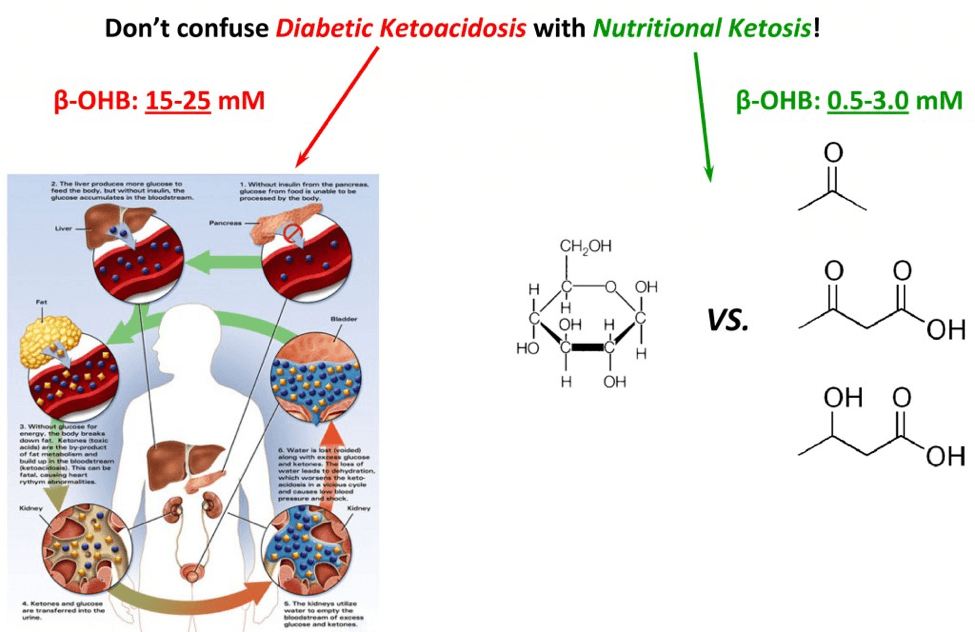
You may have heard from your doctor that ketosis is a life-threatening condition. If so, your doctor is confusing diabetic ketoacidosis (DKA) with nutritional ketosis, or keto-adaptation.
First, some semantics. Our body can produce, from fat and some amino acids, three ketone bodies (a “ketone” refers to the chemical structure where oxygen is double-bonded to carbon sandwiched between at least 2 other carbons). These ketone bodies we produce are: acetone, acetoacetone, and beta-hydroxybutyrate (B-OHB). [For anyone who is interested, they are the 3 most right structures on the figure, below.]
Why do we make ketones? For starters, it’s a vital evolutionary advantage. Our brain can only function with glucose and ketones. Since we can’t store more than about 24 hours’ worth of glucose, we would all die of hypoglycemia if ever forced to fast for more than a day. Fortunately, our liver can take fat and select amino acids (the building blocks of proteins) and turn them into ketones, first and foremost to feed our brains. Hence, our body’s ability to produce ketones is required for basic survival.
What is diabetic ketoacidosis? When diabetics (usually Type I diabetics, but sometimes this occurs in very late-stage, insulin-dependent, Type II diabetics) fail to receive enough insulin, they go into an effective state of starvation. While they may have all the glucose in the world in their bloodstream, without insulin, they can’t get any into their cells. Hence, they are effectively going into starvation. The body does what it would do in anyone – it starts to make ketones out of fat and proteins. Here’s the problem: the diabetic patient in this case can’t produce any insulin, so there is no feedback loop and they continue to produce more and more ketones without stopping. By the time ketone levels (specifically, beta-hydroxybutyrate) approach 15 to 25 mM, the resulting pH imbalance leads to profound metabolic derangement and the patient is critically ill.
But this state of metabolic derangement is not actually possible in a person who can produce insulin, even in small amounts. The reason is that a feedback loop prevents the ketone level from getting high enough to cause the change in pH that leads to the cascade of bad problems. A person who is said to be “keto-adapted,” or in a state of nutritional ketosis, generally has beta-hydroxybutyrate levels between about 0.5 and 3.0 mM. This is far less than the levels required to cause harm through acid-base abnormalities.
Keto-adaption is a state, achieved through significant reduction of carbohydrate intake (typically to less than 50 grams per day) and moderate protein, where the body changes from relying on glycogen as its main source of energy to relying on fat. Specifically, the brain shifts from being primarily dependent on glucose, to being primarily dependent on beta-hydroxybutyrate. This has nothing to do with what a diabetic patient is experiencing in DKA, but does illustrate how poorly informed and quick to react the medical community is. DKA and nutritional ketosis (or keto-adaptation) have as much in common as a house fire and a fireplace.
Photo by Andrew Yardley on Unsplash







Hi Peter,
I have type 1 diabetes and I am moderately active (3-4 hours per week of cardio). After years of low carb eating, I have dropped my carbs (four weeks ago) to about 15 grams per day and protein is 60 g per day, and I notice I am requiring more insulin than before (basal change from 12 units per day, increased to 14 units per day).
With normalized blood sugar, is there any risk?
I read that with more ketone bodies one might require more insulin. Is that what could be going on?
Do I need to increase carbs?
Will the presence of this extra insulin slow down fat loss? I am a little concerned that I have not seen a weight(fat) change.
I am thinking my basal insulin might be bad (ineffective). So that would explain a lot!
It would be fine to take off this comment and the following one, as the questions were invalid due to my bad insulin. THank you! Robyn. 🙂
<>
Does this quote suggest that a well-controlled type one diabetic cannot or should not do a ketogenic diet? It has been interpreted by some pretty well-informed people as so. I believe that as a type one, I am safe to go ketogenic, and it is indeed my best treatment option as it keeps my glycogen from dumping into my system (especially in these peri-menopausal years.)
Hi Robyn,
I’m not Peter, nor an MD, and of course I can’t respond for him or make any medical suggestions.
But Peter has often referred to the book about diabetes and low-carb diet by Dr. Richard Bernstein, who is an MD, and a Type 1 diabetic, who specializes in diabetes. You may find it worthwhile to look into it. It’s on Amazon.
Bob.
Correction to my question (and my quote did not show up!) I have been very tired due to bad insulin and did not articulate myself very well. The quote I meant to include mentions type one diabetics being in danger when having too many ketones. I think Peter meant that if our sugar is up, then it would be likely ketoacidosis. What was a little confusing was the interpreted idea that we cannot keto-adapt without a risk of keto-acidosis. A very good blogger had received some information that led him to believe a type one cannot keto-adapt. I believe this is not so. Although I have been testing for urine ketones, I have ordered the blood tester for beta hydroxy butyrate. I believe I can still keto adapt and the comments about type one diabetics refers to those not eating low-carb with normalized blood sugar.
And indeed the Bernstein book has been my guideline for some time, thank you. Agreed it is the best book EVER for diabetics. I just was following it with a slight misunderstanding of carb count and a life too busy to keep my diet consistent. I really have NO room for error without some huge blood sugar consequences, at this stage in my life. Now that I have lowered carbs to about 18g I am having much tighter control. The exercise physiology behind low carb was a mystery to me too, and got me into some hot water in the past. Now that I understand more about fat, beta hydroxy butyrate and carb fueling conditions I am hopeful to live with freedom to exercise more when I like without fear of lows.
Peter,
I’ve been reading your blogs about cholesterol, ketosis and lipidology and I thank you for taking the time to write this stuff.
I’ve been trying out a low carb diet for the last month+ and have succeeding in getting fasting ketone levels of 15 – 40 mg/dL (so 0.5 ~ 2.1 mmol/L), which is great. I’ve been testing with a urine tester, however, which seems to indicate that it is checking acetoacetic acid. Your blogs talk about beta-hydroxybuterate, though and so I’m wondering if acetoacetic acid is a meaningful proxy.
Given that you seem to geek out on how various things are tested, I was imagining you would probably have a blog post on how ketones are measured via urine versus via blood versus whatever; but I have yet to find it. Am I just bad at finding stuff on your blog, is there another post somewhere else that you recommend for understanding how that works, and/or can I request a blog post discussing this?
Hi
I am 2 weeks into the Lighter Life diet. I wanted to kickstart. I followed the Atkins diet some years ago and I know from experience that it works. I tested my ketone level yesterday and found it was .5
Today it is .3 and I have gained 2lb even though I have been religiously sticking to the diet.
Can you explain why this would happen?
Hey, quick one. I had heard it is common to find toxic substances in fat; the main point being that in the body any sort of environmental toxic threat could be directed to storage in fat since fat is a chemically neutral environment? I cannot find any seemingly credible sources to justify this or not but was curious if you had come across any literature that suggested risk from high fat diets because of this statement?
Thank you kindly.
Hello Peter,
I have been living with T1D for over 24 years and I am 41 years old. I am the mother of two and I enjoy running road marathons (PR 3:37) and have completed several ultra-marathons. I wear an Omnipod insulin pump for insulin delivery and a Dexcom CGMS.
Recently a good friend’s son was diagnosed with a brain tumor and it was recommended that he include a KD as part of his treatment protocol. I was incredibly curious about this diet and began my research immediately. IAfter checking with both my primary care physician and my diabetes specialist doctor I began the HFLC way of eating last Monday, 6/30/14.
I have been showing urine ketones in the level of 0.5 mmol/L – 4.0 mmol/l for 6 days. My glycemic control has been incredible for the past 8 days. I have remained mostly in the 70-110 mg/dL range with my highest blood sugar at 168 mg/dL. As expected, I have reduced my TDD insulin requirement significantly, from around 25-30 units/day to 12-17 units/day. Most days this is 100% basal insulin but I am still adjusting rates. Exercise is particularly challenging at this time of transition. Prior to HFLC eating I would turn down my basal rate 50% for 1.5 hours 30 minutes prior to my run. I would consume a GU packet (22 CHO) about 45 minutes into the effort, depending on the blood glucose trend. Of course it wasn’t always this predictable but you get the picture. Since I began HFLC eating I am trying to figure out how to adjust basal insulin, intensity and duration to remain in stable blood glucose control. I have successfully ran several 3 mile runs doing this with varied intensity.
After dinner last night my blood sugar rose from 80 mg/dL to 149 mg/dL. Instead of taking a bolus dose of insulin to correct the 149 mg/dL down slightly I decided to watch the impact of a newly adjust basal rate through the night. I held at 149 mg/dL for the next 5 hours, completely stable. This morning I woke up to join my running group for our Tuesday track workout and my ketone levels upon urine testing were darker purple than they had been for the previous 5 mornings, possibly 8.0 mmol/L. This concerned me, as my doctors have always advised against exercise if ketones are present and I wasn’t clear why the ketones level had increased. My son also had the flu last night and that was another area of caution from my doctors. Infection/sickness can cause a T1D to enter into DKA rapidly. Though I felt fine, I just didn’t feel comfortable with my understanding of why the ketones would increase, what my risk was as a T1D athlete and how to accommodate to remain in nutritional ketosis. If I felt I was heading toward DKA I would take a dose of insulin and eat carbs as my blood sugar needed.
My questions:
How does my reduced insulin levels impact my risk for developing DKA even with blood sugar levels below the typical “alert” level of 250 mg/dL? How does exercise impact this already existing risk of decreased insulin and ketones being present? What is the ketone threshold of caution for a T1D utilizing the HFLC way of eating?
Cheers, Terra
Complicated question, and not one I can really get into without playing “doctor,” which I can’t do via a blog. T1D is tricky for nutritional ketosis, and requires supervision. It sounds like you have good insight. The reason someone with T1D can get into DKA, while someone without it can’t, is that at high enough levels of BHB, insulin is secreted (in the non-T1D) which acts as a negative feedback loop.
Hi Terra,
I’m also a T1D (First time I’ve ever typed it that way, though…) and an athlete. I just started the Ketogenic Diet and on my 1st morning, got the deep purple stick.
Have you found any more info. on the web that’s specific to T1Ds? I feel like this diet is ideal for me in regards to both my diabetic management (on the first day, my BG sat at 89 all day with only 3 units of Novalog in the morning) and also in regards to my athletic aspirations. I’m running a Ragnar Relay in June and don’t want to let my team down.
Thanks so much.
-Mark
Blood ketones 5.9 o.0
Hi Peter,
I am a 12 year type 2 diabetic that went low carb in January then lost 20 lbs after ditching grains and most dairy. I managed to get off of my metformin at the end of March and am now running around 5.5 on HgbA1c. In early December it was 7.9 while on 2,000 mg Metformin ER. I switched to lchf in early June because of a plateau that began April 12th. Nothing has worked to break it to date other than I tried consuming eggs and fat for a day and a half last week and that bumped my ketones higher and I dropped a whole pound, lol.
Today I checked my ketones this morning and they read 3.1 with a fasting glucose of 106 but now at bedtime (it is late at 1:30am) I am at 5.9 and my glucose is106. Is that number a cause for concern? I just got a small snack to bring that down before bed because that number makes me feel a bit nervous before sleeping even though I feel fine. I just want to stay between 1.5 and 3.0. I have been researching everything to understand what is causing my plateau and I am now thinking that being diabetic and obese that I may have sluggish or possibly fatty liver issue though no doctor has ever mentioned it to me.
Today’s menu consisted of
breakfast: bullet proof coffee with 1T kerry gold butter and 1 T coconut oil, 2 eggs, 2 extra T coconut oil on top of coffee;
lunch: 2 eggs, bpc with 1 T. ea of kerry gold butter and coconut oil;
dinner: grass fed ribeye 4 oz, 1/4c steamed cauliflower, 1/4c, sauteed mushrooms., 1/2 delicata squash with 1/2 T butter.
Can you shed any insights into whether I am right about needing liver support and healing to lose more pounds?
I love this way of eating and don’t want to see my glucose rise again if I add back more carbs. Any comments would be appreciated 😀
Thanks!
Hi Peter,
I’ve been on the KD for 8 months, and I feel it has improved my health significantly
What I’m having trouble with is that somehow the KD has made my stress response bigger. For instance I have bouts of adrenaline/angst while driving, or sitting in class, and I previously did not have these problems. Like I said, I otherwise feel much healthier.
Can you think of any nutritional reasons why this might be the case?
What do you think about supplementing potassium? (All I could think of as an explanation is a high sodium-potassium ratio)
Thank you for your time!
Hi Peter,
I am a student of clinical herbology as well as holistic nutrition and wellness. My particular interest is in cancer prevention and treatment. I am confused. Everything I have studied thus far clearly states an alkaline state prevents the proliferation of cancer. In Ketosis isnt the body in a more acidic state? I understand it will not have the glucose needed to fuel cancer growth but what about the pH level? Im so glad I found your blog. Thanks for all of your expertise and guidance.
Kasey Bordas
Kasey, I’ve addressed your questions elsewhere in the blog and comments.
Hi Peter,
What do you make of elevated norepinephrine levels and high blood pressure when on the ketogenic diet. Is this cause for concern, or is it common and transient?
Thank you
Haven’t seen it. That usually speaks (if clinically significant) to pheo.
Hi Peter.
I just got back from an urgent care visit with my 3 year old daughter. We thought she might have a UTI. We brought her in and they did a Urine test. No UTI, just rash from a lot of pool time, causing stinging and withholding. But the doctor was concerned with the level of Keytones in her urine. There was no glucose in her urine, but he started mentioning diabetes as a primary cause for ketones in the urine. We have been on a mostly paleo diet for about 6 months that has basically solved my joint inflammation issues and my daughter’s instant constipation when she eats food with flour or starch – so we are pretty happy with the outcomes. That said, are there “normal” levels of keytones to be expected in the urine when on a diet like this? Is the doctor right to be concerned? Thanks for all this info, this story and blog made me a little less worried.
Impossible for me to say without knowing everything and seeing all lab values.
This morning, I’m at 6.0 mM ketones. Should I be worried? Should I intentionally bring it down? I’m not diabetic of any kind, but this high a number makes me nervous. (And no, I’m not starving.) Thanks for any help! 🙂
Thank you so much for your excellent article! I have not been able to read through all 400+ comments above so please forgive me if you have already addressed this question.
My husband is a Type 1 insulin-dependent diabetic. He has witnessed the great benefits I have experienced by being on a ketogenic diet over the past several months and wants to join me. If he cuts out most of his carbs he finds that he needs little to no insulin. Can he reach ketosis or will he become sick by taking little to no insulin? Can a Type 1 diabetic reach nutritional ketosis or are their bodies unable to reach this state? Thank you for all the information on your website – much appreciated!
Varies by case and needs a smart endocrinologist to be involved.
Hi Dr. Attia,
Please put me down as one more reader who would love to see your take on the low carb/keto relationship to hypothyroidism debate. I did find on Jimmy Moore’s site a presentation of the two sides of the issue, with interviews with Chris Kresser and Volek/Phinney. There are few references to this issue in the above string and it sounds like an issue you are thinking about. Any info would be much appreciated!
Thank you for all the well presented info!
Jesse
You mention in your article that a person in nutritional ketosis normally has B-OHB in the region of 0.5 – 3.0. For the past 5 or 6 weeks My blood tests have been ranging from 4.0 – 6.0 with my blood glucose being steady around 4.0- 4.5. I stopped losing weight and added extra calories about 4 weeks ago. I am consistent about being around 20g carbs and eat about 75-80% fat and about 1g protein per kg weight. Are my ketone measurements too high and if so how do I reduce them without putting on weight??
Hi Peter,
Your blog was recommended to me by a friend who has started a ketogenic lifestyle to lose weight and it certainly has a plethora of interesting information in it. My friend has recommended I start this type of diet because I am an endurance athlete. I am a competitive marathon runner and Ironman athlete and he says by being in a state of ketosis I will not have to take food with me on long training runs or during my races. I have to confess I find it hard to believe that I could run a 3.5 hr marathon without food and am even more skeptical I could survive an 11 hour Ironman simply by surviving off my own body fat (which is at a healthy 18% according to my latest PodPod results – 46 year old female).
I eat a varied whole foods diet that consists of fruits, veggies, nuts, seeds, oils, lean meats, diary, legumes and grains. I rarely eat anything out of a box or a bag so my ingestion of wheat & refined sugars is very limited except for the high sugar chews I take on training runs over 16 miles and bike rides covering 60 miles or more. Since weight loss is not a concern what would the benefits of a ketogenic diet have on me and my endurance performance?
Thanks!
Dr A.
I’ve been reading your blog and started eating a ketogenic diet about 3 months ago.
My new blood labs showed that it has SLASHED my Small LDL P levels in half. From 1000 to 500!
But……………My liver enzymes are now elevated. ALT = 69, AST = 42
Can beginning a ketogenic diet lead to elevated liver enzymes?
Hi, great article.
Just wondering what your references are for this? Not because I’m questioning you, but because I would like to use some of this information in my uni assignment, and they will not accept a website reference. Any texts or journal articles that explain this would be great, I have looked but without a lot of success.
Thank you 🙂
Hi, i was wondering if the type of diet your using is similar to what the Marine Corp uses at paris island for new recruits. They typically are consuming high calories in a day. For example a MRE contains 3500 calories in one MRE.
I remember my son writing telling me that they load them up on milk, eggs, bacon, very very little bread, for breakfast at the camp and then off to training they go. But the Corp breaks their bodies down, removes the fat, then builds up muscle and not much of that but conditions the muscle to becoming denser tighter.
James, I think Maggie just KO’d you lol