A couple of weeks ago Tim Ferriss and I were having dinner and the topic of cancer came up. As some of you may know my background is in oncology, specifically in exploring immune-based therapies for cancer by exploiting the properties of regulator T-cells. But that was a long time ago. Like many of you, I expect, I’ve also been personally impacted by cancer having lost a friend to glioblastoma multiforme (GBM). I often describe GBM to people as one of the cancers that gives cancer a bad name. When I went to medical school I planned on becoming a pediatric oncologist, and though I ultimately chose to pursue surgical oncology, my interest in helping people with cancer never wavered.
Over dinner that night, Tim asked me if I could write – in about 1,000 words! – a post on cancer that would be interesting and digestible to a broad audience. “1,000 words?!,” I asked. “How about 30,000 words?,” I responded only half kidding. After explaining why I couldn’t possibly write such an abridged version, Tim talked me into it. And so, I plan to accept the challenge and hope to provide readers with such a post (it will be on Tim’s blog when I do so), hopefully in the next month or two.
For an introduction, however, I’d like take a step back and place this topic in a broader context. I don’t need to say much about cancer that you don’t already know. You probably know that about one in three Americans will develop cancer in their lifetime, and you probably know that about half of them will succumb to the disease. What you may not know, however, is that we have made virtually no progress in extending survival for patients with metastatic solid organ tumors since the “War on Cancer” was declared over 40 years ago. In other words, when a solid organ tumor (e.g., breast, colon, pancreatic) spreads to distant sites, the likelihood of surviving today is about what it was 40 years ago with rare exceptions. We may extend survival by a few months, but not long-term (i.e., overall) survival.
We screen better today for sure, but subtracting lead-time bias, it’s not clear this extends overall survival. We’ve had success in treating and even curing hematologic cancers (e.g., some forms of leukemia and lymphoma). Certainly testicular cancer patients (especially seminomatous) are better off today and those with GI stromal tumors (GIST), too. Surgical control of cancer is much better today and some local treatments (e.g., specific radiation), too. But for the most part, when a patient has metastatic cancer today, the likelihood of living 10 more years is virtually unchanged from 40 years ago.
About a year ago, I was asked to give a talk about metabolic disease to a group of physicians. But before I spoke, a very astute and soft-spoken oncologist, Dr. Gary Abrass, gave the following introduction as a way to frame the context of my talk. After all, I’m sure many in the audience were wondering what could a discussion of insulin resistance have to do with cancer. I have thought often of his words that night in the many months since he so eloquently and informally introduced me.
I asked Dr. Abrass if I could have a copy of his talk and share it with you, to which he kindly agreed. Below is, nearly verbatim, the talk he delivered that night. (Dr. Abrass did give me the liberty of tweaking the text a bit, for emphasis and clarity.)
How have we fared in the War on Cancer?
On December 23, 1971, President Nixon declared war on cancer by signing the National Cancer Act. I was going to title this, “40 years in 4 minutes,” but I think this will take me a bit longer. At the time I was a third year medical student. Two years before, Neil Armstrong had inflated our national pride by setting foot on the moon, and there seemed no scientific goal unachievable. Activist Mary Lasker published a full-page advertisement in The New York Times: “Mr. Nixon: You Can Cure Cancer.” And she went on to quote Dr. Sidney Farber, Past President of the American Cancer Society and whose name now sits atop the Harvard Cancer Center, “We are so close to a cure for cancer. We lack only the will and the kind of money and comprehensive planning that went into putting a man on the moon.” Since then, the federal government has spent well over $105 billion on the effort.
Forty years later, Dr. Farber’s prophecy remains unfulfilled. In 2012 cancer killed an estimated 577,190 people in the United States. The death rate, adjusted for the size and age of the population, has decreased by only 5 percent since 1950. And most of this decline is due to mammography screening in breast cancer and cessation of smoking, resulting in less lung cancer in men.
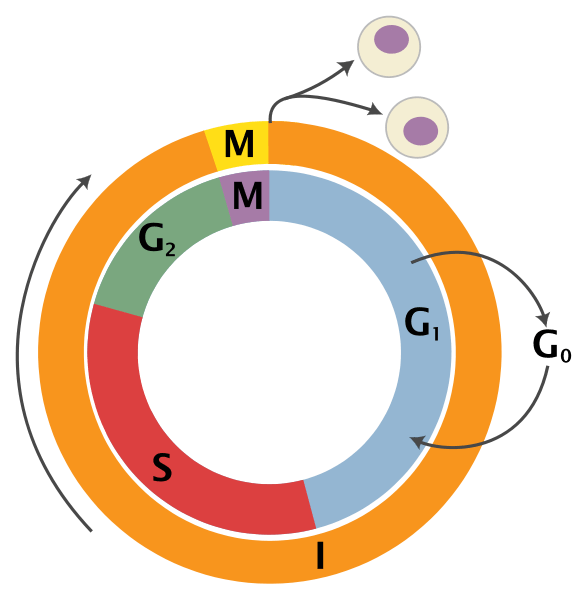
We have however developed a greater understanding of the biological and molecular basis of cancer. When I was a medical student, this graphic summarized what we knew about the growth cycle of the cancer cell.
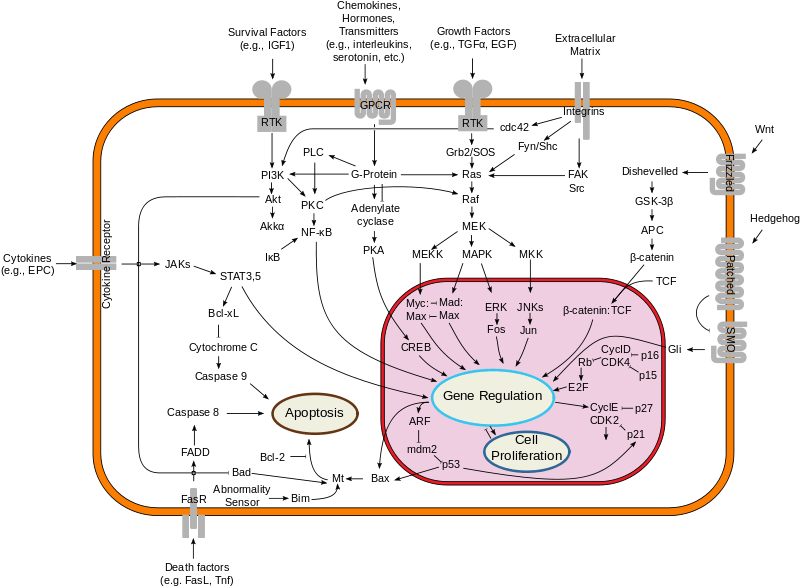
The next graphic demonstrates what we have learned, a truly overwhelming accomplishment, a dizzying array of interconnecting signaling “pathways,” and spawned a whole new field, “translational medicine.”
With the completion of the Human Genome Project, new sequencing technologies have also opened up the prospect of personal genome sequencing as an important diagnostic tool. A major step toward that goal was the completion of the sequencing of the full genome, first on James D. Watson, one of the co-discoverers of the structure of DNA. In fact, Steve Jobs had personal genome sequencing. The price is down to $1,000 and Mayo Clinic Proceedings recently had an article raising the concern of direct to consumer advertising for genomic sequencing. We are now able to sequence gene by gene, pathway by pathway, the genetic code of some cancers. New “smart” drugs have been developed that target various mutations in these pathways. And currently there are over 800 “targeted agents” in clinical development. These drugs have been described by some investigators as “The Holy Grail,” but the clinical results suggest more of a commemorative cup for a “Happy Meal.”
While there is nothing unique about this paper, it is a good example of a typical negative trial targeting the IGF-1 receptor with a monoclonal antibody. The lack of response does not make us question the role of the IGF pathway as a prime driver of malignancy, but rather demonstrates the ability of the cancer to resist therapy. It seems there is so much redundancy in the system that the cancer finds alternate pathways. The cancer cell continues to defend itself, to bob-and-weave like the arcade game “Whack-a-Mole.”
So the investigators combined the IGF-1 monoclonal antibody with various other therapies: standard platinum based chemotherapy regimens, the “small molecule” tyrosine kinase inhibitor gefitinib (Iressa) targeting another common pathway (EGFR), and also the mTOR inhibitor temsirolimus (Torisel) which targets the IGF-1 pathway a bit further along. In any case, the point is, it still didn’t work. But why?
Investigators have mapped the genome of a typical lung cancer patient and found over 50,000 mutations. That’s a lot of targets! Granted they are not all ‘driver’ mutations, some are ‘passenger’ mutations. The patient whose genome was mapped was a 51-year-old man who’d reported smoking 25 cigarettes a day for 15 years. At 50,000 mutations, it works out to one mutation for every 2.7 cigarettes.
Last year the New England Journal of Medicine published a study by Gerlinger and colleagues. These investigators looked at intra-tumor heterogeneity. They performed a molecular dissection. They found diversity within the tumor itself. Each cancer is not cancer but, indeed, it is CANCERS. In other words “all cancers are rare cancers.” Let me repeat this point. Each tumor is a collection of heterogeneous – not homogenous – mutated cells. This article has engendered some discussion and some controversy. Many say that the results of the study bring the idea of personalized medicine to a halt, or at least dramatically slow it down. Are there exceptions? Yes, but they are rare. One example of an exception to this revelation is chronic myelogenous leukemia (CML), a cancer with a known single driver mutation.
In September 2011, biologist Dr. Alasdair MacKenzie of the University of Aberdeen, speaking at the British Science Festival in Bradford, explained that researchers trying to fully understand how our DNA causes disease might not be looking in all the right parts of the genome. The past decade of genetic studies has revealed that our 3.2-billion-long-DNA-letter code is more complex than anyone could have thought. More than 98% of the human genome does not encode protein sequences. It’s been referred to as “Junk DNA” and thought not to have a function, but maybe more correctly is that we do not know the function. He refers to this as the “dark matter” of the genome. And it’s thought that some of these “alternate pathways”, in which our resourceful cancer cell seeks refuge, may reside here. If this was not complicated enough, the new field of Epigenetics has grown exponentially resulting in a widening of the battlefield.
These are factors that can affect the expression of genes without causing mutations, turning switches on and off. In terms of cancer, much of this research has concentrated on what are called “Nononcogenic stress targets.” We can stress an organism in many ways: heat, poison, starvation, suffocation or more scientifically thermal, chemical, metabolic and oxidative stress. Organisms have an ingenious way of responding to such stress. In the 1960s an assistant in FM Ritossa’s lab accidentally boosted the incubation temperature of Drosophila (fruit flies), and when later examining the chromosomes, Ritossa found a “puffing pattern” that indicated the elevated gene transcription of an unknown protein.
This was later described as the “Heat Shock Response” and the proteins were termed the “Heat Shock Proteins.” This same HSP increases survival under a great many pathophysiological conditions. The HSP70s are an important part of the cell’s machinery for protein folding and help to protect cells from stress. While it enhances the organism’s survival and longevity under most circumstances, HSF1 has the opposite effect in supporting the lethal phenomenon of cancer. These proteins enhance the growth of cancer cells and protect tumors from treatments. This remarkable protein affords a protective response to other proteins in the cell, acting as a “chaperone” preventing them from mis-folding or “denaturing,” like when a boiled egg white turns opaque. These heat shock proteins are expressed at high levels in many tumor types: breast, endometrial, lung, prostate, even brain tumors. HSP overexpression signals a poor prognosis in terms of survival and response to therapy. HSP’s are now on the radar as a key target in the ongoing battle. This protein folding stress response is a hot topic in current cancer research. I have been communicating with Dr. Debu Tripathy who is currently studying epigenetic changes and protein folding stress responses associated with obesity. This protein folding stress response affords the cancer cell a survival advantage, and we share this protective mechanism with a fly, such a distant relative in our family tree, that one can only conclude that the cancer cell has hijacked this maneuver, this protective drive for immortality from the legacy of 100’s of millions of years of evolution…such a resourceful and formidable opponent.
In any case, when the Human Genome Project was near completion, President Clinton hosted a White House ceremony and announced that, “it will revolutionize the diagnosis, prevention and treatment of most, if not all, human diseases, and that humankind is on the verge of gaining immense new power to heal.”
The hubris of it all. It’s reminiscent of the quote of Sidney Farber. Hopefully this is not tempting fate. Theologians tell us the only unforgivable sin is pride. The increasing complexity of the science is affording us quite a dose of humility. British Physicist Brian Cox said that “being at the junction of the known and the unknown is a beautiful place to be for a scientist,” but it seems the more we know, the more we don’t know. Not unlike Winston Churchill’s characterization of Russia as “a riddle wrapped in a mystery inside an enigma.” Not unlike modern theoretical physics, one questions whether we are capable of understanding the complexity of the science. Hopefully it’s not like trying to teach my dog quantum theory. We are so smart, but it seems that the cancer cell is smarter. It bobs and weaves, slips our punches, and when we back it into a corner, it defends itself in remarkable ways borne of millions of years of evolutionary acumen much of it hidden in the dark matter of our genome.
Maybe we should call a truce in the War on Cancer and concentrate on prevention. Besides smoking, the most preventable cause of cancer seems to be obesity. It is generally thought that obesity may account for about a third of many cancer types, particularly breast, colon, uterus, kidney and esophagus. Obesity is a risk factor for type II diabetes and these patients are not only more likely to get cancer, but to have poor outcomes. Other speakers will explore the relationship of obesity and cancer, the epidemiology and the science, and see if this lends support to any practical prevention measures.
Gary Abrass, M.D.
April 19, 2012
Afterword
Just as the best way to get in shape is not to ever get out of shape, the best treatment for cancer is almost assuredly not to get cancer. And that’s clearly the theme of the introduction Dr. Abrass gave me. But I’m sure many of you are asking a more important question — what happens if I or someone I care about has cancer? If you can be patient with me, I do plan to address this, to the best of my understanding, in the coming months.


Have you come across this before?
Cancer-specific Cytotoxicity of Cannabinoids
By Dennis Hill
First let’s look at what keeps cancer cells alive, then we will come back and examine how the cannabinoids CBD (cannabidiol) and THC (tetrahydrocannabinol) unravels cancer’s aliveness.
In every cell there is a family of interconvertible sphingolipids that specifically manage the life and death of that cell. This profile of factors is called the “Sphingolipid Rheostat.” If ceramide (a signaling metabolite of sphingosine-1-phosphate) is high, then cell death (apoptosis) is imminent. If ceramide is low, the cell will be strong in its vitality.
Very simply, when THC connects to the CB1 or CB2 cannabinoid receptor site on the cancer cell, it causes an increase in ceramide synthesis which drives cell death. A normal healthy cell does not produce ceramide in the presence of THC, thus is not affected by the cannabinoid.
The cancer cell dies, not because of cytotoxic chemicals, but because of a tiny little shift in the mitochondria. Within most cells there is a cell nucleus, numerous mitochondria (hundreds to thousands), and various other organelles in the cytoplasm. The purpose of the mitochondria is to produce energy (ATP) for cell use. As ceramide starts to accumulate, turning up the Sphingolipid Rheostat, it increases the mitochondrial membrane pore permeability to cytochrome c, a critical protein in energy synthesis. Cytochrome c is pushed out of the mitochondria, killing the source of energy for the cell.
Ceramide also causes genotoxic stress in the cancer cell nucleus generating a protein called p53, whose job it is to disrupt calcium metabolism in the mitochondria. If this weren’t enough, ceramide disrupts the cellular lysosome, the cell’s digestive system that provides nutrients for all cell functions. Ceramide, and other sphingolipids, actively inhibit pro-survival pathways in the cell leaving no possibility at all of cancer cell survival.
The key to this process is the accumulation of ceramide in the system. This means taking therapeutic amounts of cannabinoid extract, steadily, over a period of time, keeping metabolic pressure on this cancer cell death pathway.
How did this pathway come to be? Why is it that the body can take a simple plant enzyme and use it for healing in many different physiological systems? This endocannabinoid system exists in all animal life, just waiting for it’s matched exocannabinoid activator.
This is interesting. Our own endocannabinoid system covers all cells and nerves; it is the messenger of information flowing between our immune system and the central nervous system (CNS). It is responsible for neuroprotection, and micro-manages the immune system. This is the primary control system that maintains homeostasis; our well being.
Just out of curiosity, how does the work get done at the cellular level, and where does the body make the endocannabinoids? Here we see that endocannabinoids have their origin in nerve cells right at the synapse. When the body is compromised through illness or injury it calls insistently to the endocannabinoid system and directs the immune system to bring healing. If these homeostatic systems are weakened, it should be no surprise that exocannabinoids perform the same function. It helps the body in the most natural way possible.
To see how this works we visualize the cannabinoid as a three dimensional molecule, where one part of the molecule is configured to fit the nerve or immune cell receptor site just like a key in a lock. There are at least two types of cannabinoid receptor sites, CB1 (CNS) and CB2 (immune). In general CB1 activates the CNS messaging system, and CB2 activates the immune system, but it’s much more complex than this. Both THC and anandamide activate both receptor sites. Other cannabinoids activate one or the other receptor sites.Among the strains of Cannabis, C. sativa tends toward the CB1 receptor, and C. indica tends toward CB2. So sativa is more neuroactive, and indica is more immunoactive. Another factor here is that sativa is dominated by THC cannabinoids, and indica is predominately CBD (cannabidiol).
It is known that THC and CBD are biomimetic to anandamide, that is, the body can use both interchangeably. Thus, when stress, injury, or illness demand more from endogenous anandamide than can be produced by the body, its mimetic exocannabinoids are activated. If the stress is transitory, then the treatment can be transitory. If the demand is sustained, such as in cancer, then treatment needs to provide sustained pressure of the modulating agent on the homeostatic systems.
Typically CBD gravitates to the densely packed CB2 receptors in the spleen, home to the body’s immune system. From there, immune cells seek out and destroy cancer cells. Interestingly, it has been shown that THC and CBD cannabinoids have the ability to kill cancer cells directly without going through immune intermediaries. THC and CBD hijack the lipoxygenase pathway to directly inhibit tumor growth. As a side note, it has been discovered that CBD inhibits anandamide reuptake. Here we see that cannabidiol helps the body preserve its own natural endocannabinoid by inhibiting the enzyme that breaks down anandamide.
In 2006, researchers in Italy showed the specifics of how Cannabidiol (CBD) kills cancer. When CBD pairs with the cancer cell receptor CB-2 it stimulates what is known as the Caspase Cascade, that kills the cancer cell. First, let’s look at the nomenclature, then to how Caspase kills cancer. Caspase in an aggregate term for all cysteine-aspartic proteases. The protease part of this term comes from prote (from protein) and -ase (destroyer). Thus the caspases break down proteins and peptides in the moribund cell. This becomes obvious when we see caspase-3 referred to as the executioner. In the pathway of apoptosis, other caspases are brought in to complete the cascade.9
Even when the cascade is done and all the cancer is gone, CBD is still at work healing the body. Its pairing at CB-2 also shuts down the Id-1 gene; a gene that allows metastatic lesions to form. Fundamentally this means that treatment with cannabinoids not only kills cancer through numerous simultaneous pathways, but prevents metastasis. What’s not to like. One researcher says this: CBD represents the first nontoxic exogenous agent that can significantly decrease Id-1 expression in metastatic carcinoma leading to the down-regulation of tumor aggressiveness.10
This brief survey touches lightly on a few essential concepts. Mostly I would like to leave you with an appreciation that nature has designed the perfect medicine that fits exactly with our own immune system of receptors and signaling metabolites to provide rapid and complete immune response for systemic integrity and metabolic homeostasis.
Excellent article, that was over my head at times; helpful references; and interesting comments above. If I had been diagnosed with cancer, I’m sure I’d give low carb a try in case it helped the chemo. Yours and other discussions on the topic seem to be in that direction.
But what about every one of us that have pre-cancerous cells in our body and care mostly about prevention? There must be a comprehensive recommendation that is more specific than exercise and don’t be overweight!
Maybe this sounds insensitive, but aren’t high cancer rates an extremely GOOD thing? Cancer is what people die from when they haven’t already died from childbirth, cholera, bubonic plague, shipwrecks, mineshaft collapses, etc.
The fact that a high portion of the population dies from cancer shows how unbelievably successful we’ve been at solving the problems that traditionally plagued mankind.
Don’t take this the wrong way- obviously I’d do anything to help a family member with cancer survive. But I do think it’s worth pointing out the historical significance of higher cancer rates. I suspect people in the past would gladly trade life expectancies with us….
I think understand what you’re trying to get at, but I’m not sure I agree. I can think of a dozen ways I’d rather see a loved one die than succumb to malignancy.
I came across something very promising as a cancer treatment that has actually been proven to work on skin cancer. It is a totally different approach that has been overlooked, probably because it is based on an old folk remedy and the researcher is outside the conventional medical establishment. Such claims are usually dismissed as “quackery”, but this doctor actually spent over 25 years and millions of dollars in order to validate his treatment with studies conducted by reputable institutions. He can legally call it a “cure” because he has the proof to back it up. I posted about it here: https://carbwars.blogspot.com/2013/09/is-there-already-cure-for-cancer.html.
I have no vested interest in promoting this treatment; I discovered it while searching for a way to help a family member, but I have tested it myself and I feel that it deserves consideration.
Why not starve the cancer by removing glucose? Most cancer cells need glucose for energy. What about the brain you might rightfully ask? Enter ketosis, then the brain will do fine on beta-hydroxybutyrate.
But the body will keep a constant blood glucose level even in ketosis you might argue? True, but any MD can give you several ways to lower blood glucose level close to zero with medication (Jeff Volek did inject insulin in ketogen adapted athletes and they did just fine on ketones despite a dramatic drop in blood glucose).
Has anyone tried this? I’ve written to several Journals about this idea and they all responds it is a total new and interesting way of addressing the cancer issue but non of them feels it is the right stuff for their audience. Please Peter, do something?
Best regards
Patrik
(former R&D Chemist in big Pharma)
https://www.facebook.com/#!/NewIdeaToCureCancer
Pleas “like” to spread the word
Yes, It’s called a Ketogenic diet. Originally formulated to reduce seizures in epileptics. It has been shown to starve Cancers by denying them access to glucose.
Great post even though I didn’t get all of it since it was a bit technical and english isn’t my first language.
Both my parents died in cancer way too early (mom 54, dad 68). Since dad passed last year I started reading about cancer and I soon realised that a ketogenic, low-carb-high-fat diet probably is a good way of preventing cancer. LCHF as this diet is called here in Sweden is really becoming popular and Dietdoctor.com is one of the largest blogs in the country (I know you’ve met Andreas). One of the best books I’ve read on the subject is “Ett sötare blod” (“A sweeter blood – The health effects of a century with sugar “) by the science journalist Ann Fernholm. https://www.bokus.com/bok/9789127133730/ett-sotare-blod-om-halsoeffekterna-av-ett-sekel-med-socker/
She explains how insulin effects high levels of igf-1 and that igfbp-1 plays an imortant roll which in turn stimulates tumour growth. She ends the chapter about cancer like this (translated from swedish): “With all the knowledge available about how sugar and high blood sugar can drive cancer, this chapter should have been concluded with the effect a blood sugar lowering low-carb diet can have on the development of cancer.
But when I look in the scientific literature, I start to wonder if I’m crazy or at least if I have misunderstood something . Part of me still wants to live in the belief that the scientific community is driven by some kind of logic. Once it has identified a problem – it looks for the solution to that problem. If high blood sugar drives cancer, a blood sugar-lowering diet could probably help chemotherapy to get the upper hand in treatment. It could tip the scale in the right direction. However, I cannot find any good studies examining this.”
You would like Ann. She, like yourself, is very credible as a science researcher and is very technical about it but is good at explaining stuff for average Joe’s lke myself as well. She also performs experiments on herself which I know you do too.
None of my parents were obese. On the contrary, they were both lean and quite athletic (both swimmers in their youth) and they didn’t smoke. They lived healthy lifestyles and were very “outdoorsy”. Mom died in acute myelogenous leukemia which was an effect of the aggressive treatment for her breast cancer one year earlier. Dad died of esophageal cancer. You talk about reducing obesity in order to reduce cancer. Do you believe a ketogenic diet is as effective for the lean person or do you think cancer strikes for other reasons when it comes to lean people? I mean, I’m lean but I eat a ketogenic diet and work out a lot beacause I don’t want to end my life as they did. It’s just not worthy. Do you belive I am improving my odds or am I kidding myself?
The major deviation from evolutionary dietary norms for our species which has occurred in the past 100 years has coincided very neatly with the exponential rise in rates of both heart disease and cancer. It would seem to be the most obvious place to look if one applies the principle of Occam’s Razor to the question of “what’s gone wrong.” Add in endocrine disruptors and the altered lipid profile of factory-farmed meat, plus what we’re now finding out about the new GMO wheat, and the answer would seem to be self-evident . . . but the message is being actively suppressed by those with SO MUCH TO GAIN from the current paradigm. As ever, “Cui Bono?”
The politically-correct but dead WRONG dietary disinformation still parroted by National Public Radio has resulted in my now refusing to fund them with my membership–they will not acknowledge alternative hypotheses.
You are doing vital work here–my thanks!
I still support NPR, but you’re right: some stories make me want to throw the radio out the window, like the one where doctors were taking cooking lessons at a culinary institute (so they could better tell their patients about “healthy” eating). First up on the menu? “Recovery” bars containing marshmallows…
“We’re going to try to take advantage of what’s called an anabolic window, a specific period of time after the workout where we can give them the best gains,” he says.
The first course will be a “recovery” bar with whole grains, spices and marshmallows to deliver some quick sugars. Then there’s the frittata that Solanki is laboring away at, stuffed with baby zucchini, red bliss potatoes, red bell peppers, parmesan and feta cheese and spinach. It’s a feast, says culinary student Briana Colacone, designed to refuel with lean protein and carbs. “It’s going to be really good,” she says.”
*sigh*
Yes, this is frustrating. Imagine how confusing this is for the public?
Dear Peter,
I almost jumped out of my chair at work when I saw this post come through my email. I knew you would start covering cancer eventually and was trying to be patient, so I just want to say I’m really happy to see the beginning post. I’m also in the Seyfried camp and have followed metabolic cancer research for awhile now. I lost my mom to GBM three years ago so I follow the research on brain cancer in particular. My mom was a nurse practitioner in vascular radiology at Duke and meticulously followed a “heart healthy” low fat diet. I recently came across a cardiologist who is in remission from GBM (3 years) and had also done a lot of research on his diagnosis. He found an intriguing study by a Johns Hopkins-trained cardiologist who now practices in Israel. This doctor had collected data on 23 invasive radiologists and cardiologists who had developed tumors, of which 17 were GBMs on the left side of the brain (my mom’s was also on the left side of her brain as was the cardiologist’s who was not included in the data). Perhaps I am using facts to suit theories instead of theories to suit facts, but even if this study doesn’t demonstrate anything conclusively I think it is a very alarming cause for pause. The current literature on this topic seems to blame the cardiologists’ exposure to radiation, but I thought immediately about the low fat diet cardiologists typically endorse (and live by).
I asked the cardiologist if he had tried the ketogenic diet and he said he had. He also said that the “keto breath” side effect was particularly potent in his case (to the point where people around him noticed his odor) and he recognized the smell from treating diabetic patients with ketoacidocis. I don’t know why this seems significant to me, but I had only a mild and fleeting experience with this side effect while adapting to nutritional ketosis. I wonder if there is some kind of link here to people who adopt ketosis in an earlier/healthier phase of life? It also could just be a random side effect that varies by person but I thought it might add some anecdotal food for thought to your research.
Anyway, I also just wanted to say that I’m appreciative of your work and look forward to learning more about your thoughts and research in the next post.
Caitlin
Caitlin, I’m very sorry to hear about your mother. I can understand how this would generate so much interest for you. Hopefully I can point you in some interesting directions over the next few months.
Caitlin,
The loss of your mother is even more devastating considering she worked at Duke, which is where Dr. Eric Westman’s clinic is. (If you’re not familiar with him, he’s one of the top proponents/pioneers of low-carb/ketogenic diets. His focus is weight loss and metabolic syndrome, but I’d be surprised if he wasn’t quite familiar with Seyfried’s work and the implications of ketosis for cancer.) He and the cardiologists are probably only a few hundred feet away from each other physically, but galaxies apart in approach to medical practice.
Thanks Peter, I look forward to it.
Amy, yes Duke is on the cutting edge in brain cancer research. I’m not familiar with Dr. Westman, but my mom was treated by Dr. Henry Friedman at the Brain Tumor Center and Dr. Allan Friedman was her surgeon. I do agree that it’s unfortunate that these links were not well understood enough for the two departments to collaborate. My mom worked at Duke for 20+ years and had surgery the same day as Ted Kennedy. She had worked as an OR nurse earlier in her career for the surgeon and everyone kept telling her she was Duke’s real VIP. Her colleagues from all over the hospital went above and beyond for her and for our family. If they had thought about the metabolic links they definitely would have discussed it with her.
Most of all, my mom thought she WAS following a cancer prevention diet, so she never thought to try and change it once she was diagnosed. My brother and I joked that she was a rabbit because she ate so many colorful vegetables. She loved preventative medicine and read all kinds of books about it. To her credit, she did not have as much difficulty (not saying it was easy, just in a relative sense) with surgery recovery and enduring a lot of the chemo/radio treatments because of her otherwise good health (non-smoker, no diabetes, no high blood pressure, etc.). Unfortunately, I’m finding out a lot of her diet information was wrong, or at least it was missing a very significant component (FAT). But I try not to get too bogged down in the what ifs (would lose it if I did). Dr. Seyfried’s book came out in June 2012 and my mom was diagnosed in May 2008. She lived for exactly two years, which was pretty much the max as I understand it (99% of GBM patients don’t survive past 2 years). I’m happy to hear that is starting to change. In 2007, a good friend of mine lost his mom to GBM in a matter of 24 hours (she died in the OR). In that respect, I feel very lucky to have had those two years with my mom. I think she would be really happy that preventative medicine is making more progress on the cancer front. If she were still here I think she would be leading the charge to for cardiology/radiology to collaborate with oncology.
Excellent blog post as always – however compliments to the readers, I must say i am startled to see how many people apparently have discovered and read Seyfrieds book, its a tough read, I read it as a preventive measure and thought nobody else would read it due to its density of information. Now I feel like a nerd…
Yes, Andre, I think it’s safe to say this is the dorkiest blog out there…
Dr. Abrass falsely links, in part, the reduction in the death rate of cancer since 1950 to mammography use when the most reliable, non-conflicted (by vested interests) studies found no discernible reduction in breast cancer mortality from its use (read Rolf Hefti’s e-book “The Mammogram Myth: The Independent Investigation Of Mammography The Medical Profession Doesn’t Want You To Know About”). He also puts much hope into gene sequencing and other genetic notions when it was found that not one disease has ever been successfully tackled upon knowing the entire human genome.
Abrass is merely another spoke of the medial orthodoxy who’s been teaching an erroneous, unscientific approach to healing in their doctrinaire mechanistic reductionism model. Hence, the war on cancer has been little more than complete failure. And not one chronic degenerative disease has ever been cured by the idiotic treatments of toxicity of mainstream medicine. Who, in their right mind, would ever expect a cure from such an unscientific approach? Modern medicine is great at bragging about their overblown advanced treatments. And they are great at denying and hiding some of the most severe harms of their products and services -due to their influential marketing few people are even aware of this.
With conventional medicine, which is a huge commercialized business, it’s mainly about treating disease (true prevention is practically meaningless to them), and the supposed looking-out for a cure. It’s almost all propaganda, helping for the unsuspecting public to keep donating huge sums of money to a illogical, profit-hungry business industry of disease to allegedly finding a cure. Keep dreamin’… or start to wake up.
Fiona, I’m pretty sure you didn’t read the same post I put up. You must have ready something else. I’ve read and re-read your comment twice (breaking one of my rules), and I’m convinced you’ve missed the point by about 175 to 185 degrees.
“With conventional medicine, which is a huge commercialized business…”
Unlike alternative medicine, which is well known for providing its treatments free of charge. Of course, it’s easy for alternative medicine to do this, because practitioners don’t need to pay for medical school, or for a medical license, and the makers of alternative “remedies” don’t have to spend millions of research dollars on clinical trials, or demonstrate the efficacy of their treatments to the FDA, or spend a lot of money creating new molecules in a laboratory when the ingredients they use are available on the nearest highway median.
Wait – they’re NOT giving the treatments away?
What a rip-off!
@ Dr. Attia: What exactly did I miss by such a wide margin? Please explain because I can’t see it as the post is about the war on cancer and my comments took a strike at the heart of the matter.
@ Alexandra M: Does me stating a fact (“With conventional medicine, which is a huge commercialized business…”) that the opposite (or anything else) applies to another related industry? Sounds like, based on your defensive illogical response, that you’re offended by what I posted.
Hi Peter,
Was going to write and plead with you to read Seyfried’s book about cancer as a metabolic disease – but looks like you’re aware of his work – thrilled about that.
Just finished listening to your Ted talk again. (It didn’t make your list but it’s top ten in my book 🙂
How shocking that one of our great artists, Tom Hanks, has Type 2 diabetes. And how disappointing that all he mentions about controlling his disease (that I’ve heard) is his weight – exactly the problem you discuss in your presentation.
How great would it be if he put his disease into remission with a ketogenic diet and then told the world about it?
I wish he knew your journey – insulin resistant in mid 30’s – but healthy later with a radical change of diet. So if anyone out there knows a guy, that knows a guy… that … knows Tom Hanks, please let him know!
Yes, Eric, I heard this the other day. Too bad. I’m sure the last thing Mr. Hanks would want is to hear from random folks like me. I do wish him well.
Peter,
Just want to thank you for all that you do. Your posts and talks and the approaches you take are what killed my fat-phobia, and helped me gain back my health. “Dorky”? No, they’re detailed and informative!
Really looking forward to your comments on Thomas Seyfried’s work, and the work coming out of NuSi!
Thank you, Monting. Whether “dorky” or “nuanced” or “detailed” … I like it!
It’s heartbreaking to hear all these stories about loved ones lost to cancer. I can’t imagine how awful it must be, given how awful it was losing a beloved cat to cancer earlier this year. I asked the veterinary oncologist how ketogenic diet could be implemented for cats, who are obligate carnivores to begin with (but you’d be amazed at the quantity of grain put into ordinary cat and dogs foods). He looked at me like I was nuts, even though I handed him a journal article about ketogenic diets to starve tumors of glucose.
Two months later, when my cat was having difficulty eating, I began mixing some butter into her food to make it easier for her to swallow, and to try to get some extra calories into her. When I told the vet he said, “Well, maybe those aren’t the best calories.” Which tells you a lot about how deeply entrenched the idea is that nothing – absolutely nothing – is worse for you (or your pet) than eating fat, not even slowly starving to death.
If you can find any solace in this, I’ve interacted with a few vets who have taken this approach with pets. They claim impressive results, though I don’t know if such outcomes are actually studied rigorously.
Peter, do you see any health benefit and/or drawbacks to a diet based primarily on “healthy” plant-based fats (nuts, seeds, olive oil, avocado, coconut) versus animal-based fat sources (lard, bacon, dairy, eggs, beef)? Thanks!
I don’t think so. Probably more of an individual question, rather than a general one, though.
Brian, I would note that fish seems to be one of the more important sources of fat. If you read more about omega-3s there is a difference between the omega-3s found in flax seed and the omega-3s found in fish. ALA versus DHA and EPA in particular if you are looking for some keywords. Not sure if your question comes from a particularly vegetarian/vegan point of view, but if there was one animal to eat for its fat it would be fish. You could also just supplement with a high quality fish oil. Not sure if Peter agrees with this but he does supplement with fish oil so I’m guessing he sees some further added benefit from this type of fat (or he’s just in the middle of experimenting).
Brian,
I have spent the last 50 or more hours reading the blogs and comments of Peter Dobromylskij (Hyperlipid) at https://high-fat-nutrition.blogspot.ca/. This blog is the MOST technical that I have ever seen and includes a lot of biochemisty in the blogs and the comments. Most of the commenters appear to be well educated scientists. I would recommend to start reading the blogs at the beginning, i.e. circa 2006, before GT book. Peter D is a high fat low carb proponent, but not too keen on veggies or PUFA’s inlcuding omega oils. He does supplement W3, but only a little. Check out the blog – very very interesting discussion, especially if you can persist in spite of the chemistry.
Not specific to cancer, but two excellent advocates of low carb, meat-based, grain free diets for cats are Drs. Elizabeth Hodgkins and Lisa Pierson. They cite some decent research, but as in human medicine research is dominated by commercial interests, especially the huge pet food industry. More impressive is their amazingly successful clinical experience. Diabetes and weight loss, of course, plus GI problems, allergies, urinary tract problems, and much else.
https://www.amazon.com/Your-Cat-Simple-Secrets-Stronger/dp/0312358024/ref=sr_1_1?ie=UTF8&qid=1381440613&sr=8-1&keywords=hodgkins+your+cat
https://www.catinfo.org
My current thought is that while cats are clear carnivores who handle carbs extremely poorly, dogs are more like us, having shared food with us for eons: tolerant of whole food carbs to a greater or less extent but not doing well at all on refined grain-based modern foods. Both of the vets I mentioned discuss the unique physiology of cats in relation to dietary needs and tolerances.
Hey Doc! Have you looked at the research regarding the effect of various fat sources have on tumor growth? Specifically, ketosis seems only beneficial if it’s (mostly?) fueled by saturated and mono-unsaturated fats.
I heard about it from this blog post: https://high-fat-nutrition.blogspot.com/2013/08/starvation-and-cancer-growth-sauer-vs.html “Palmitic, stearic and oleic FFA supplementation was inactive in promoting tumour growth. Linoleic and arachidonic promoted growth, really well. That is very scary.”
I’m frankly not smart enough to understand the significance of everything at that link, but those two lines stood out at me.
Thanks! I enjoy your posts.
Joshua, it’s not clear to me that this is necessarily true. Cancer is a pretty tricky disease, as I’ve learned from my personal research in oncology. What happens in vitro or in vivo in a mouse does not necessarily (or often) translate to a human.
Hello Dr. Attia
Have you heard of the Warburg effect? https://en.wikipedia.org/wiki/Warburg_effect
I have been talking to oncologists for years why they don’t test “starvation” like ketogenic states with cancer patients. Although oncologist researchers that know the Warburg effect told me it justifies research there have been to the best of my knowledge zero experiments with humans to date. However just recently a clinical study of brain cancer treatment with a ketogenic diet has been started in Israel in Ichilov hospital. So finally someone is paying atention to dear old Dr. Warburg and his simple idea.
https://www.cancer.gov/clinicaltrials/search/view?cdrid=669338&version=HealthProfessional&protocolsearchid=6891142
What do you think?
Guy
Yes.
Hi Peter,
Do you think there is any basis to low-carb diets being a) preventative in avoiding cancers, and b) recuperative in recovering from them? There seems to be some official looking information to this effect.
https://www.foodconsumer.org/newsite/Nutrition/Diet/low_carb_high_protein_diet_may_help_fight_cancer_0617110701.html
https://www.healthnewstrack.com/health-news-1451.html
https://www.sciencedirect.com/science/article/pii/S0005272810006857
https://cancerres.aacrjournals.org/content/early/2011/06/10/0008-5472.CAN-10-3973.short
Cheers, Mark (from Perth Australia)
Mark, I don’t know the answer, at least not in the same way I know when drop a tennis ball that it will hit the ground, but I do plan to address these questions eventually.
Hello Dr. Attica – thank you for your work! Curious- have you ever come across the work of Dr. Mark Rosenberg? I came across him while researching treatment options for my mom’s st V lung cancer. I was looking specifically for options that would include integrating ketogenic diet and found his facility in Boca Raton, FL –
https://www.antiagemed.com/programs/integrative-advanced-stage-cancer-therapeutics.php
He mixes alt therapies with low dose chemo (chemo customized thru tumor testing at Weisenthal Cancer Group – weisenthalcancer.com).
Finding treatment that emphasizes nutrition is difficult as you know and finding a nutritionist/dietician that doesn’t practice the standard model is rare. Even mention “Ketogenic” and I either get a puzzled look or a lecture on how dangerous it is to be on long term. Hoping you had some thoughts/comments. Thank you!!
I am not familiar with him, Diane.
Diane…Did you go see dr rosenburg? my dad with stage IV glioblastoma is thinking of going there in lieu of traditional chemo/radiation……how was your experience?
Peter,
Just in case you didn’t notice, ADA has officially removed the support for “balanced diet” for diabetes.
https://care.diabetesjournals.org/content/early/2013/10/07/dc13-2042.full.pdf
Yes, I did see this. Very interesting. Definitely a step in the right direction.
As I read the recent ADA position paper, I’m not sure I’d characterize it as a full step in the right direction.
My posture on T2D is that it’s a totally optional ailment that is trivially avoided with diet, is fully reversible with diet at the metabolic syndrome and pre-diabetic stages, and is often reversible after that, or is at least fully manageable primarily with diet. T1D is another matter.
The paper reads to me more like liability management – being mindful that the ADA has been, for decades, advocating a diet that causes T2D and keeps people on meds. The ADA is giving deminimus acknowledgement to what the grass roots have already figured out. This new ADA diet only slightly reduces the harm of the old one.
This quote pretty much says it all:
Page 2: “People with diabetes should consume at least the amount of fiber and whole grains recommended for the general public.”
We might ask Dr. William R. Davis, former diabetic, to opine on that :).
Page 14: “There is no standard meal plan or eating pattern that works universally for all people with diabetes.”
Notice that they fail in that sentence to differentiate T1D and T2D. The ADA seems to do that when it suits them.
New cases of T2D can easily be made to vanish.
T1D is going to be with us for some time, until its trigger is found and eliminated.
The ADA calls for more diet research. I read that as: today’s tiny half step means the ADA isn’t going to do anything substantial on diet and T2D for decades. I considered them to be a public health menace prior to this paper, and still do.
I think I’m mostly pleased that they have at least acknowledged that the dogma of eat all carbs, eat no fat has no evidence supporting it.