One night, as I alluded to in this post, Tim and I were having dinner and the topic of cancer came up. Personally and professionally I have a great interest in cancer, so when Tim asked if I could write something about cancer that was: (i) interesting to a broad audience, (ii) not technically over the top, (iii) not my typical 5,000 word dissertation, (iv) yet nuanced enough for his readers, I agreed to give it a shot, in about 1,000 words. (The content of this blog went up on Tim’s blog last week, but I’ve reproduced it here, less Tim’s commentary.)
Semantics and basics
Before jumping into this topic I want to be sure all readers — regardless of background — have a pretty good understanding of the ‘basics’ about cancer and metabolism. In an effort to do this efficiently, I’ll list concepts here, such that folks can skip them if they want to, or refer back as necessary. This way, I don’t need to disrupt the ‘story’ with constant definitions. (Yes, I realize this is sort of cheating on my 1,000 word promise.)
Cancer – a collection of cells in our bodies that grow at roughly normal speeds, but that do not respond appropriately to cell signaling. In other words, while a collection of ‘normal’ cells will grow and stop growing in response to appropriate messages from hormones and signals, cancer cells have lost this property. Contrary to popular misconception, cancers cells do not grow especially fast relative to non-cancer cells. The problem is they don’t ‘know’ when to stop growing.
Metabolism – the process of converting the stored energy in food (chemical energy contained mostly within the bonds of carbon and hydrogen atoms) into usable energy for the body to carry out essential and non-essential work (e.g., ion transport, muscle contraction).
ATP – adenosine triphosphate, the ‘currency’ of energy used by the body. As its name suggests, this molecule has three (tri) phosphates. Energy is liberated for use when the body converts ATP to ADP (adenosine diphosphate), by cutting off one of the phosphate ions in exchange for energy.
Glucose – a very simple sugar which many carbohydrates ultimately get broken down into via digestion; glucose is a ring of 6-carbon molecules and has the potential to deliver a lot, or a little, ATP, depending on how it is metabolized.
Fatty acid – the breakdown product of fats (either those stored in the body or those ingested directly) which can be of various lengths (number of joined carbon atoms) and structures (doubled bonds between the carbon atoms or single bonds).
Aerobic metabolism – the process of extracting ATP from glucose or fatty acids when the demand for ATP is not too great, which permits the process to take place with sufficient oxygen in the cell. This process is highly efficient and generates a lot of ATP (about 36 units, for example, from one molecule of glucose) and easy to manage waste products (oxygen and carbon dioxide).
The process of turning glucose and fatty acid into lots of ATP using oxygen is called ‘oxidative phosphorylation.’
Anaerobic metabolism – the process of extracting ATP from glucose (but not fatty acids) when the demand for ATP is so great that the body cannot deliver oxygen to cells quickly enough to accommodate the more efficient aerobic pathway. The good news is that we can do this (otherwise a brief sprint, or very difficult exertion would be impossible). The bad news is this process generates much less ATP per carbon molecule (about 4 units of ATP per molecule of glucose), and it generates lactate, which is accompanied by hydrogen ions. (Contrary to popular belief, it’s the latter that causes the burning in your muscles when you ask your body to do something very demanding, not the former).
Mitochondria – the part of the cell where aerobic metabolism takes place. Think of a cell as a town and the mitochondria as the factory that converts the stored energy into usable energy. If food is natural gas, and usable energy is electricity, the mitochondria are the power plants. But remember, mitochondria can only work when they have enough oxygen to process glucose or fatty acids. If they don’t, the folks outside of the factory have to make due with suboptimally broken down glucose and suboptimal byproducts.
DNA – deoxyribonucleic acid, to be exact, is the so-called “building block” of life. DNA is a collection of 4 subunits (called nucleotides) that, when strung together, create a code. Think of nucleotides like letters of the alphabet. The letters can be rearranged to form words, and words can be strung together to make sentences.
Gene – if nucleotides are the letters of the alphabet, and DNA is the words and sentences, genes are the books – a collection of words strung together to tell a story. Genes tell our body what to build and how to build it, among other things. In recent years, scientists have come to identify all human genes, though we still have very little idea what most genes ‘code’ for. It’s sort of like saying we’ve read all of War and Peace, but we don’t yet understand most of it.
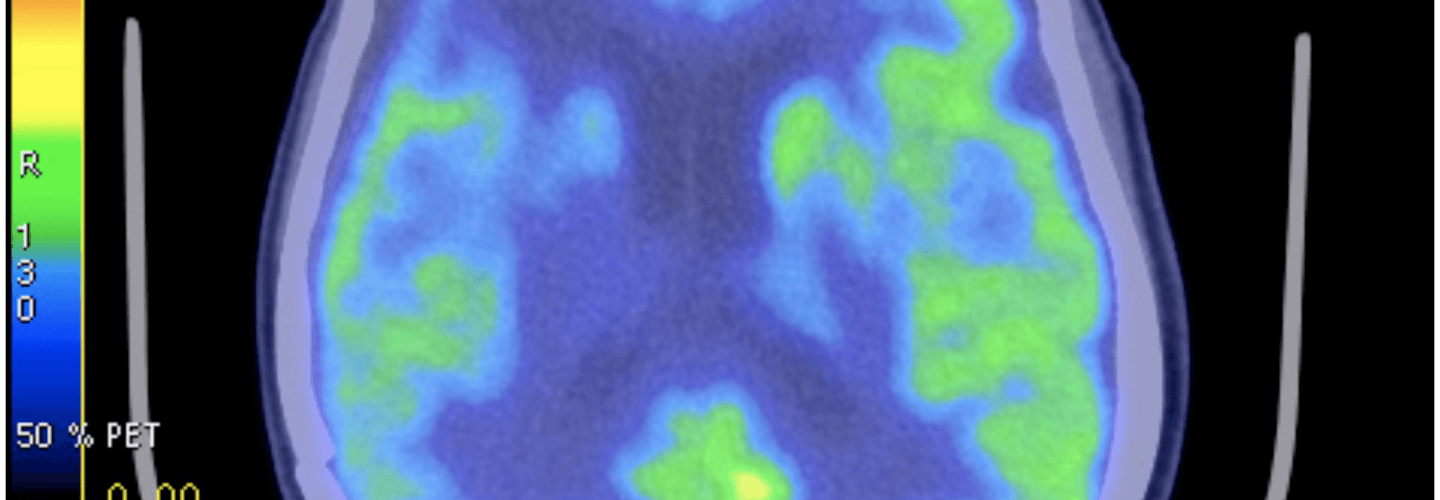
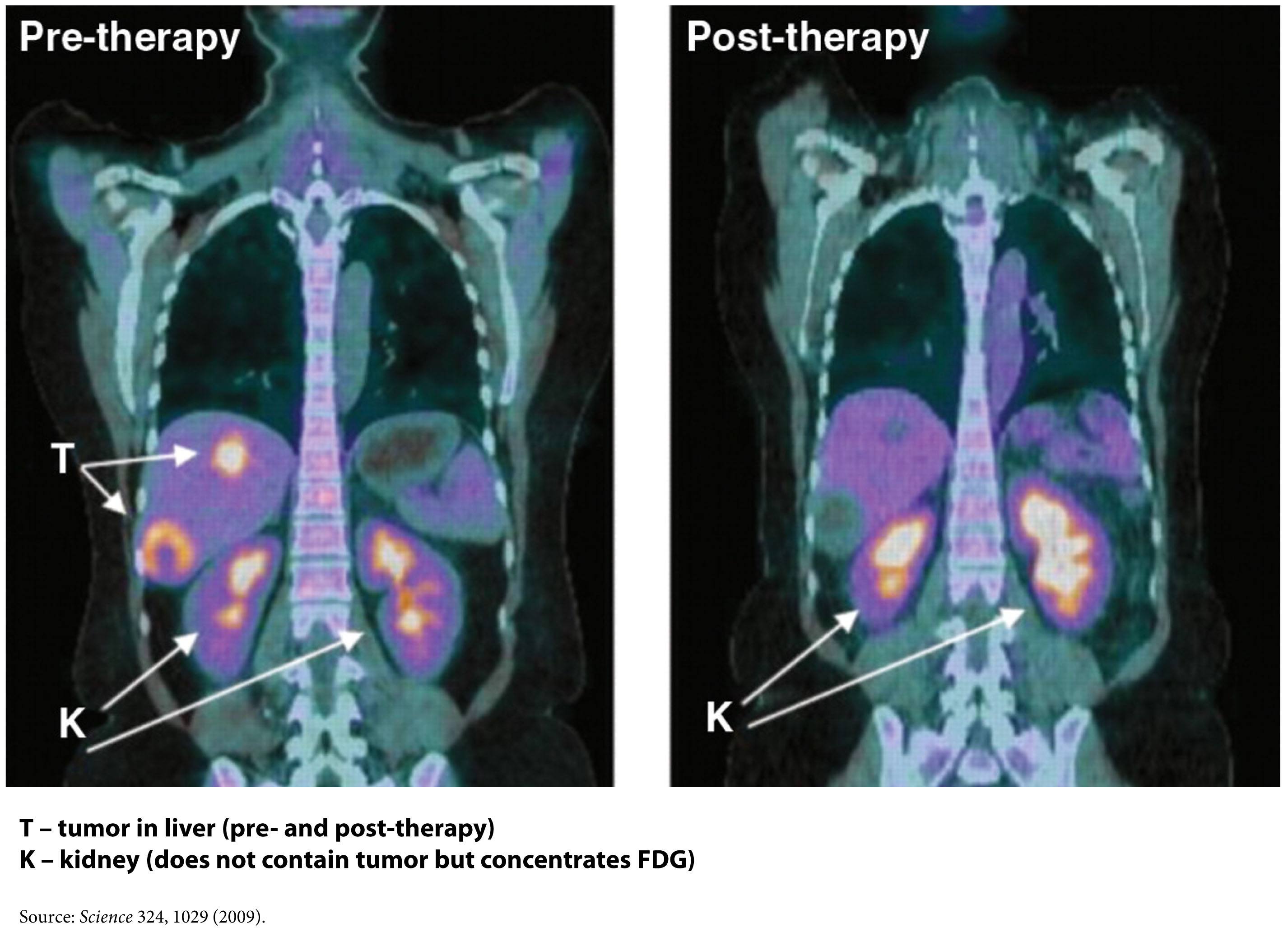
FDG-PET – a type of ‘functional’ radiographic study, often called a ‘pet scan’ for short, used to detect cancer in patients with a suspected tumor burden (this test can’t effectively detect small amounts of cancer and only works for ‘established’ cancers). F18 is substituted for -OH on glucose molecules, making something called 2-fluoro-2-deoxy-D-glucose (FDG), an analog of glucose. This molecule is detectable by PET scanners (because of the F18) and shows which parts of the body are most preferentially using glucose.
Phosphoinositide 3-kinase – commonly called PI3K (pronounced “pee-eye-three-kay”), is an enzyme (technically, a family of enzymes) involved in cell growth and proliferation. Not surprisingly, these enzymes play an important role in cancer growth and survival, and cancer cells often have mutations in the gene encoding PI3K, which render PI3K even more active. PI3Ks are very important in insulin signaling, which may in part explain their role in cancer growth, as you’ll see below.
The story (in about 1,000 words, as promised)
In 1924 a scientist named Otto Warburg happened upon a counterintuitive finding. Cancer cells, even in the presence of sufficient oxygen, underwent a type of metabolism cells reserved for rapid energy demand – anaerobic metabolism. In fact, even when cancer cells were given additional oxygen, they still almost uniformly defaulted into using only glucose to make ATP via the anaerobic pathway. This is counterintuitive because this way of making ATP is typically a last resort for cells, not a default, due to the very poor yield of ATP.
This observation begs a logical question? Do cancer cells do this because it’s all they can do? Or do they deliberately ‘choose’ to do this? I’m not sure the answer is entirely clear or even required to answer the macro question I’ve posed in this post. However, being curious people we like answers, right?
The first place to look is at the mitochondria of the cancer cells. Though not uniformly the case, most cancers do indeed appear to have defects in their mitochondria that prevent them from carrying out oxidative phosphorylation.
Explanation 1
Cancer cells, like any cells undergoing constant proliferation (recall: cancer cells don’t stop proliferating when told to do so), may be optimizing for something other than energy generation. They may be optimizing for abundant access to cellular building blocks necessary to support near-endless growth. In this scenario, a cancer would prefer to rapidly shuttle glucose through itself. In the process, it generates the energy it needs, but more importantly, it gains access to lots of carbon, hydrogen, and oxygen atoms (from the breakdown of glucose). The atoms serve as the necessary input to the rate-limiting step of their survival — growth. The selection of cancer cells is based on this ability to preferentially grow by accessing as much cellular substrate as possible.
Explanation 2
Cells become cancerous because they undergo some form of genetic insult. This insult – damage to their DNA – has been shown to result in the turning off of some genes (those that suppress tumor growth) and/or the activation of other genes (those that promote cell growth unresponsive to normal cell-signaling). Among other things, this damage to their DNA also damages their mitochondria, rendering cancer cells unable to carry out oxidative phosphorylation. So, to survive they must undergo anaerobic metabolism to make ATP.
Whichever of these is more accurate, the end result appears the same – cancer cells almost exclusively utilize glucose to make ATP without the use of their mitochondria. A detailed discussion of which explanation is better is beyond the scope of my word allotment, and it’s not really the point I want to make. The point is, cancer cells have a metabolic quirk. Regardless of how much oxygen and fatty acid they have access to, they preferentially use glucose to make ATP, and they do it without their mitochondria and oxygen.
So, can this be exploited to treat or even prevent cancer?
One way this quirk has been exploited for many years is in medical imaging. FDG-PET scans are a useful tool for non-invasively detecting cancer in people. By exploiting the obligate glucose consumption of cancer cells, the FDG-PET scan is a powerful way to locate cancer (see figure).
You can probably tell where I’m leading you. What happens if we reduce the amount of glucose in the body? Could such an intervention ‘starve’ cancer cells? An insight into this came relatively recently from an unlikely place – the study of patients with type 2 diabetes.
In the past few years, three retrospective studies of patients taking a drug called metformin have shown that diabetic patients who take metformin, even when adjusted for other factors such as body weight and other medications, appear to get less cancer. And when they do get cancer, they appear to survive longer. Why? The answer may lie in what metformin does. Metformin does many things, to be clear, but chief among them is activating an enzyme called AMP kinase, which is important in suppressing the production of glucose in the liver (the liver manufactures glucose from protein and glycerol and releases it to the rest of the body). This drug is used in patients with diabetes to reduce glucose levels and thereby reduce insulin requirement.
So, the patients taking metformin may have better cancer outcomes because their glucose levels were lower, or because such patients needed less insulin. Insulin and insulin-like growth factor (IGF-1) also appear to play an integral role in cancer growth as recently demonstrated by the observation that people with defective IGF-1 receptors appear immune to cancer. Or, it may be that activation of AMP kinase in cancer cells harms them in some other way. We don’t actually know why, but we do know that where there is smoke there is often fire. And the ‘smoke’ in this case is that a relatively innocuous drug that alters glucose levels in the body appears to interfere with cancer.
This may also explain why most animal models show that caloric restriction improves cancer outcomes. Though historically, this observation has been interpreted through the lens of less ‘food’ for cancer. A more likely explanation is that caloric restriction is often synonymous with glucose reduction, and it may be the glucose restriction per se that is keeping the cancer at bay.
Fortunately this paradigm shift in oncology – exploiting the metabolic abnormality of cancer cells – is gaining traction, and doing so with many leaders in the field.
Over a dozen clinical trials are underway right now investigating this strategy in the cancers that appear most sensitive to this metabolic effect – breast, endometrial, cervical, prostate, pancreatic, colon, and others. Some of these trials are simply trying to reproduce the metformin effect in a prospective, blinded fashion. Other trials are looking at sophisticated ways to target cancer by exploiting this metabolic abnormality, such as targeting PI3K directly.
To date, no studies in humans are evaluating the therapeutic efficacy of glucose and/or insulin reduction via diet, though I suspect that will change in the coming year or two, pending outcomes of the metformin trials.
Last point (beyond my 1,000 word allotment)
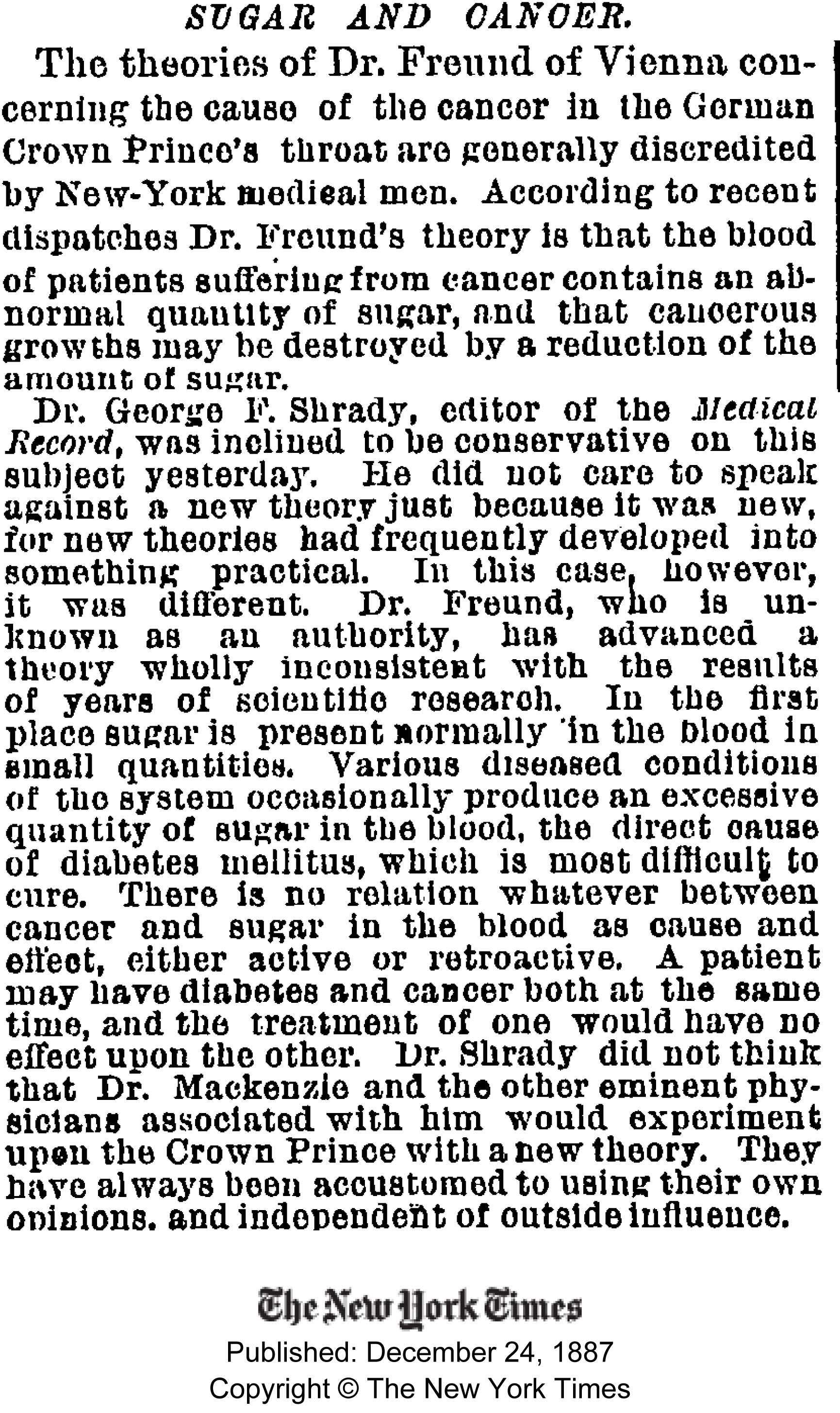
Check out this blast from the past! Gary Taubes, who is currently working hard on his next book, came across the article the other day from 1887.
Influences
I’ve been absurdly blessed to study this topic at the feet of legends, and to be crystal clear, not one thought represented here is original work emanating from my brain. I’m simply trying to reconstruct the story and make it more accessible to a broader audience. Though I trained in oncology, my research at NIH/NCI focused on the role of the immune system in combating cancer. My education in the metabolism of cancer has been formed by the writings of those below, and from frequent discussions with a subset of them who have been more than generous with their time, especially Lewis Cantley (who led the team that discovered PI3K) and Dominic D’Agostino.
- Otto Warburg
- Lewis Cantley
- Dominic D’Agostino
- Craig Thompson
- Thomas Seyfried
- Eugene Fine
- Richard Feinman (not to be confused with Richard Feynman)
- Rainer Klement
- Reuben Shaw
- Matthew Vander Heiden
- Valter Longo
Further reading
I do plan to continue exploring this topic, but for those of you who want to know more right now and/or for those of you with an appetite for depth, I recommend the following articles, some technical, some not, but all worth the time to read. This is the short list:
- Relatively non-technical review article on the Warburg Effect written by Vander Heiden, Thompson, and Cantley
- Science piece written about cancer (for non-technical audience) by Gary Taubes
- Non-technical talk by Craig Thompson
- Detailed review article by Tom Seyfried
- Review article on the role of carb restriction in the treatment and prevention of cancer
- Talk given by author of above paper for those who prefer video
- Moderately technical review article by Shaw and Cantley
- Clinical paper on the role of metformin in breast cancer by Ana Gonzalez-Angulo
- Mouse study by Dom D’Agostino’s group examining role of ketogenic diet and hyperbaric oxygen on a very aggressive tumor model
- Mechanistic study by Feinman and Fine assessing means by which acetoacetate (a ketone body) suppresses tumor growth in human cancer cell lines
Figure of FDG-PET imaging showing no evidence of recurrent tumor after standard care treatment including a water-only fast and a ketogenic diet by Zuccoli et al., 2009 is licensed under CC by 2.0

https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3047616/
What about an article like this the Reverse Warburg that says Ketones fuel tumor growth?
Thanks so much for this fine 1000 word overview of the subject how cancer cells feed. It was the suggestion I start on Enbrel for my AS (ankylosing spondylitis) and its connection with cancer development over time that got me to researching again. Funny part is I learned a low carb/protein but high fat (MCT type fats) was good for AS. After only 10 days on this diet my joint pain is down by 50%+ and my mobility is up by the same amount (subjective data 🙂 ) plus I have lost a couple pounds. This AM I blew a .023 BAC% reading (.125 on the metric scale) using a $15 meter off eBay but have more studying to do to understand the meaning of these acetone readings. I do hold an OD degree from SCO, Memphis TN 1986 which is helpful understanding research. Will read more of the links you added at the end. Thanks again!
Re: 2010 TED talk where Dr. William Li introduced the crowd to “anti-angiogenesis therapy”… https://www.youtube.com/watch?v=B9bDZ5-zPtY
Very cool. Kill blood supply, kill the cancer. Stop the blood supply from developing, stop the cancer from developing..
I read through this fascinating paper today that describes the mechanisms by which calorie restriction (CR) helps to fight cancer: https://www.cancerandmetabolism.com/content/1/1/10
Check these quotes out from the paper:
“Calorie restriction consistently and robustly decreases systemic leptin levels… Leptin… impacts angiogenesis…”
“Calorie restriction decreases chronic inflammation. The transcription factor NF-?B … is activated in response to … inflammatory molecules and is responsible for inducing gene expression associated with … angiogenesis.”
“PAI-1 is also involved in angiogenesis … Circulating levels of PAI-1 are consistently decreased in response to CR.”
Now consider:
In many ways, the ketogenic diet, when done correctly with the appropriate amount of protein, manipulates the exact mechanisms… Why?
Because the Keto diet mimics calorie restriction. It tricks the body into thinking that nutrients are scarce by keeping insulin, mTOR and leptin low… This puts the body into “maintenance and repair” mode – without starving you to do it.
Rosedale covers much of these concepts in this post: https://drrosedale.com/blog/2011/11/22/is-the-term-safe-starches-an-oxymoron/#axzz3CJOLVzQE
Keto diet – 2 birds, one stone.
Fascinating.
Love your blog. Thanks so much for the education.
Kelly T – Ft. Collins, CO
In April, after treatment and having no-evidence-of-disease (NED) for 11 months, our 11-year-old son was diagnosed with relapsed metastatic osteosarcoma (bone cancer) with inoperable tumors on his hip and spine. Osteosarcoma is a rare cancer to start with, and usually metastasizes to the lungs, where it can often be treated successfully with surgery. Our son has had no detectable lung metastasis, only in his hip and spine. This type of bone-only re-occurrence is called “multi-focal,” and it is observed in less than 2% of osteosarcoma relapses. There is no standard of treatment for this kind of multi-focal disease, and unfortunately, the statistical prognosis for this miserable disease after metastases is grim.
However, having been on a ketogenic diet (KD) myself for 2 years and after having read this blog post, I began immediately pushing for putting him on a KD as an adjunct to conventional treatment (chemotherapy and radiation). My wife was a bit skeptical until she saw the massive glucose uptake by these tumors in his initial PET scans. The oncologists and oncological nutritionists were both skeptical and fearful. (That’s another story.)
Keeping a child who has been used to carbohydrates and sweets his whole life on a KD has been a challenge, but we have been quite successful at it. As I had become proficient in baking with almond and coconut flours (and using sucralose as a sweetener), I was able to concoct low-carb high-fat substitutes for almost all of his favorite carb foods. Our goal was to limit his carbs to under 40g per-day, and he still gets plenty of healthy vegetables and protein. His routine laboratory tests have consistently shown blood glucose levels in the fasting range (60-90 mg/DL) and moderate to high ketones in his urine.
After the first two rounds of chemotherapy and 8 weeks on the KD, the smaller spinal tumors were undetectable on the PET scan and the PET activity of the larger hip tumor had decreased by 79%. After four-rounds of chemotherapy, the tumors had become undetectable by PET scan. After this scan, we started radiation therapy on his hip as well as adding a low-dose of metformin (500mg/day), and we are about to complete the seventh and final round of this chemotherapy.
The probability of the this particular chemotherapy being active against this disease was about 25% (and it was the best shot we had), so we are very pleased with the results so far. We cannot, of course, separate out the effects of the KD (if any) from the chemotherapy, but we believe that using a metabolic treatment in combination with conventional cytotoxic chemotherapy and radiation can only help. Nevertheless, as one oncologist told us, “you can fit a million cells on the head of a pin, and it takes about 1 centimeter of cells in a tumor to become visible on a PET scan,” so we know that “no evidence of disease” does not necessarily mean cancer free.
Going forward, there is no “conventional standard of treatment” for this disease. We are very interested in using hyperbaric oxygen in combination with a KD based on both the work of D’Agostino and researchers at MIT who have demonstrated that cancer cells can survive on glutamine in the absence of glucose in a hypoxic tumor environment, but not in an oxygen-rich environment. In addition to other chemotherapies, we are also closely watching developing immunological approaches to treating this disease.
Can’t wait until we have the right kind of clinical trails to give us answers to these questions. I suspect your intuitive is correct about multi-modality therapy–metabolic, cytotoxic, immunologic.
Very interesting Peter. I would like to add my understanding to the discussion. I’m not a scientist or healthcare professional, but I too have tried to look at the subject of Cancer with fresh eyes – in much the same way you have with diabetes.
IMHO Cancer is all about oxidation of biomolecules leading to cellular dysfunction via DNA/RNA mutation. All aerobic organisms have had to develop anti-oxidant defence mechanisms against pro-oxidative internal processes and external carcinogens. Our cell membranes, proteins and RNA/DNA can be severely compromised by these actions. Our defences are now being overwhelmed by an environment containing hundreds of pro-oxidative sources. I also think there is a major modern co-factor which is being over-looked.
All the observed effects(glucose utilization, disrupted apoptosis, unchecked cell growth etc) are (IMHO) simply symptoms of dysfunction. My own research has identified all the main causes of Cancer as being generators and promoters of Reactive Oxygen Species(ROS) free radicals (Superoxide, Singlet O2, Hydrogen peroxide and Hydroxyl – amongst others). These ROS are generated both endogenously and exogenously via dozens of mechanisms in huge quantities(by the trillion?). All the main carcinogens (Ionizing radiation, UV, Smoking, Alcohol), as well as a considerable percentage of the IARC Class 1 carcinogen list , all contribute to DNA mutation via ROS.
Is this just a coincidence?
I don’t want to explain too much in a single comment, but I think I can explain all of the characteristics of cancer(increased incidence in the elderly, overall increase in incidence, association with modern life, same promoter causing multiple types of cancer, metastases, spontaneous remission, cancer in the young, poor treatment outcomes and survival rates, dietary and lifestyle factors and more) in a single unifying theory.
Apologies if this is a little short and matter-of-fact. It’s a huge subject which is difficult to do justice in a couple of paragraphs and your TED talk suggested more ‘straight talk’ to be beneficial to the debate.
Here is a link supporting this by a Harvard trained surgical oncologist:
https://www.integrativeoncology-essentials.com/2013/02/an-over-the-counter-ancient-medicinal-berberine-fights-cancer-and-diabetes/
Peter, I’ve read your post with great interest. In it you say “Over a dozen clinical trials are underway right now investigating this strategy in the cancers that appear most sensitive to this metabolic effect – breast, endometrial, cervical, prostate, pancreatic, colon, and others.” Since some time has passed since you posted your piece, do you have any information about the progress or outcomes of these trials? I’d really like to know who to contact to get more information.
I have stage IV pancreatic cancer (exocrine) with metastases in both lungs. I was diagnosed about 14 months ago. My diet is focused on getting plenty of protein and vegetables, is not low-fat, and does include grains and fruit, with occasional treats that have sugar. My oncologist has said that she does not recommend that I go on a Paleo diet and that my current diet is fine, but I’d like to hear your thoughts on this. Do you think that I should go on a KD? If so, can you point me in the direction of any legitimate (not based on anecdotal evidence) studies that demonstrate the advantage of KD for someone with pancreatic cancer? Also, if so, what % of calories should be carbs? I’ve seen one KD that suggests carb intake should be 2-4%, which seems very low and would be quite difficult to maintain. Anything you can provide will be much appreciated! Thank you!
p.s. Since the beginning, I’ve been taking 1000 mg of Metformin/day
Sorry to hear about diagnosis. There really are no studies pointing definitely to one diet or another. But it’s hard to make the case that a diet that promotes hyperinsulinemia is the right choice in the case of most cancers.
Here’s a recent paper on ketogenic diet and cancer (published earlier this month):
PLOS|ONE: Non-Toxic Metabolic Management of Metastatic Cancer in VM Mice: Novel Combination of Ketogenic Diet, Ketone Supplementation, and Hyperbaric Oxygen Therapy
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0127407
Yeah, mice, but still. And note that the diets were ad libitum, and not calorie-restricted as might be expected if you’ve read Seyfried’s book.
The exogenous ketones used in the trial may not be generally available, but there is one commercial product available from time to time (Patrick Arnold’s KetoForce). Dilute H2O2 has also been suggested as an alternative to hbO2.
One of the paper’s authors (D’Agostino) has a web site with links to useful resources.
re: Do you think that I should go on a KD?
Do not expect anyone to give you a definitive answer, and if they do, question it. Anyone who distrusts the Standard of Care, based on the apparently dead-end somatic theory of cancer, needs to fully take charge of their own case, do their own research, and make their own decisions.
Recent research shows that high levels of growth factor significantly increase the risks of colorectal, breast, and prostate cancer. It also has been determined that a protein that binds to the growth factor seems to neutralize it and reduce the risk of these malignancies. My question being, how does Sermorelin use tie into these findings? It was my understanding that Sermorelin use leads to higher levels of growth hormone which slows the aging process, thus, reducing cancer risk. In light of this research, however, it seems that just the opposite has been proven.
I would not consider sermorelin to be a longevity agent. Things that increase GH later in life likely reduce longevity.
I’m under the impression that Cancer patients often die from Starvation most directly. At one point in history, measuring ketones on the breath was even a (late) measure suggesting cancer. If this is true, am I right to suppose that inducing nutritional ketosis may be of limited use to a later-stage patient? Perhaps that’s irrelevant and certainly not a rebuttal against prophylatic ketosis. Also, would it be beneficial for a keto-adapted person to consume glucose prior to a FDG-PET scan? Otherwise, it seems like a false-negative (“miss’) could occur.
The starvation symptom in the final stages of cancer has been referred to as “wasting away”. It’s known as cachexia: https://en.wikipedia.org/wiki/Cachexia
Cancer cachexia represents the replacement of specialized cells which burn glucose and fat with do-nothing cells which ferment only glucose. It’s no coincidence that this transition happens in an insulin-resistant environment with way too much glucose. It represents the replacement of human cells which are incapable of importing the abundant glucose with cancer cells which use the glucose.
A ketogenic diet has been known to work.
The rEally great thing about a ketogenic diet for cancer is that it has no down side. Switching from carb ingestion to fat ingestion does not rely on the chemical pathways argued back and forth between Warburgh advocates and consensus oncology.
Trying a ketogenic diet for cancer merely relies on the fact that humans can use either fat or sugar, but cancer can use only sugar.
Sure, the pathway science is quite important in defeating the wrong-headedness of the cancer-is-genetic crowd, but it’s not necessary for any individual cancer patient.
Hi Peter, I’m a grad student training to be an epidemiologist at a top-ranked US public health school and I am a HUGE fan of yours and Gary Taubes’ work. For years, my dream has been to work with NuSI to test these Warburg/excess glucose/cancer theories. If there really is a causal effect between glucose/sugar and cancer, the implications are so massive, we might have another cigarette smoking > lung cancer type situation on our hands. If a link like that can be established, then bigger changes in policy and public opinion and surgeon general’s reports etc. could one day happen. I am super passionate that this theory HAS to be tested and the experiments to prove it have to be expertly designed. Please contact me if NuSI is looking for a dedicated worker for this cause. I would be willing to put in tons of hours and work for low or no wages. Thanks!
Garrett, I’m no longer at NuSI.
Peter, what happened (NuSI)?
I am no longer at NuSI.
Hi Dr. Attia,
Your last comment was a surprise to me. What happened at NuSI? Are you still intimately involved in nutritional research?
No, I am no longer at NuSI.
I’d love to know what happened too. This is a bit of a downer to my day. That said, david bowie recently died and even more recently the mighty dons were found guilty in the ASADA/WADA supplemets scandel. So life has been worse.
I get the feeling you don’t want to publicly say it, but this has shaken my faith in NuSI a bit. You can always email me, or message me on twitter or facebook. I won’t tell the world (I haven’t got my radio show anymore, had to quit that 🙂 …….year 12 and footy was too time consuming)
for what’s it’s worth, your interest in nutrition lit my passion to become involved. I will be submitting my research proposal spring of this year focusing on nutritional ketosis, so I can evaluate this further during my residency in dermatology. I hope you pick back up this endeavor at some point, as you have enlightened many people to think and question dogma. Thank you.
Thanks, Michael. I’ll be as involved as ever in the space of health, but my interests have grown quite a bit broader than nutrition.
I have followed you for years, I have asked my doctor for an “upgraded” blood work but he doesn’t know what to do with it…any suggestions, where can I go to have someone look at LP(a), ApoB, etc.. and make sense of it all?
What?! I thought NuSi was a ‘legacy’ project?!
Hi Peter,
I’m sure your readers would appreciate if you could do a short post on “why I left Nusi”. Thanks
Dear Dr. Attia:
I’m a medical student at Stanford going into radiation oncology, and I’ve seen an increasing number of patients adopting ketotic diets. Often times the question of how this metabolic state can affect their radiation treatment comes up, so I was wondering if you knew of any relevant literature.
Thanks,
Palak
Check with Dom D’Agostino. He’s looking into this question.
throw us a bone. Its been 51 weeks since you posted a new story on here.
How about a podcast that just got posted today? https://chriskresser.com/the-keys-to-longevity-with-peter-attia/
And what a podcast it was! Excellent discussion on longevity and one that requires a more in depth conversation, perhaps on a subsequent podcast. I’m curious about the change in direction on the nutritional aspect though?