Note to readers: This post was written in December of 2011. PLEASE do not ask me why I eat ‘this’ or why I don’t eat ‘that’ — as what is shown here does not necessarily reflect what or how I eat today (or more importantly, how you should eat). My diet evolves constantly, due to my constant tweaking and self-experimentation. Over time, I’ll share it here and there, but what I eat is not at all the focus of this blog. I ask that you refrains for pursuing questions about what I eat in the comment section.
Once people start to “get it” with respect to why carbohydrate reduction, or all-out restriction, leads to good things, the inevitable question I’m asked is, “So….what exactly do you eat?” I’m always a bit hesitant to get into this. It’s sort of like asking a pilot, “So…how do you fly this plane?” It’s a great question, but probably the wrong first question.
For many people it’s so overwhelming to contrast what they currently eat – probably a typical American diet of 500-600 daily grams of carbohydrates (200 grams of which are sugar) – with a diet of less than 50 daily grams of carbohydrate, which is what I consume. Remember, what I’m showing you here is what I have been eating for about the last 7 months. For the first 20 months of my nutritional transformation, I was gradually reducing carbohydrate intake from about 600 daily grams to 300 daily grams to 150 daily grams.
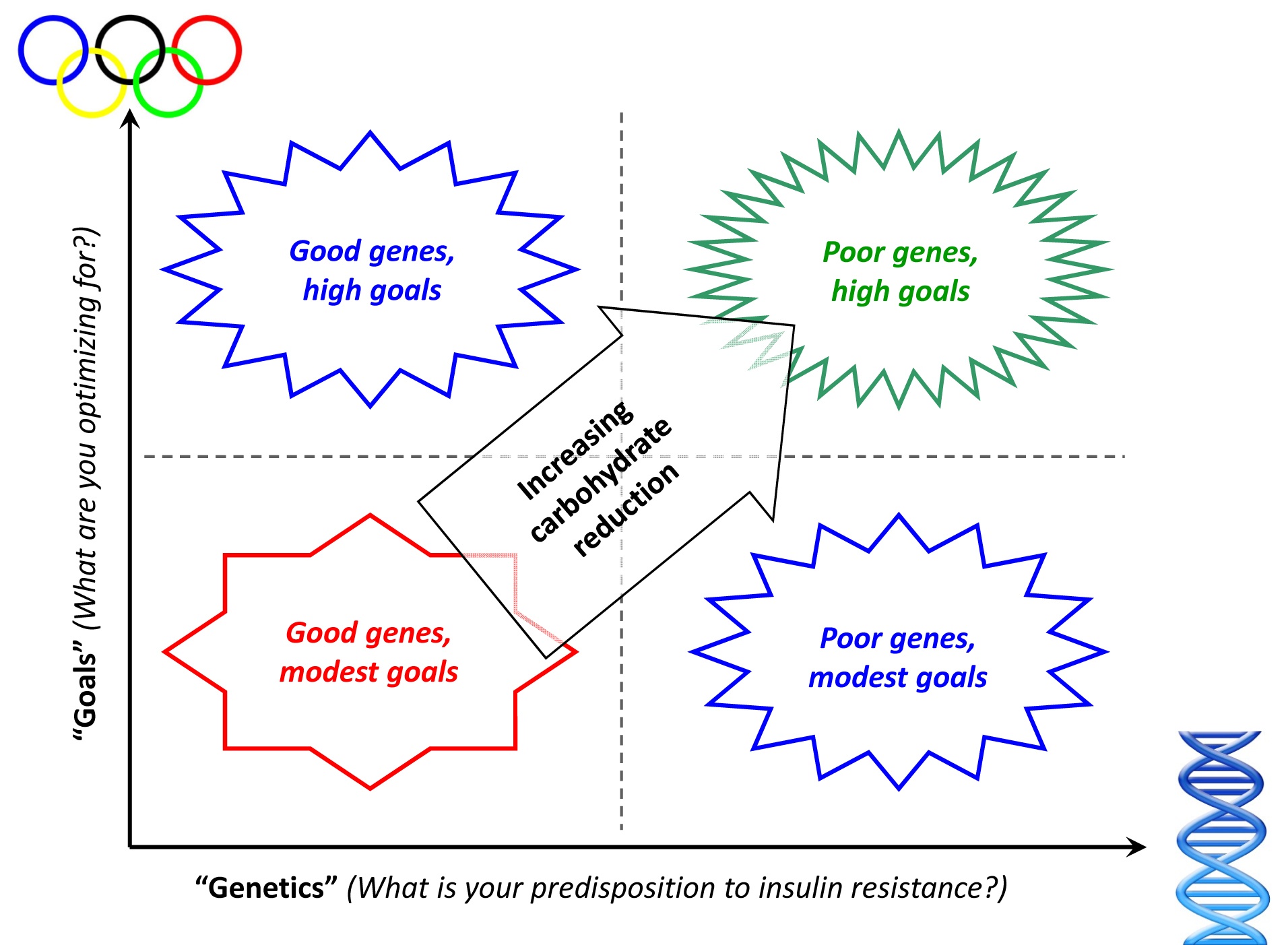
It’s really important to understand that carbohydrate reduction is a continuum. There is no “right” amount of carbohydrate to eat. Let me illustrate this with the following “2 by 2” matrix, below (sorry, once a consultant, always a consultant). When asking the question, “How much should I reduce my intake of carbohydrates?” it’s a good idea to start with two broader questions:
- What is my inherent level of insulin resistance?
- What are my goals?
There are technical ways to quantify the answer to the first question, which I will detail in future posts. However, the simple version of determining your inherent amount of insulin resistance is checking how many criteria of metabolic syndrome are present. In other words, are you overweight? Is your waist large? Is your blood pressure high? Do you have elevated blood glucose or triglycerides (these are determined from a standard blood test)? Do you have low HDL cholesterol? For the purpose of this question, even responding “yes” to one of these questions means you are predisposed to being insulin resistant. I was a “yes” to 3 of these questions.
Consider this matrix, and let’s use me as an example.
- How predisposed am I to insulin resistance? One look at a picture of me in my non-lean state, coupled with an understanding of my family history, and it’s clear I didn’t hit the genetic lottery with respect to insulin resistance. Hence, I am towards the right of graph.
- What am I optimizing for? Some folks want to lose 15 pounds. Others want to have fewer swings in daily energy level, or stop taking their blood pressure medicine. In my case, I want to maximize as many variables as possible: I want to be as lean as I can; I want to cure my insulin resistance; I want to be sure I never have a single symptom of metabolic syndrome; I want to do everything I can to avoid cancer and Alzheimer’s disease; I want to be metabolically flexible. Hence, I am towards the top of the graph.
As you can see, based on my poor genes and lofty goals, I find myself in the upper right square, which means I need to adopt the greatest amount of carbohydrate restriction. My wife, in contrast, has good genes, coupled with high goals, placing her in the upper left box. As a result of this combination, she does not need to restrict carbs as much as I do. If her goals were even more modest, she could get away with very little reduction in carbohydrates – probably just reducing sugar without much reduction in starch.
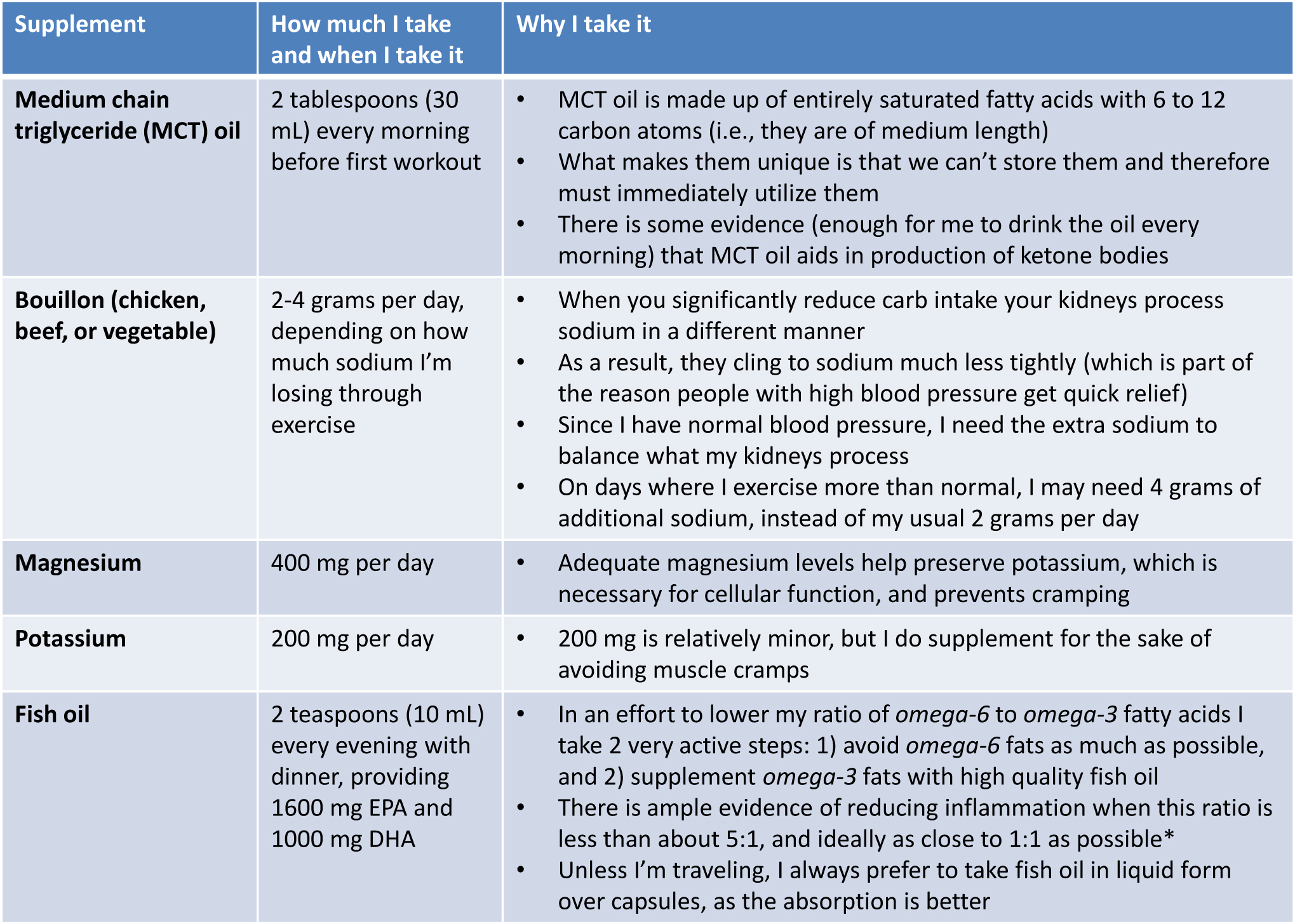
Below is a picture of a few of the foods you’ll typically find in my refrigerator. Note that on average I consume about 4,000 to 4,500 calories per day. I get this from approximately 400-425 grams of fat, 120-140 grams of protein, and 30-50 grams of carbs. In addition, there are a number of supplements I consume daily, which I describe in the table below. In future blog posts I will go into greater detail as to why I consume each of these supplements, but for now I’ll give a very quick explanation.
Finally, note that under no circumstance do I ever count calories (for the sake of limiting them). When I was first transitioning into ketosis I did need to count how much carbohydrate and protein I was consuming – anything over about 50 grams of carbs and 150 grams of protein makes it difficult to generate sufficient ketones – but I do not ever count calories for the sake of restricting them. I eat when I’m hungry. I don’t eat when I’m not hungry.
Regular supplements I consume every day
*I will be writing a great deal about the role of omega-6 and omega-3 fatty acids in our diet in subsequent posts. However, if you want a quick (albeit high-level and not overly nuanced) overview of the topic, take a look at what Dr. Andrew Weil and Livestrong have to say about it.
One last point on supplements – I do not take a multivitamin at this time, but I am looking into it a bit more closely. My concern is that 1) they may not be necessary when you remove glucose from your diet (I’ll write about why in the future), and 2) they may actually do direct harm, as a result of contaminants.
Ok, at long last, here is a list of what I ate over the past 5 days (excluding water, still and sparkling, which I consume about a gallon of each day)
Wednesday
Breakfast: “Fat shake” (In a blender: 8 oz heavy whipping cream, 8 oz sugar-free almond milk; 25 gm sugar-free hydrolyzed whey protein, 2-3 frozen strawberries)
Lunch: About 4 or 5 oz of assorted cheese (Gouda, Swiss, Manchego), 2 or 3 oz olives, about 4 oz of particularly fat salami and pepperoni
Late afternoon: About 2 oz of mixed nuts (almonds, walnuts, peanuts), large latte (latte made with heavy fat cream instead of milk) at Peet’s
Dinner: Garden salad with olive oil (lots of extra oil) and balsamic vinegar dressing, about 6 oz grilled salmon with a lot of butter and lemon juice
Thursday
Breakfast: Scrambled eggs (6 yolks, 3 whites**, with added heavy fat cream) cooked in coconut oil, 3 or 4 sausage patties (be sure to look for brands not cured in sugar).
Coffee with homemade whip cream (heavy fat cream hand whipped)
Lunch: Half chicken (thigh, breast, wings) with lots of skin; about 2 oz of Gouda and aged-cheddar
Dinner: Wedge blue cheese salad with bacon; 12 oz prime rib with lots of butter; 5 or 6 pieces of asparagus coated in butter
Coffee with half and half cream, 2 cups (the restaurant did not have heavy cream, so I had to settle for half-and-half)
**The reason I typically minimize egg whites, at least when making my own eggs, is to ensure I keep protein intake under about 125 grams per day. Ketosis is pretty easy to attain if one is eating, say, 2500 calories per day. However, given my caloric demands – and the requirement that I keep protein intake limited – I really need to go out of my way to ensure I’m not eating too much protein. I will be writing about this in much greater detail in a future post.
Friday
Breakfast: Whole fat latte at Starbucks (made same as above), scrambled eggs (about 4 eggs), bacon (high fat pieces), slice of Swiss and slice of cheddar (since I was eating in the airport, the scrambled eggs were made “normally,” not with the additional fat I use when making my own)
Lunch: About 4 oz of especially fat salami and pepperoni, about 2 oz Parmesan cheese
Dinner: Ground beef sautéed with heavy cream, onions, broccoli, and melted cheese
2 large cups of decaf coffee with homemade whip cream (heavy cream whipped with a touch of xylitol)
Saturday
Breakfast: Scrambled eggs (6 yolks, 3 whites, with added heavy fat cream) cooked in coconut oil, 3 or 4 pieces of especially fat bacon (not cured in sugar), about 3 oz of cream cheese
2 cups of coffee with heavy cream
Lunch: Tomatoes with basil and mozzarella and balsamic vinegar and olive oil, about 2 oz raspberries with homemade whip cream
Dinner: Leftover ground beef sautéed from previous night, salad with homemade cream dressing (whole fat Greek yogurt, olive oil, basil, blue cheese, garlic)
1 cup of decaf coffee with homemade whip cream
Sunday
Breakfast: Omelet (6 yolks, 3 whites, coconut milk, sautéed onions) cooked in coconut oil, 4 or 5 pieces of the fattest bacon I can find
2 cups of coffee with heavy cream
Lunch: Plate of assorted cheeses (aged Gouda, Swiss loaf, aged Parmesan – about 3 oz), about 2 oz salami, about 1 oz olives
Dinner: Cream of mushroom bacon soup (heavy cream, chicken broth, shredded Parmesan cheese, mushrooms, chopped bacon, garlic, butter, chopped papers, various spices), leg of lamb (baked in sauce made of red wine, balsamic vinegar, diced tomatoes, garlic, and a lot of spices)
2 cups decaf coffee with homemade whip cream (as above)
So there you have it — 5 days in the eating life of Peter Attia. This may look a bit strange, relative to what you may be eating now, but remember, I’m at the far end of the spectrum – i.e., nutritional ketosis. You may just be starting your own journey of reducing carbohydrates, but I hope this gives you an idea of what I eat. In particular, what probably stands out is:
- I go to great lengths to avoid sugar which, unfortunately, shows up in virtually every highly processed food.
- I eat zero starch (e.g., bread, cereal, rice, crackers, pasta).
- I consume only modest amounts of fruit (one serving per day, at most, and only in the form of berries, which contain the least amount of fructose).
- I eat vegetables, but primarily because they are a great way to get more fat (e.g., high-fat salad dressings, butter), not because I “need” them.
- I go out of my way to eat as much fat as possible, especially monounsaturated and saturated fat (the only fat I avoid is omega-6 polyunsaturated fat).
- I have a few “go to” meals that I eat several times per week. I do this because I really like them and it’s quick and easy make them. Yours need not be the same!
Photo by Glen Carrie on Unsplash





Can you talk a little about why you count total carbs vs. net/effective carbs?
It’s a “higher bar” and it’s quicker and easier. For example, it’s pretty easy for me to calculated 40 gm of total carbs per day and know that I’m getting even fewer net carbs.
Ok, that makes sense. Just wanted to make sure there wasn’t something I was missing from a scientific perspective (new research). I’m ok with the lower bar (~20-30) and checking labels to do the calculation to avoid accumulating too many net carbs.
“Higher bar”… I love this way of thinking about net carbs
Hello Peter,
Great website! I stumbled upon this via one of my random checks of Gary Taubes’ site. Have you come across any research regarding the cooking of meat and related cancer risks? Also, you mentioned that you typically eat salami and pepperoni. Any concerns regarding nitrates and cancer?
Thank you,
Chris
Thanks very much for support, Chris. The biggest risk (think of the irisin post from 1/25) is the first order stuff – sugar in the meet that actually leads to the AGE’s. This is where I spend a few extra dollars to get higher quality products, rather the pre-packaged variants. That said, I think you’re better off with pre-packaged pepperoni than, say, fresh corn and potatoes.
Hi, I’ve been reading through the site and I might be missing it, but am very interested in doing this kind of “program”, so do you have it published? I read the 5 day sample week. what happens on the 6 and 7 day? is there a “free” day where you can eat what you want (including more carbs?)
Thanks,
Sinai
Sinai, there is no “program” here. The blog is really my vehicle for trying to help people understand the science of health and nutrition better. I am in the process of putting together a separate entity that will be focused on the “program” side of things, but it won’t be part of the blog. I’ll address all of these issues and more. Thanks for your interest and please stay tuned. Hopefully there is enough content on this blog to help you get started, though. If you haven’t read it check out the page: How can I lose weight?
Great info and website! I too was directed here from Gary Taubes blog. I’m really interested in the high amount of calories you consumed even while losing weight. It really happened for you even without being in a caloric deficit? Or were you just extremely active and therefore in a deficit even while eating 4000+ calories a day? I always understood that low insulin levels helped with satiety but one still needed to be in a deficit to lose weight…but not the case here right?
Suzi, by definition I was in a calorie deficit if I lost weight (take a look at the post titled “Revisit the causality of obesity”), for the First Law of Thermodynamics to be true (which it always is). This meant that despite eating 4,500 calories or so each day I was expending more – not by exercising more or doing more daily activity (which I didn’t do) – but through a greater basal metabolic rate and probably a greater amount of digestion expenditure. Because my insulin levels were reduced, my body made these changes.
I think there’s a fundamental misapprehension here about the First Law of Thermodynamics and human bodies. Just *eating* a “calorie” (whatever that means) doesn’t mean it will be burned–as any lactose-intolerant person knows. In order to invoke the First Law, you have to demonstrate that the calories you ate were actually burned, not just excreted.
Not so. First Law only states that energy in less energy out is equal to change. Lots of ways energy can leave a system, including thermogenesis and failure to digest (e.g., excretion in stool). Look at post “Do Calories Matter” for a more detailed description.
There is no evidence about metabolic advantage while in ketosis. Au contraire:
https://www.bodyrecomposition.com/research-review/ketogenic-low-carbohydrate-diets-have-no-metabolic-advantage-over-nonketogenic-low-carbohydrate-diets-research-review.html
Hi Caveman, thanks for passing this link along. I’m assuming you’ve read the actual study, and not just the commentary on the study that you sent. I’ve read this study several times, actually, as it was originally published in 2006. If you haven’t done so, it’s probably worth reading it – it’s only 7 pages. LOTS to say about it, but not enough time right now. I did want to respond, though. Here are a few things to consider when looking at something like this: be clear you define metabolic advantage inclusively. This study looked at some good things (e.g., HOMA-IR, via fasting insulin and glucose), but many completely useless things (e.g., LDL-C, TC-C). Also, we have no idea exactly how the study designers balanced out things like omega-6 and omega-3 ratios. As I’ll be writing about a great deal, after reducing insulin levels, in my opinion, this is probably next on the list to “get right.” Almost certainly, given the delta in PUFA consumption, this was the cause of ALA:EPA:DHA:AA levels. Next, it’s not clear at all that the ketogenic group was receiving the ideal supplementation of sodium, magnesium, and potassium, which is the cause of “feeling bad.”
However, undoubtedly the biggest criticism I have have this paper is that the “ketotic” group was not really ketotic! If you look at table 3 of the actual paper (not the summary in link you sent), you’ll note that the level of beta-hydroxybutyrate in the low carb group went from 0.1 to 0.2 to 0.2 mM, while the ketotic group went from 0.09 to 0.72 to 0.33 mM. One does not even begin to generate the advantages of ketosis below 0.5 mM, and probably close to 1.0. In other words having a ketone level of 0.33 is the most miserable thing on earth. Why? Because you’re clearly restricting glucose (so your brain is agitated), but you’re not generating enough ketones to fuel your brain. Trust me, I was in the zone of misery for weeks. If you read the work of people who have the most experience treating patients with ketotic diets (e.g., children with intractable seizures, recalcitrant diabetics), they usually keep beta-hydroxybutyrate above 1.0. I check my blood levels every day (and have logged them for nearly 8 months). Anything below about 0.6 feels horrible, and I generally walk around between 1.2 to 2.0 mM. So, I guess my issue with this article is that it didn’t actually do what it set out to do – test a ketotic diet.
If you really want to get nuanced, you’ll probably note the conflict of interest, also (note the last author on the paper). Hope this helps. Keep in mind, if you’re out there doing your thing and feeling great – that’s awesome. I’m happy for you. Keep it up and please don’t think I’m trying to change you. However, I do feel strongly that people really understand what they are saying. The majority of published studies are not worth the paper they are printed on, so we need to be diligent when we look at them. Finally, if I’m coming across as a bit glib, I don’t mean to, but when someone phrases a question as you have, they won’t get my “gentlest” response. Ask nice, and I’ll answer nice. Ask like a wise-guy, and I may sound a bit glib. Fair?
I’m also low carb/keto athlete like you but not an expert for ketosis. I wanted to hear your opinion about this because you said your bmr is much higher while in ketosis. But how can you be sure ketosis is the cause for this?
I posted this link because this is the only keto vs non keto study i know about and it doesnt show any bmr increase.
If i understood correctly, keto group wasnt keto adapted enough?
Caveman, it’s a fair question you’re asking. Yes, you’re correct, the “keto group” was not actually keto. The fact that they went from 0.7 mM at week 2 to 0.3 mM at week 6 says they did not eat the right foods to stay in ketosis. They flirted with it briefly, but ultimately ended up eating too many carbs or too much protein to actually generate sufficient ketones.
Let me rephrase your question to be sure I’m answering it. You’re really saying, “How do you know that the increase you experienced in BMR going from 150 gm/day of carbs (i.e., Low carb) to <50 gm/day (i.e., ketosis) was accounted for by the actual presence of ketones in your body?" Assuming this is your question, it's a great one. There is no dispute my BMR increased dramatically during this period, as I lost 4 pounds of fat in 12 weeks while increasing my caloric intake from about 3100 calories per day to 4400 calories per day. Little change in my exercise (except that I stopped doing heavy squats, deadlifts, tire flips and cleans - which probably accounts for the loss of 3 pounds in lean mass). But the question is what drove this change in my metabolism? At the simplest level we can point to at least 3 "changes" - 1. I ate fewer carbs (150 down to 50 gm/day), 2. I ate more fat (about 150 up to 400 gm/day), 3. My body produced high amounts of ketones (I was 0 to 0.1 mM of beta-hydroxybutyrate at the outset, and greater than 1.0 once ketotic). To my knowledge no one has done the experiment you would need to do to figure out if it's the rise in beta-hydroxybutyrate OR the fall in carbs (and insulin) that effects the change. Or the rise in fat intake for that matter. These 3 are heavily related and therefore not what we'd call independent variables. My guess would be the actual presence of ketones bodies are not what's CAUSING the effect, but are merely a byproduct of the effect. The CAUSE, I would hypothesize, is the reducing in circulating insulin from fewer carbs ingested. Hope this helps.
I have a question about ordering the whole fat latte’s at Peets and Starbucks. Do they charge more for it? And do you just say ‘latte with full fat cream please?” And do they look at you funny? 🙂
I ask them to make a latte as they normally would, but instead of using milk, to use whipping cream (aka 35% cream or whole fat cream). I always watch when they make it to be sure I can see the cream they are using, since they probably don’t make it often (or ever). They charge me the same. They look at me VERY funny. In fact, once I had 2 in one day from the same Starbucks and when I ordered the second everyone in the shop came up to see what I looked like because they’d heard about it from the morning shift. You gotta eat fat to lose fat!
I recently stumbled upon one of your lectures on YouTube and I am already a huge fan.
I’m curious as to how our bodies handle carbs in the post-workout phase. More specifically, I eat essentially no carbs during the day (except broccoli, spinach, etc.) but immediately after a strength training workout I will have a bowl of oatmeal with protein powder. My thinking was that in the post-workout phase the carbs would be preferentially stored as muscle glycogen, but I don’t know if the biochemistry backs that up. Furthermore I don’t know if these carbs might inhibit my ketosis.
Any insights you have would be great!
Scott, thanks for the support. I will write a lot about sport-specific implications in the future, but let me try to give a quick though. It is true that if you’re going to eat carbs, the best time to do it is when you’re immediately post a workout when your glycogen stores are depleted. The will ensure, in a reasonably insulin sensitive person (which I’m assuming you are), that your metabolic preference is in glycogen formation FIRST. Keep in mind the size of your glycogen “tank,” though. If you overdo it, you will start to divert the excess into fat storage. It’s pretty hard to be in ketosis with a bowl of oatmeal and other carbs in your diet. The only way to really know would be to test yourself. When I was starting out, I would do 5 or 6 blood tests per day, while varying all sorts of conditions (e.g., exercise, food intake).
the reasons you posted at the end is similar to my approach and thinking; this is real exciting.
Fantastic and interesting blog,
discovered via Gary Taube’s site, reading on Dr Oz.
I live in the UK, 2 years ago my GP told me I should be put on statins as my cholesterol is high -7.2, higher than in my last test. He gave me a year to improve it, as I did not want take them – 40 and on statins hello? I eat all my greens, no junk, cigarettes, alcohol, no or little simple sugars, no processed food, I go to the gym 3 times a week and lift weights, cycle 60 – 80 km a week, walk 30 km at the weekend, how the frack do I have a cholesterol higher than my dad? My friends joke that I should be thinner with the boring food I eat, I am 80 kg and a US size 12, my skeletal muscle mass might be strong, but my visceral fat is far too high. I should be 72 kg ( if only).
My GP volunteered me to be a guinea pig for a new cholesterol-lowering -drug (I agree for the free health check) after being poked and prodded ( do you know how hard it is to give up coffee as a French person, torture), I was rejected for being too healthy. After reading Dr Annika Dahlqvists, I realised I did not have enough fat in my diet and I decided to ingest 2 table spoons of raw coconut oil a day (not easy), with 1mg of vitamin C and B complex. My HDL is gone up from 1.42 to 1.75, my GP told me , “ok you are one of these people who have a high cholesterol no matter what, go away”.
I have been overweight since puberty, in my twenties, despite being physically active, I reached the boundary obesity-corner of the charts. I went on diets, lost the the weight and gained it back and some more. In my late twenties, I developed ailments that baffled my GP and after a ruptured ovarian cyst that landed me in hospital, I was diagnosed with PCOS. I was put on the pill and on a strict low fat diet. Within 6 months on the pill (after a welcome relief from symptoms) I felt like a Stepford wife, worse, on the high carb diet I had gained weight, reaching 95 kg for 5.8, putting on 5kg. When I put my concerns to my GP, a woman, she told me that my yo-yo dieting was responsible for my PCOS and that I was obviously cheating on my diet. Something clicked in me and I thought – FU, this is not all on me -. I did some research and stumbled on insulin resistance and found that my symptoms matched, I was alway sweating and hungry for sugar after a meal. I quit my GP, the pill and the high-carb low-fat diet.
I went on the Atkins diet and lost 15 kg in a year, and worked that if I wanted to keep it off, I had to modify my diet, no simple sugars, no junk, no processed foods, bread, pasta, (for the odd croissant at weekends), Lepicol with digestive enzymes, greens (I like them) and good fats. The endocrinologist that follows me, declared me PCOS free, but with a estrogen dominance. I take after my dad, on his side of the family it’s cardiovascular disease (strong men, who gain weight, never get sick but die of a heart attack after 50 – the women, maybe protected by estrogen, get sick later but are always fat ), my mother is thin and lives on sugar without gaining weight but on her side, liver, stomach and digestive track cancers dominate.
My problem is that no matter how much I exercise, my fat % does not go down below 33%.
Even on complex carbs, some protein and vegetables, weight creeps up. If I did not go to the gym, I would be even bigger than I am now. I need to give up carbs again. I train with a lean guy whose body fat is at 10% and lives on pasta, and I swear I have bigger calf muscles than he does.
I can’t live on the Atkins or Dukan ( too much meat brings digestive problems) for long and I am lactose intolerant since birth, so after 2 weeks of yogurts, ( my limit is 125g a day) fromage frais or full fat cream, even if it’s from goats, my sinuses pack-up and scream – enough is enough woman. If my brain goes foggy by late afternoon, I have never felt mentally – stronger than on the low carb diet but what can I use instead of full fat milk and cheese? Nuts?
Dominique, thanks so much for sharing your story and your struggle. The tough part of “this” nutrition thing is that we are all quite different in terms of our genetic susceptibility to carbohydrates, and even within the world of carbs, we all respond different to the different variants. As far as the statins go, this is one of the biggest tragedies in modern medicine (next to the nutrition problem). The problem is not that statins are bad or that some people aren’t dramatically helped by them – the problem is that 99% of doctors who prescribe them do so for the wrong reason. They treat the wrong endpoint (e.g., LDL-C instead of LDL-P or ApoB) AND fail to realize how many people don’t actually need them. Obviously, I can’t tell if you should or shouldn’t be on them, but I will write more about this in the future, so hopefully you’ll get a better sense of the questions to ask your doctor.
What you’ve got to figure out is, what do you want to optimize for? How much are you willing to experiment with the boundary conditions? I can’t really address it here, but I’ll give you an example. My entire life I believed I was lactose intolerant. As I contemplated the transition to ketosis I was a bit concerned about the need to increase dairy. To my surprise, by increasing dairy dramatically and reducing fruit intake, my supposed lactose intolerance vanished within days. In other words, I was intolerant to the 6 servings of fruit per day, not the lactose. I’m not saying this will be your experience, but the more you experiment – and measure outcomes correctly – the more you’ll find your sweet spot. Best of luck as you continue your journey.
Thank you for your response.
I will experiment – I already don’t eat fruit – and will “measure outcomes correctly”.
Sorry, I take 1000 mg of vitamin C, not 1mg, I definitely need to measure correctly !
Also, I like to clarify, in the UK, the acceptable ratio TC/HDL ratio is 4.5 (mine is 4.9) and is viewed as one key element of your cardiovascular risk. Your age, weight, physical activity, blood pressure, blood sugar, family history, smoking habits are all taken into account. If you have high-blood pressure, family history of heart disease, diabetes, and a TC/HDL > 4.5, you are deemed high risk, then it’s statins for you, no ifs or buts. We don’t get LDL-C or P on our charts, most of us take a while to understand our results anyway.
Here the obesity levels are rising and the National Health service is concerned about the costs and also the impact of obesity related illness like diabetes 2, heart disease and some cancers will have long term. A cholesterol test is offered to you when you reach 40 and statins are seen as a preventive cure.The campaigns are to eat healthy and limit fat and sugar, yet sugar laden food is cheap and cheerful, and in every processed food it seems. Plus we are in a recession, cupcakes are thriving, vibrant food-colourings, sugar and fat give you a high on the cheap.
If I told my GP, I am eating fat to lose weight, he would re-open Bedlam just for me.
Thanks for this site.
Dominique, unfortunately, the ratio of TC/HDL is of little value. When viewing a standard cholesterol panel, the only ratio of value is TG/HDL (but you need to convert to US units). This ratio should be at or below 1.0. I will be writing much more about this in the future.
Hi Dominique,
When you say, “I can’t live on the Atkins or Dukan ( too much meat brings digestive problems) for long,” Do you mean high fat meat or high protein meat? Have some chicken thighs with skin still on them. Avoid turkey breast. Egg yolks are high fat, fatty bacon is high fat, Avocados are high fat. None of these things are dairy.
If you do indeed like greens, drown them in olive oil and put some avocados on top. If your greens are broccoli, cover them with Hollandaise. I believe butter contains no or little lactose and almost certainly clarified butter contains no lactose.
Try checking out Adam Zickerman’s power of 10 slow motion fitness revolution for your weight training. It isn’t really necessary to go to the gym three times a week. Peter is a bit of an exercise nut, so your don’t have to start tossing tractor tires around to lose weight. 🙂
Fascinating stuff. I believe you’ve just acquired another whole cadre of fans from the Atkins website, clued in by some followers of Gary’s. Two questions:
1. Can a regular non-doctor shmoe check their own beta-hydroxybutyrate, & if so how?
2. I’m especially interested in your conclusion #4 at the end of your original post:
I’m sure you know Colette Heimowitz, “our” nutritionist over at Atkins. Here’s what she says, and we endlessly repeat, about veggies:
•Why Are Vegetables Important?
o https://boards.atkins.com/showthread….Help!!!!/page8
o From Colette: Now here is my thesis on why veggies are important;
It is true that protein and fats are “essential nutrients” and carbohydrates are not. However, I consider the nutrients in colorful vegetables extremely important living in the toxic environment we are exposed to on a daily basis.
Could you please comment, in view of your conclusion #4? We’re interested to hear your input. Thanks!
Thanks for your comments and questions. And thanks for your interest in this blog. To your first question, yes, anyone can check (should they choose to) the level of beta-hydroxybutyrate in their blood using a very simple point-of-care device similar to the type one would use to check blood glucose levels. On my page “Books and tools” I provide a link to the Abbott meter I use to check both beta-hydroxybutyrate and glucose levels daily. Urine strips measure a different ketone body, and do so qualitatively, rather than quantitatively, which is why I prefer the blood test. Plus, my daughter is fascinated by the fact that her daddy pokes himself in the finger every morning and gives himself a boo-boo.
Ok, your next points/questions are excellent, but too long for me to address in this response. I will be addressing them in future posts. I do still stand by my conclusion that the only reason for me to eat veggies it to get more fat (rather than due to some physiologic “need” for them). The “science” of our need for fiber is based on very poor observational epidemiology, courtesy Denis Burkitt, which has been refuted by a number of studies between 1994 and 2000. I’ve written a post about this, and will publish it in the next month or so. Hopefully it will address your concern about fiber (or the lack thereof).
As far as the other points, I think it’s important to really scrutinize the studies that point to these benefits. These studies are not designed to, and therefore are not really capable of, actually elucidating cause and effect. Just like studies like the China Study that “tell us” meat is bad and plants are good, they can’t separate and isolate the variables on the “cause” and “effect” side. I have also written a post about this entire topic and will try to get it out soon also. So much to write about…
I’m not sure I understand your point of omega-6 and omega-3 ratios, as it pertains to eating vegetables, but I wholeheartedly agree with what I think you’re saying: we should do everything we can to avoid omega-6 PUFA and go out of our way to consume high quality sources of omega-3 PUFA. The ratio of omega-6 to omega-3 PUFA is probably quite indicative of our body’s inflammatory state. I believe I discussed in this in one of my videos.
Please stay tuned for future posts on many of the topics you’ve raised and thanks for your interest.
I appreciate your insights into Protein with respect to a low carb lifestyle. I know historically I have not been mindful with tracking that. I will certainly look to transition to lower protein levels moving forward to see how it works for me.
I do have a question. When buying meat that is still on the bone. Is there a rule of thumb or easy way to to calculate the nutritional values? It would seem that all the data I have seen takes the serving size weight with no bone. This is most frustrating for me with chicken wings that I’ll often prepare on the weekends.
This level of precision was only really necessary during my (very difficult) transition into ketosis when my usual eating habits (>250 gm/day of protein) were causing problems. After preparing a few meals with surgical precision, you’ll be able to eye-ball it. Remember, this level of precision was only necessary for ketotis. You do not NEED to do this to make better food choices.
Your comment about “levels of precision” for ketosis is exactly why I am writing. I lost 11 pounds the first week, following you menu. However, this week, I went up 4 pounds, due to, in my opinion, an increase in my meat consumption. Obviously, I will lower it greatly, but as I reviewed your menu, I noticed you wrote in one place about limiting protein to only 125 grams (4.4 ounces) per day, yet one day you ate a 12-oz prime rib, and another day, 6 oz grilled salmon.
I ask not to argue (believe, your plan is working very well for me… and I am happy), but for me to remain in ketosis, is it partly trial-and-error, or is the 125 grams protein a number of particular significance?
Again, bottom line, I am (as of today) taking in waaaaaaaay less protein to get back into ketosis.
Mark, I wish, I *really* wish, I could answer these questions with precision. I can’t. It’s much more “art” than “science” at the individual level. Yes, my protein intake varies from day to day. So, too, do my ketone levels. I have observed — IN MYSELF — that when I consistently eat more than 125-150 gm/day of protein, I bump myself out of ketosis. I simply don’t have enough to data to know for certain this is the case for everyone. Individual variation is non-trivial part of this process. Above all else, I’m delighted that you understand this and are becoming a “self-experimenter,” also. Keep up the good work.
Mark, I hope Peter will correct me if I’m wrong, but I believe the 125 grams protein per day refers not to the weight of the meat itself but to the actual protein content of the meat, which is only approx 25% of the lean mass total of the meat by weight.
So, for example, that 12oz prime rib that Peter mentioned eating would only actually contain around 85 grams of actual protein (even less if it was a fatty prime rib).
Hope this makes sense!
Ahh Leoni, thanks so much for clarifying. I didn’t realize what was causing the confusion. Yes, you are correct. In fact, since I go out of my way to consume the highest fat meat possible, I generally get even less protein per oz of meat.
No problem Peter, glad I could help in some small way! 🙂
I have only just found your blog so will take this moment if I can to also say a quick but heart-felt thank you for the wonderful resource you are building here!
Not just because of the invaluable information you provide and for helping sort through many of the lingering ‘issues’ which seem to cause such heat in the LC world (and subsequent angst for many of us trying to wade through it all), but also for how you relate it, with warmth and graciousness and regard for your readers. Thank you most of all for that.
Thanks so much for your support and kind words.
This is the best low carb blog yet! I found you through Gary Taubes’s latest post (of course) and now have you bookmarked. The simplicity of your explanations is so refreshing, and you handle the inevitable conflicts of cyber interaction well.
My story is testimony to the diet you recommend. I’m a 53-year-old female, post menopausal as you might guess. 16 months ago I reduced my carb consumption to <50 grams per day and lost 20 pounds within 2 months. I'm not where I want to be in terms of muscle mass and body composition, but I love how I look and feel. I sleep better; I don't get horrible dry skin in the wintertime, my mood is calmer, and I don't get the horrible hunger pangs that used to dog me when my insulin was out of control on my old diet of 150 grams of carb and 70 grams of sugar per day (and that was low compared to the average American – good grief!). I do take .05mg per day of bioidentical estrogen in topical form.
OK, not a big problem, but it's bugging me anyway. After 16 months of low carbing, my total cholesterol nearly doubled. Here are my old, then new numbers:
Total C: 140, 255
Trigs: 52, 54
HDL: 56, 76
LDL Friedewald: 74, 168
My doc, bless his heart, focused on the HDL and trigs and told me not to worry, but he'd like to see the other two numbers come down and told me to "eat less butter and cream." Heh, over my dead body! But isn't the Total C a serum measurement of all circulating cholesterols? That means there's something other than HDL and triglycerides circulating around in there, and I'd like to know what it is and why it nearly doubled after I improved my diet. Not asking for medical advice, just help with understanding why my lipid numbers are so often typical of people who shift to this diet and whether we should be concerned. Thank you!
Hi Lacie, thanks for sharing your experience and thanks for the kind words of support. I’m glad you doctor is focusing on the only valuable information generated by this test (indirectly): TG/HDL. You went from VERY GOOD (52/56 < 1), to EXCEPTIONAL (54/76 << 1). Unfortunately, the LDL-C and TC-C numbers don't tell us anything. Please ask your doctor to check LDL-P and ApoB. Without these numbers one can't be sure of your LDL risk. I'll write about this a lot more in the future, but I recommend you check out the work of Tom Dayspring, MD. My mentor on the lipid side.
Hi Peter,
Thank you for writing this and all of your other articles. I happened on your blog yesterday afternoon and was going through each of your articles, one by one. What a mass of information and knowledge I have gained. I love that you’re so methodical leaving almost no stone unturned and that you experiment with things and document outcomes so you can share with all of us.
I feel like I’ve read a book and you’ve kept me engrossed from the first moment. I’ve been following a LCD since July last year. I seem to have plateaued (in weight loss) and was looking at doing a ketogenic diet but had no idea how to eat 80% (or thereabouts) of my calories from fat! This particular post gives me some great tips. However, I don’t have diary either so I may look at using Coconut milk/cream instead.
What you don’t seem to explain anywhere is:
1.How do you know you’re in ketosis (I know there are Ketosticks etc. but is there something more reliable)
2.I was under the impression that once you’re in ketosis and your body acclimatizes to burning fat for energy you won’t see any ketone bodies in urine.
So I’ve love to know how you know (or test) that you’ve been in ketosis for 7 months.
You don’t mention any issues with being regular (bowel movements) since being on LCD. I’ve curious if you have trouble and if so what you did. Also, I don’t see much fiber in your diet, does fat help here or do you take probiotics?
Your results are very exciting and inspiring and the information you have presented is a gold mine. Thank you!
Hi Shiv, glad you’re enjoying this information. I’ve never used urine ketone strips and only use whole blood analysis via my point-of-care ketone meter that measures beta-hydroxybutyrate (see my section on books & tools). Using this, it’s been very easy for me to document my exact degree of ketosis since I started. As far as bowel habits go, mine have improved so much since becoming ketotic, I kick myself for all of those years of suffering with bloating, gas, and other misery. Turns out fructose and gluten are 2 of the most harmful substances for your bowel. The key to healthy bowel habits is actually including sufficient sodium and fat in your diet. If you think you’re still having trouble, consider adding a bit of mineral oil or medium chain triglyceride oil. Keep up the great work!
Hi Peter. Thanks for all this very interesting information. I’m particularly interested in more info on why eating too much protein was making you feel so lousy. I understand it was keeping you out of ketosis with protein being converted to glucose, and that this was preventing you from reaching your goal. But why was it making you feel bad, and why did reducing protein further to stay in ketosis help you feel better?
The reason so much protein, in this case, was making me feel lousy was that protein – in and of itself – stimulates insulin release. With too much protein, despite “low” enough carb intake, I was prevented from generating sufficient ketones to supply my brain. But I was too low in glucose, also. So I was in what I refer to as the “zone of misery” — a place where you have too few carbs to feed your brain, but too many carbs (plus/minus protein, and in my case too much protein) to allow sufficient ketone formation.
Makes sense! Thanks so much!
peter,
I’ve never understood how some elite athletes (by elite i mean professional) especially cyclist could perform on a vegetarian diet, what are your thoughts?
I think it is possible, especially because most people in this capacity are very mindful of what they are eating. If you think about it, they are probably going out of their way to avoid not just meat (obviously), but sugar and highly refined “junk” food. If they work with a great nutritionist to ensure a good balance of amino acids (made easier if they still consume eggs and dairy), I think it’s doable. Not for everyone, but I think it can be done.
Peter, during especially hard training blocks i will get the midnight sweats (neogenesis) have you experienced this, has your new diet affected it?
Jeff, I have not experienced night sweats except as when “sick,” even during the most profoundly stressful periods of my training.
Hi Peter,
Thanks for answering my earlier questions. I have a few more…
It is known that Omega-3 fatty acids reduce TGs in blood (The Fish Oil and Triglycerides Study by Dr. Christopher Gardner from Stanford). So my question to you is, at what point did you start supplementing with Fish Oil.
Do you attribute some portion of your weight loss to exercise, or only change in body composition?
Looking at the graph in your “How I lost weight” post, your lean body mass changed by a pound over the entire period (granted a pound of muscle is quite a bit), but how do you feel about that? Further Doug McDuff (Body by Science fame) says you only need 12 minutes a day. Mark Sission (Mark’s Daily Apple) seems to be of a similar opinion. You obviously seem to disagree? Why?
Dairy (Casien) I believe (after all the research I’ve done online) has similar effects to Gluten. Again, you don’t seem to concur. What are your reasons for continuing on with dairy?
What are your thoughts on fermented foods (Kombucha, Kefir, Sauerkraut, Kimchi etc.) as related to gut flora and gut/immune system health?
Shiv, quickly: I consume omega-3 not because of the TG-reducing properties (which I think are small), but because of the counterbalance to omega-6; I don’t “disagree” with folks who work out 12 minutes per day, I’m just optimizing for a different outcome (remember: 5 reasons to exercise and weight loss isn’t one of them); the research on the harm of casien is very weak, to be gentle about. I do not subscribe to it at all. If you want to really understand why this “research” is weak, read Denise Minger’s review of “Forks Over Knives.” As far as fermented foods, I do not have a view other than these effects are certainly not 1st-, 2nd-, or 3rd-order terms. Probably not worth fretting about until one fixes everything else.
Peter,
The study shows that supplementing Omega-3 Oils reduces TGs by about 25%. Your TGs dropped by about 47%. So it’s possible that it was a combined effect, no? These are questions that come to mind and thus need to be asked and answered (eventually at least), and so I ask.
So since you’ve practically fixed everything else….:)
Neuroscience professor and aging researcher Dr. Charles V. Mobbs found that a ketogenic diet reversed diabetic nephropathy (in mice). Have you found “reversal” of any chronic aches/pains or other symptoms since being ketogenic?
Peter: thanks for the site and your feedback.
A bit about me: I decided to lose weight after hitting 257lbs (6’1 frame) and being told I had fatty liver. I decided to change the way I ate after realizing that not only was I NOT losing weight despite running 30 miles a week for 3 months while training for a marathon, I was also losing precious HDL while eating a nutritionist’s recommended “5 fruits a day” for those same 3 months.
Going low-carb helped me get down to 205 within about 4 to 5 months but then I stalled out despite being convinced that I was eating next to no carbs. Unfortunately I still carry a tire of fat and clearly have a lot of visible excess body fat that I need to clear. Over the holidays I took a break and had as much ice cream, candy and cake (while still avoiding pasta, bread, potato, etc.) and am now back up to 216lbs. I’ve also taken up weight lifting and have experimented with varying amounts of protein and even intermittent fasting. I’m starting to suspect my stall was due to excess protein rather than carbs and I’m gearing up to take another run at the magic 200lb mark by increasing fat while decreasing protein to about 100 to 150grams on a consistent basis (I’m keen to keep lifting weights and don’t want to lose muscle mass).
My question (finally) is this: are you still losing fat or weight despite eating nearly 5000 calories a day or are you just maintaining? If you needed to lose more fat would you be consuming fewer overall calories within your ketotic state rather than upping your activity levels? In other words, is it fair to say that it is not that the therodynamic relationship between weight gain/loss and calories in/out doesn’t matter it just doesn’t matter as much or in the ways we’ve been trained to believe? Do you think that people who “stall” during low-carb diets are failing to achieve consistent ketosis due to macronutrient imbalances or is it possible that they’re just eating too much fat and this is what’s stalling their weight loss despite their ketosis? (I’m assuming that too much protein or carbs would kick them out of ketosis so if they have an excess while in ketosis it could only come from fat?)
As an aside, if you had to stop exercising as much as you are currently, how would you change your diet?
Thanks in advance!
Al, you’re raisin some good points. Let’ me try to respond. I have been at weight equilibrium for about 5 months now, so I suspect this is my “new” normal weight and fat content. That said, I’d like to see one more full year go by, especially to know what a summer of long rides does to me in net (i.e., create a caloric deficit or increase appetite further). The bigger question is why here? Why have I “stalled” so to speak at 170-172 pounds, rather than, say 165-167 pounds? When I know the answer to this question, I will be delighted. Unfortunately, I just don’t…at least not yet. Your next question is a testable one, and is one of the reasons Gary and I, along with others, want to create an organization to fund the right kind of studies to answer these questions.
To your last question, when I exercise less my appetite goes down. It seems my weight is almost independent of how much I exercise. In fact, it seems to be about 2-3 lb lower when I do NOT exercise.
Peter,
I’ve found the most cold cuts and other processed meats have in their ingredients dextrose/maltodextrine even though the nutrition label cites 0 carbs (because they’re not required to mention unless greater than 0.5gms I believe). So my question is related to the bacon and sausage patties you consume. Do they have Dextrose (or other ‘ose) in their ingredients? If not I’d love to know what brand these are.
I currently make my own patties, but would love to have the option to buy bacon and sausage patties for variety.
I seek out brands that have as little as possible. With bacon and sausage, as you point out, this can be difficult, but generally it means ingesting up to 3 or 4 gm a day. With other products, like salami, I buy “pure” products without additives.
You have turned my world upside down. You are right in saying that asking what you eat is the wrong way to start. Your diet goes against everything I currently do, maybe that is a good thing. It just seems like a lot to process all at once.
Cynthia, I’m sorry and I’m delighted – at the same time. Don’t try to process it all at once. Step by step…it took me over a year to get my head around all of this, despite my understanding of biochemistry (or possibly, despite it). Enjoy the journey.