BJ Miller is a hospice and palliative care specialist on a quest to reframe our relationship with death. In this episode, BJ begins with how his own brush with death radically shifted his perspective and ultimately forged his path towards palliative care and helping patients integrate and understand their life in a meaningful way. BJ recounts several moving stories from his patients, which reveal important lessons about overcoming the fear of death, letting go of regret, and what’s most important in life. He discusses the major design flaws of a “death phobic” healthcare system. Furthermore, he makes the case that seeing death as a part of life allows us to live well, as opposed to living to evade death itself. He concludes with a discussion around physician-assisted death as well as his hopes around the use of psychedelics to reduce suffering in end-of-life care.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- BJ’s accident leading to the loss of his limbs and his experience inside a burn unit [3:00];
- Coping with his amputations—being tough, the grieving process, and the healing properties of tears [14:30];
- Going from art history to medical school: the value of a diverse background in medicine [28:15];
- How BJ’s new body liberated him [40:00];
- How losing his sister to suicide and his disillusionment with medicine altered his path [47:15];
- Discovering his path of palliative care—distinct from hospice—in medicine [55:30];
- Our complicated relationship with death, and how acknowledging it can release its grip and improve living [1:02:15];
- The different distinctions around the fear of death, and how BJ helps his patients negotiate fears [1:10:00];
- The major design flaws of a “death phobic” healthcare system [1:14:15];
- Common regrets, the value of time, and other insights from interactions with patients in their final moments of life [1:23:00];
- The story of Randy Sloan—a case study of playing life out [1:33:45];
- Hastening death with physician-assisted dying: Legality and considerations [1:39:45];
- The use of psychedelics in end-of-life care, and what BJ is most excited about going forward [1:45:45]; and
- More.
BJ’s accident leading to the loss of his limbs and his experience inside a burn unit [3:00]
Life-altering event
- Shortly after Thanksgiving in 1990, BJ was in college at Princeton at the time
- He was out having a drink with friends and climbed on top of a non-operating commuter train as a goof
- He got too close to the electrical line above the train the electricity entered through his metal watch on his my left arm and then ground down causing an explosion
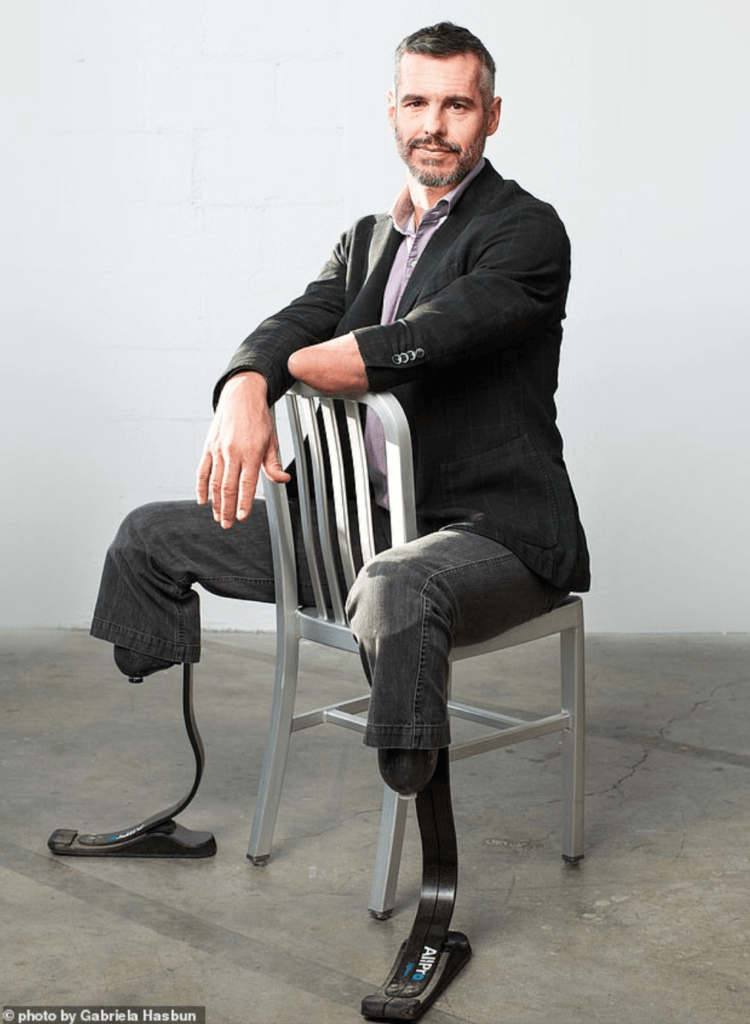
- He ended up losing both legs below the knee and his left arm below the elbow and spent months in the burn unit
- What does he remember from the night?
- Very little, doesn’t remember getting shocked
- His first memory was being awkwardly loaded onto a helicopter as the paramedics were trying to vent the heat from his body (With electrical burns, you burn from the inside out, so you’ve got all this heat running around in your system and it’ll keep burning you)
Life inside the burn unit
“It is another world that I’ve always struggled to impart to people what it’s actually like in there. It is a wholly unnatural place. I mean, nature is completely kept at bay.” —BJ Miller on the working conditions inside a burn unit
A burn unit is a very different place that requires specialized doctors and nurses
- The grotesque nature of the disfiguration of the skin
- These dressing changes several times per day on a patient require incredible sterility at the bedside
- Even the smell of burned tissue is a very foreign odor to people
Risk of infection
- Infection is very often the thing that kills people, hence all the sterility
- Someone might look just fine, but their survival odds can be quite low because their body is so susceptible to infection
- There is no touching allowed (hard for BJ and his parents)
Coping with his amputations—being tough, the grieving process, and the healing properties of tears [14:30]
Why the need to amputate limbs?
- When fasciotomies are performed initially, it’s with the hope of salvaging the limbs
- They came to the realization trying to salvage the limbs was actually going to threaten BJ’s life due to infection
The conversation with the surgeon
- One night, BJ had a memory of the conversation regarding amputation with the surgeon
- When he awoke the next morning, he was in a daze and remembers thinking, “Thank god that was just a dream.”
- In his hazy state, BJ managed to extubate himself, put out the central lines in this neck, get out of bed and start to walk to the bathroom
- About halfway there, the catheter line ran out of slack and it yanked on the Foley, “that’s a pain that I won’t soon forget.”
- At that point, clarity hit him—he knew at that point that the amputation conversation wasn’t a dream
“It was instantaneous that I realized this wasn’t a dream. And all the relief that I had experienced moments ago in the other direction just immediately went away, and I was very, very clear where I was and what was happening to me. Instantaneously. It was a wild, wild moment I won’t soon forget.” —BJ Miller
Figure 1. Photo of BJ’s new body. Image credit: dailymail.co.uk
BJ’s process of mourning the loss of his limbs
- His conscious mourning process was delayed, he thought the thing to do was to pick yourself up, be tough, and get back on the horse, “The less you acknowledge what’s gone on, the better. The tougher you are, the faster you’ll be functional again.”
- Weird level of immediate acceptance: BJ’s mom has been disabled due to polio her whole life, so in his first conversation with her was almost an excitement to be able to relate with her, “now we have so much more in common”
- It wasn’t a thorough acceptance, “It was where I wanted to be, but it wasn’t really where I was.”
- He was on autopilot in a way
First time he let it out—
{end of show notes preview}
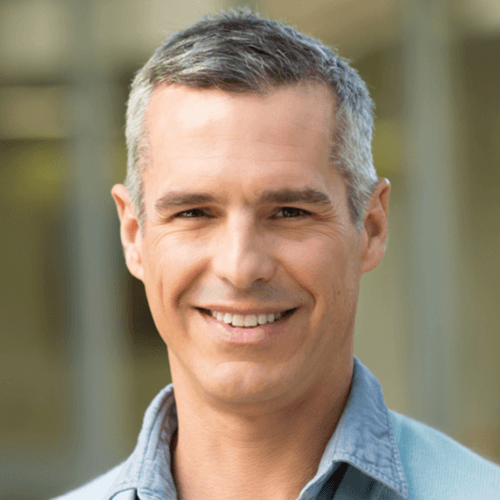
BJ Miller, M.D.
BJ Miller is an author, TED speaker, and physician. He specializes in hospice and palliative medicine treating hospitalized patients with terminal or life-altering illnesses. In his work in end-of-life care, he seeks to connect art, spirituality and medicine, and thinks deeply about how to create a dignified, graceful end of life for his patients.
BJ currently works with Mettle Health which helps those facing challenging diagnoses improve their quality of life by addressing physical, emotional, social, and spiritual needs.



This is going to be incredible! I’ll have more to say later when I’m able to give it a listen. Congrats on the move to Texas as well. You’ll have plenty of opportunities to bow hunt axis, and if you want challenging terrain thrown in the mix, look for an outfitter with land on the Devil’s River.
What a beautiful story, thank you Peter! I’m so thrilled to learn about Mettle Health too and look forward to learning more from Dr. BJ Miller directly.
“…What does quantum physics have to do with near death experiences?
It’s going to be quantum physics that discovers that consciousness survives death, that consciousness is an energy that can neither be created or destroyed. It’s consciousness that causes the collapse of the wave function. When you see something it’s because the wave becomes a particle, allowing you to actually see it as a solid. But things are not really solid, that’s the illusion. There’s a dual nature to reality and it’s this duality which explains why our bodies are separate from our actual selves, our consciousness. Our reality is determined by consciousness. It determines what we see and what we believe. Our consciousness is not just some invisible thing in our heads. We are not our brains. We are not just matter. There is more to us than just the sum of our parts. Consciousness is something akin to the airwaves of a radio station. You can destroy a radio but you haven’t destroyed the airwaves where the music is playing. …” Source: https://www.funeralwise.com/digital-dying/sex-drugs-and-quantum-physics-interview-with-a-wizard-on-near-death-experiences/
Thank you for this extraordinary conversation! Death can be so messy, yet we don’t prepare for it. Doctors often don’t acknowledge it either, waiting for it to happen somehow, or drugging the patient before he or she can even realize that the end is near. Dying without having had the chance to say goodby, or to understand what is happening, is so excruciating. I wish I had had some of this wisdom in me, and in the people around me, when my mother died. Dr DJ Miller’s humanity is remarkable. Thank you for all you do!
Beautiful episode! My thoughts are as follows- Hospice is a wonderful service when it is needed. The problem is that health care providers- in my experience- do not offer it when they could/should. In 2002, my first husband was diagnosed with colon cancer- toward the end, I had to ask for hospice- it wasn’t offered. I summoned the courage to marry again, and in 2015 my second husband also came to the end of treatment options from colon cancer- and again, I had to ask for hospice. In both instances hospice helped us with the transitions and declining health, but why did I have to ask for it?? What happens to families that are not in the health care field and don’t know the benefit or the existence of hospice? To die without that specialized care and support is a tragedy. I hope this raises awareness and gets hospice at the bedside more timely.
Thank you for another thought-provoking podcast. I almost didn’t listen to this one (for all the reasons you discussed), but I’m very glad I did.
Thanks Peter… this was one of my favorite episodes, and I’ve listened to almost all of them. BJ’s story is amazing, and I really appreciated the really eloquent way he talks about palliative care as a discipline focused on the person living with the disease, rather than on the disease itself. As a NP working in hospice (and now palliative care) for over 22 years, I’ve seen how much of a difference that distinction in the focus of care can make for patients and their families.