Check out more content with sleep expert, Matthew Walker, Ph.D.:
- (April 1, 2019) Part I of III: Dangers of poor sleep, Alzheimer’s risk, mental health, and memory
- (April 8, 2019) Part II of III: Heart disease, cancer, sexual function, and sleep disruption
- (April 15, 2019) Part III of III: The penetrating effects of poor sleep from metabolism to genetics
- (June 17, 2019) AMA #1: Strategies for sleeping more and sleeping better
- (October 28, 2019) AMA #2: short sleep mutants, optimal sleep environment, & sleep apnea
- (August 31, 2020) Sleep & Covid-19: Sleep and immune function, chronotypes, and hygiene tips
- (September 7, 2020) AMA #3: Fasting, gut health, blue light, caffeine, REM sleep, and more
In part 2 of this 3 part series, Matthew Walker, professor of neuroscience at UC Berkeley and expert on sleep, describes the preponderance of evidence linking poor sleep to cardiovascular disease, cancer, and sexual function. He also details the impact of cortisol on our nervous system contributing to sleep disturbances and insomnia as well as the efficacy and risks associated with the most common sleeping pills. Matthew also describes the sleep needs of teenagers and urgently lays the case that we should reconsider school start times. We also get into the effect of electronics at night, the efficacy of napping, the general impact of modern society on our sleep habits, and what changes we can make to course correct.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Sleep and cardiovascular disease [6:00];
- Fuel partitioning and dieting while sleep deprived [16:45];
- Sleep and the reproductive function: testosterone, sperm count, FSH, menstrual cycles, and fertility [19:45];
- The biological necessity of sleep, the lack of a “safety net”, sleep debt, and ways to course correct sleep problems [23:45];
- Fighting cancer and improving immune function with sleep [34:30];
- The medical profession: A culture that devalues sleep [47:30];
- The sleep needs of children, the travesty of early school start times, electronics at night, and advice for parents [1:04:45];
- How exposure to light affects sleep, and how modern society has changed our sleep habits [1:26:15];
- Is napping helpful? [1:36:00];
- The effect of cortisol levels on sleep [1:41:15];
- Are sleeping pills doing more harm than good? [1:52:15]; and
- More.
Sleep and cardiovascular disease [6:00]
Why is CVD worsened (or accelerated) by sleep deprivation?
Example: Daylight savings time and myocardial infarction
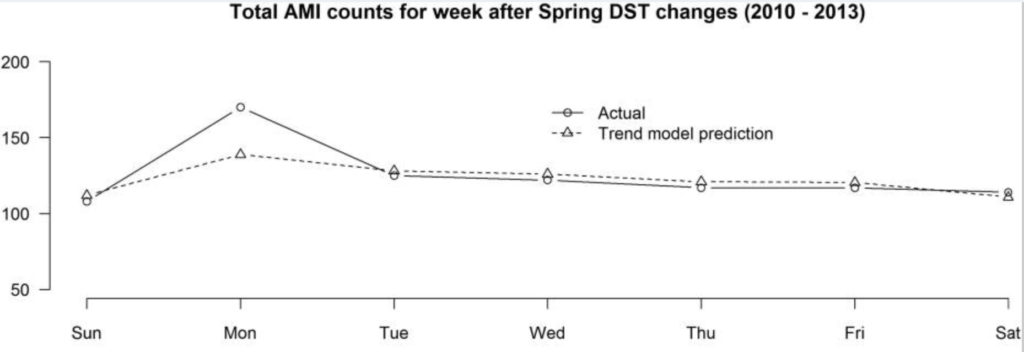
- 24% increased risk of heart attack day after daylight savings in spring
- And in Fall, there’s a 21% reduction
Figure 1. Actual and predicted acute myocardial infarction (AMI) counts for the week after the spring daylight savings time (DST) time changes. Source: (Sandhu et al., 2014)
⇒ Other examples involving daylight savings:
- Increase in car accidents
- Increase in suicide attempts
- And Federal judges hand out harsher sentences on Monday after spring and are more lenient in the fall
⇒ Furthermore…
- The effect lasts for roughly 3 days
- In the northern hemisphere, you’d predict the opposite if sleep weren’t important because more sunlight. . .but despite this, the lost hour of sleep still has big effect.
Study: Short sleep duration and incident coronary artery calcification.
- Study tracked healthy adults without signs of CVD
- By the end of the study, those getting 5 hrs of sleep or less had a 200-300% increased risk of coronary artery calcification
- The study controlled for factors like exercise, smoking, BMI, snoring, etc.
⇒ What is the mechanism?
- With lack of sleep, the body becomes much more driven by the sympathetic nervous system (the fight or flight branch of the nervous system ratchets up)
- This means more adrenaline release, high spike in cortisol levels, and blunting of growth hormone (all factors leading to atherosclerosis)
Other disease pathways affected by sleep deprivation
- Lack of sleep increases blood pressure (hypertension)
- Having an ApoE4 gene is a risk factor for Alzheimer’s, but one study showed that if you are normotensive (normal blood pressure), you don’t necessarily have an increased risk of Alzheimer’s disease, but if you are hypertensive, then your Alzheimer’s disease risk is far higher
- It’s like revving an engine in neutral; eventually the gaskets will blow
“If there is one central, common pathway through which we can understand almost all aspects of the deleterious impact of insufficient sleep, it is through the autonomic nervous system, and specifically an excessive leaning on the fight or flight branch of the nervous system.”
Matthew Walker Ph.D.
Dr. Walker earned his degree in neuroscience from Nottingham University, UK, and his PhD in neurophysiology from the Medical Research Council, London, UK. He subsequently became a Professor of Psychiatry at Harvard Medical School, USA. Currently, he is Professor of Neuroscience and Psychology at the University of California, Berkeley, USA. He is also the founder and director of the Center for Human Sleep Science.
Dr. Walker’s research examines the impact of sleep on human health and disease. He has received numerous funding awards from the National Science Foundation and the National Institutes of Health, and is a Kavli Fellow of the National Academy of Sciences.
Dr. Walker is the author of the International Bestseller, Why We Sleep. It has a singular goal: to reunite humanity with sleep.
In addition, Dr. Walker is an internationally recognized speaker, a successful entrepreneur, and a Sleep Scientist for Google.
[sleepdiplomat.com]
Twitter: @sleepdiplomat
Center for Human Sleep Science: https://www.humansleepscience.com/
Matthew’s publications: https://www.humansleepscience.com/p-u-b-l-i-c-a-t-i-o-n-s





I did not hear the docs review the orexin pathway and Belsomra . Did they at some point?