In this “Ask Me Anything” (AMA) episode, Peter and Bob discuss all things related to insulin resistance by revisiting the important points made in the fascinating, yet quite technical, episode of The Drive with Gerald Shulman. They devote the entire discussion to understanding the condition known as insulin resistance, how it’s measured, how it manifests in the muscle and liver, and ultimately, what we can do about it.
If you’re not a subscriber and listening on a podcast player, you’ll only be able to hear a preview of the AMA. If you’re a subscriber, you can now listen to this full episode on your private RSS feed or on our website at the AMA #20 show notes page. If you are not a subscriber, you can learn more about the subscriber benefits here.
AMA #20 Sneak Peak:
We discuss:
- Explaining the format of this AMA: Extracting insights from Gerald Shulman’s masterclass on insulin resistance (2:00);
- The basics of insulin, defining insulin resistance (IR), and gold-standard methods of quantifying IR in the muscle (7:15);
- Practical ways to test for insulin resistance in a normal clinical setting (15:45);
- How insulin resistance manifests in the muscle (23:00);
- The biochemical block in glycogen synthesis—drivers and mechanisms resulting in insulin resistance in the muscle (30:45);
- The disparity in fat oxidation between insulin-sensitive and insulin-resistant individuals (44:45);
- The fate of the ingested carbohydrate in someone who is insulin resistant (51:00);
- The prevalence and clinical phenotype of insulin resistance (1:00:15);
- The role of exercise in mitigating and reversing insulin resistance (1:05:00);
- How insulin resistance manifests in the liver (1:09:15);
- Biggest takeaways: what we can do to mitigate and prevent insulin resistance (1:20:45); and
- More.
Explaining the format of this AMA: Extracting insights from Gerald Shulman’s masterclass on insulin resistance [2:00]
Peter recently did a podcast with Gerald Shulman: #140 – Gerald Shulman, M.D., Ph.D.: A masterclass on insulin resistance—molecular mechanisms and clinical implications
- Listening to that discussion was like “drinking through a fire hose” with so much info, so many mechanisms, etc.
- Today’s AMA will be designated to going through the important points of that podcast in a slower way to unlock the takeaways
- Prep for this AMA largely came from Shulman’s Banting Memorial Lecture
Questions to answer today:
How does insulin work under normal circumstances?
What does insulin resistance really mean?
How do we even measure it?
How is insulin resistance manifested in muscle?
How is it manifested in the liver?
How are those the same or different, and what are the consequences of this?
What should you do about this?
“Once you understand the consequences of this, you’ll appreciate how central this is to your health.” —Peter Attia
The basics of insulin, defining insulin resistance (IR), and gold-standard methods of quantifying IR in the muscle [7:15]
The basics of insulin
- Insulin is secreted as what’s called a pro-peptide
- The pancreas secretes something that is inactive and it gets split into insulin and C-peptide (insulin is the active thing)
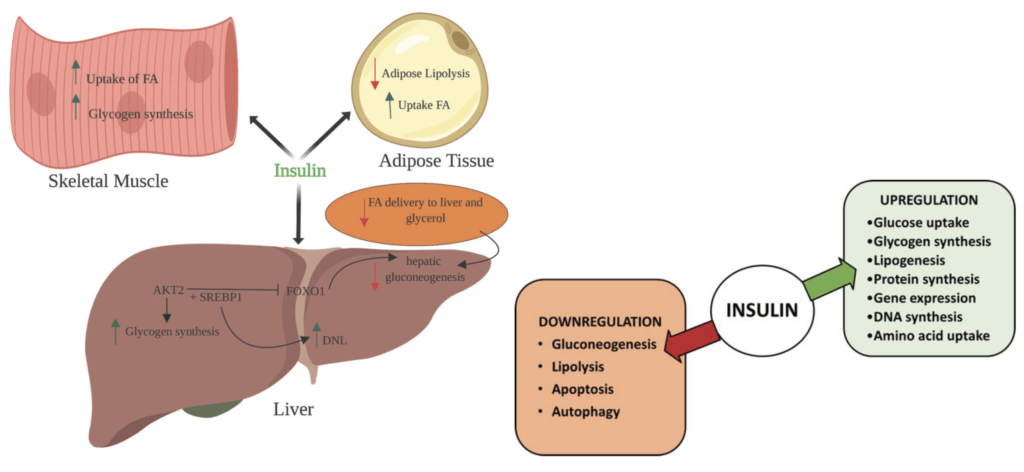
- Insulin as a very anabolic (building/growing) hormone, and does the following:
- Drives glucose into muscles where it can be turned into glycogen
- Plays a role in glycogen synthesis in the liver
- Increases fatty acid uptake into fat cells
- In short: Insulin makes fat cells more fat, it makes muscle cells more glycogen rich, and it makes the liver more glycogen rich.
- It’s a pro-building hormone
Figure 1. Effects of Insulin on Glucose & Lipid metabolism (left, 2019); Critical actions & pathways controlled by insulin (right, 2018).
Defining insulin resistance (IR) and how it’s measured
Definition:
- Insulin resistance is probably best defined as an impaired ability for insulin to do some of the things listed above
- E.g., if insulin’s job is to take glucose into a muscle so that a muscle can make glycogen, when that gets impaired, that is insulin resistance in the muscle
- However, fat cells and liver cells have a slightly different explanation/manifestation of insulin resistance
How insulin is measured (Focusing on the muscle for this discussion)
There are a couple of gold standard ways to measure and quantify insulin resistance that are done in clinical trials (i.e., not something done at the doctor’s office as part of any regular checkup)
1-Hyperinsulinemic-euglycemic clamp technique
- Using to separate IV lines…
- The plasma insulin concentration is acutely raised and maintained at 100 μU/ml by a continuous infusion of insulin.
- Meanwhile, the plasma glucose concentration is held constant at basal levels by a variable glucose infusion.
- When the steady-state (i.e., euglycemic/normal) is achieved, the glucose infusion rate equals glucose uptake by all the tissues in the body (almost exclusively into their muscles)
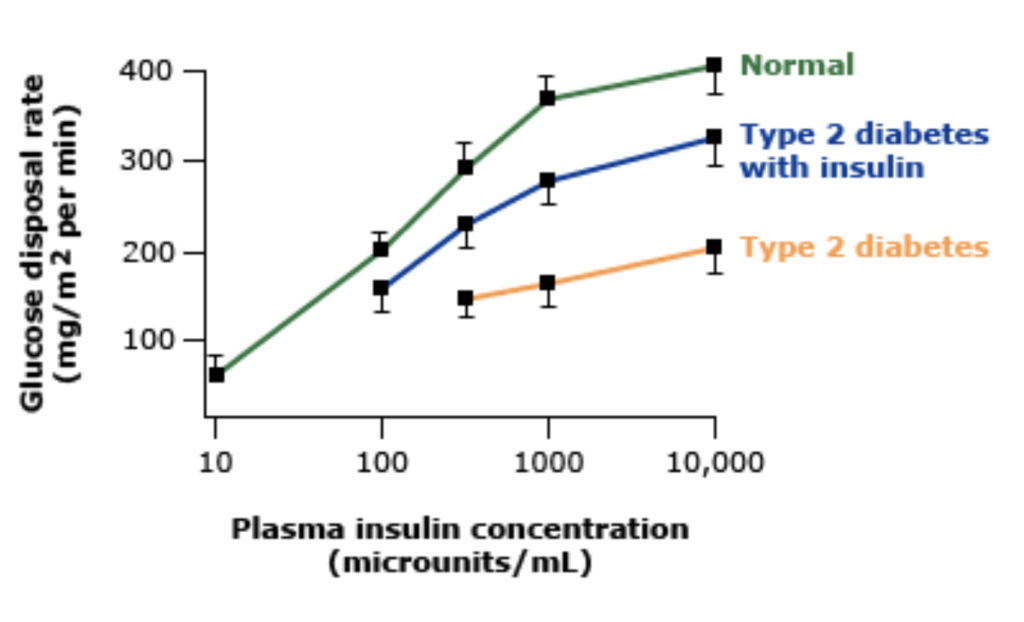
- This is a measure of tissue insulin sensitivity, and the more insulin sensitive you are, the higher that glucose disposal rate will be
Figure 2. [UpToDate]
- The figure above is actually showing glucose disposal, not glucose
- And that’s why the more insulin-sensitive person at a fixed level of insulin requires more and more glucose to maintain glucose homeostasis
2-Insulin suppression test
- Two IV lines
- In one of them you’re infusing epinephrine, propranolol (which suppress your endogenous insulin release) as well as insulin
- in the other IV, you’re infusing glucose
- This is done until you have a steady state level of glucose and insulin
- The way this test works is kind of the opposite of the euglycemic clamp, which is you fix the level of glucose and you’re trying to see how much insulin is required to do that
- Because the steady-state insulin level is the same in all subjects, the height of the steady-state plasma glucose level provides a direct estimate of insulin resistance.
- NOTE: When Peter did this test, he got very, very hypoglycemic and it got a little dangerous
{end of show notes preview}





I think it’s “ drinking from a firehouse”… FYI..great job
Thanks for summing things up. I’d like to see a mix of AMAs, one answering general questions and then one on a specific topic. Some things I was hoping to see mentioned in this AMA on insulin resistance: quality of sleep, stress management, looking at foods from glycemic and insulin index, cold/heat exposure.
Dear Peter and Bob
Amazing episode. I was riveted the whole time. I actually do understand this material better due to this podcast. I hate exercise. But this episode has driven it home how much I need to incorporate it into my life daily.
Coincidentally, I listened the the Schulman podcast yesterday for the second time and understood it much better than the first time, but still had some trouble with the deep dive into the biochem parts.
As a non-biologist who is interested in the nutrition and metabolism I appreciate this ADA to take some of the more complex concepts and put them in terms that can be more easily understood to inform future action.
This is a vote for more of this type of AMA podcast.
I listened to the Shulman podcast 2X- once just audio, once with the show notes handy (lots of 15 sec back buttons both times!) I listened to todays review at my walking desk and have a much better grasp of the nuances- although I still used the 15 sec back button a few times. Definitely convinced me that I need to re-listen to the Zone 2 podcast while I am walking faster and at an incline!
Great episode, I appreciate the new format and hope to see more of these in the future for the complex topics. Thanks to all involved!
Shouldn’t we be standardizing glucose to patient weight in an OGTT?
Years ago, there was a cooking oil sold under the brand name Enova that had a high percent (80%) of DAG and was supposedly healthier than other oils. They claimed the DAG would be used by the liver immediately for fuel and not stored as fat as other oils would. There were studies showing it lowered serum triglycerides and also lead to weight loss. It’s off the market now. I don’t know if its DAG content was the same stereoisomer (sn-1,2) as that implicated in Dr. Shulman’s research as causing insulin resistance. Makes me wonder though if dietary intake of DAG is contributing to insulin resistance?
In insulin resistance, PI3K (phosphatidylinositol 3 kinase) activation is decreased, ultimately leading to impairment of GLUT4 translocation to the cell membrane. There are studies supporting that oral supplementation with myoinositol and/or D-chiro-inositol improves metabolic markers in women with PCOS (polycystic ovarian syndrome) (the pathophysiology of PCOS is rooted in hyperinsulinemia). Could the mechanism by which inositol is working is by somehow upregulating PI3??
Excellent AMA! I especially appreciated reviewing the differences between liver and muscle cell metabolism with respect to insulin resistance.
I found the discussion of the differences between TAG and DAG to be very interesting as a possible reason explaining how intramyocellular lipid impacts glycogen production in insulin resistant muscle. Given the prevalence of diabetes and NAFLD, better understanding of these mechanisms is critical.
I would very much like to see an AMA covering the fate of ingested lipids and the genesis of atherosclerotic vascular disease. I get so many patients that are confused about the metabolism of fat and cholesterol. There is at least as much i not more bias out there with regard to ingested lipids than with glucose/sugars.
Fantastic work – thorough and very accessible. Far and away the most complete explanation of insulin resistance for the interested lay person that I’ve come across. Definitely interested in this type of format as a way of making the science underlying Peter’s podcasts more understandable.
This was great and very appreciated. You did a magnificent work summing the most important facts we were listening to in several podcasts. As an obsessed with IR, I really appreciate the effort. I learned a lot with Dr. Attia and I am proud to apply all this knowledge in regaining my health.
I am weak on biochemistry, physiology, etc consequently I am in the camp with those who want to know more about 1) how to prevent metabolic syndrome and 2) how to treat, or reverse it, once we get it. Thanks for your continued good work.
Great format, I’d love to have more explanatory deep dives like this. I was able to follow it without listening to the original podcast (but I was also looking at the show notes.)
Sometimes the information about a topic is spread out across many podcasts; it’d be great to use a deep dive as a starting point and reference other podcasts on a topic from there.
Hi Peter and Bob,
I’m a UK doctor, longtime listener (first time commenter).
Thank you for compiling this excellent podcast on a topic of such paramount importance.
– I would love to know your thoughts on what is ‘the first domino to fall’ in this process: reduced mitochondrial efficiency/ox phos; adipocyte dysfunction; hypertriglyceridaemia; something else?
– I noted that a discussion on insulin resistance in adipocytes was absent and wondered if this might be of import/interest particularly with respect to hypertrophy vs hyperplasia (and as an aside help to understand the MoA of TZDs).
Thank you for a great AMA. You cited the study of the benefits of Zone 2 training. Is muscle hypertrophy useful in providing more places to dispose of glucose? Thanks again
This was a fantastic podcast. I love connecting the properties of molecules with effects on metabolism so the effects of DAG based on electrons that could cause damage to host proteins was fascinating. Understanding metabolism helps provide motivation for improving and maintaining diet and exercise habits. The bit about oxidative metabolism of glucose being equivalent in diabetics and normals was confusing since glucose would need to be taken in for both glycogen synthesis and oxidative phosporylaton. If uptake is defective, wouldn’t it affect both processes?
Loved this podcast. In addition to the practical thoughts in the final minutes around getting an OGTT, making sure to exercise, reducing sugar and such – I can’t help remembering the very different but also fascinating interview with Jason Fung in episode #59. I’m going to have to go back and listen to that again in light of this episode, but would be curious whether you’d think differently now about Jason’s hyperinsulinemia lens on the problem, as well as the suitcase analogy (which more at the level that I can actually understand).
Simply not eating sometimes, layered on top on a lifestyle where I long ago kicked the sugar habit and already enjoy mountain biking, backcountry snowboarding and similar sports – from a personal standpoint this really seems like the most fundamental and practical way to make sure that insulin resistance doesn’t sneak back in somehow. For the last year some friends and I have just been not eating for the first three days each month – and I think a lot of the reason it sticks is that it is so simple and practical, and it only requires one decision ever.
Did I miss this in the show? What is the average amount of time it takes to make a positive (clinically relevant) change in insulin sensitivity?
Assuming dietary changes and exercise additions…
Very interesting episode. I’ve looked at all the episodes dealing with Zone 2 training, and the one thing I haven’t been able to find is a description of what, if any, changes I should expect to see (without special equipment) over time. For example, if I were doing strength training you might say that over time I would expect to be able to squat with higher weight. But what will I, as an average 57-year-old, be able to see after doing, say 6 months of Zone 2? I’ve currently figured out that if I go at about 85 RPM on my exercise bike, at a particular resistance level, I can go for 45 minutes with my heart rate staying roughly constant in Zone 2. Should I expect that in 6 months I’ll be able to go at, say, 95 RPM? Or is it one of those things where there won’t be obvious gains, and unless I get more sophisticated equipment, I just need to accept that my mitochondria are benefiting? Perhaps this can be addressed in a future AMA.
@Gary, re “I just need to accept that my mitochondria are benefiting? ”
no. You’ll know by tracking your lactate levels. If they go down at the same zone 2 (and above) power out put then your mitochondria (and heart) are getting more efficient (and vice-versa). The cheap proxy for measuring lactate levels is tracking heart rate vs est. power output. Also, if your zone 2 max power level (e.g., at a certain max resistance/speed on your bike) increases (e.g., able to do higher speeds) then that is a way of knowing that you’ve mitochondria got more efficient at burning the cellular fat, which presumably should improve glucose sensitivity over time. That (along w/ HIIT) should also stimulate mitochondrial genesis, the whole grail. BTW, an easy way to gauge what is your zone 2 max for any exercise means is to do the maximum speed/power that keeps your average heart rate in the 2nd half of your workout no more than 5% higher than the average of the first half.
Hope this helps!