth a try?
Dr. Terry Wahls has a protocol you might find helpful.
Hi Peter,
I am an oncologist in Bethesda and trained at the NCI and in practice with another NCI grad. We have been following your work and have been interested in nutrition and healh for some time. We are interested in your medical practice and in investigating what sort of patient sees you and if it makes sense for us to be your patients? Steve Rosenberg knows me and can vouch, I’d be a decent guy to work with!
Manish, I may have just responded to your friend over email on this.