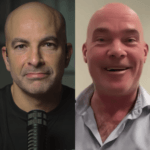
Harold (Hal) Burstein is an internationally renowned breast cancer expert. In this episode, Hal discusses a broad range of topics related to breast cancer, starting with the intricacies of breast anatomy and the endocrinological factors at play. He covers the spectrum of breast cancer, from precancerous lesions to invasive breast cancer, classifying these conditions into a helpful framework. He delves into various screening methods, including self-exams, mammograms, ultrasounds, and MRIs, and addresses the ongoing debate surrounding early screening and detection. Hal provides insights into the latest advancements in cancer treatment, offering valuable guidance for individuals to understand their unique circumstances within the three primary categories of breast cancer. Finally, Hal delves into the role of genetics in breast cancer and brings attention to the less commonly addressed issue of male breast cancer.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- The prevalence and mortality rate of breast cancer in women [4:15];
- The anatomy of the breast and the complex factors behind breast cancer development [6:30];
- The three main categories of breast cancer [16:45];
- Breast cancer risk: the impact of menopause, estrogen, breast density, obesity, and more [21:15];
- Finding and evaluating lumps in the breast [25:30];
- Identifying and treating precancerous lesions like ductal carcinoma in situ (DCIS) [31:00];
- Post-lumpectomy for DCIS: standard of care, future risk of cancer, and pros and cons of radiation and other preventative options [41:15];
- Lobular carcinoma in situ (LCIS): how it differs from DCIS in terms of treatment and future risk of invasive cancer [55:00];
- Breast cancer screening: mammography, ultrasound, MRI, and more [1:03:45];
- Invasive breast cancer: pathology report, surgery, and survival [1:11:00];
- The argument for aggressive screening for breast cancer [1:22:15];
- Advances in the treatment of breast cancer, adjuvant therapy, and neoadjuvant therapy [1:27:00];
- The use of hormone replacement therapy in women who are in remission from breast cancer [1:41:15];
- The role of genetics in breast cancer [1:44:45];
- The importance of multidisciplinary care delivered by cancer centers [1:53:15];
- Breast cancer in men [2:03:30];
- Parting thoughts and takeaways [2:05:45]; and
- More.
The prevalence and mortality rate of breast cancer in women [4:15]
Give listeners a sense of your background, the post you sit in, and the work you do
- Hal is a professor of medicine at Harvard Medical School and a medical oncologist here at Dana-Farber Cancer Institute where he specializes in breast cancer
- He trained in medical school as an M.D. Ph.D. student and got a Ph.D. in immunology
- Following that, he was a house officer studying internal medicine at Mass General and came over to Dana-Farber to do medical oncology where he’s been for the reminder of his career
- In his day-to-day work, he sees a lot of patients who
- He runs a very active and busy clinic at Dana-Farber
- He’s involved in a lot of teaching at the medical school
- He does a lot of both clinical research and clinical education
- Including guidelines work with ASACO, the NCCN, the St Gallen Pathways, and other international and national groups interested in breast cancer care
Give people a sense of the magnitude of breast cancer. What is a woman’s lifetime incidence of breast cancer?
“The famous statistic is that American women have about a one in eight lifetime risk or 12% lifetime risk of developing breast cancer.”‒ Harold Burstein
- The good news is that only a small fraction of those will be fatal
- The mortality associated with breast cancer depends on the stage at which it is caught
- It also depends on the subtype of breast cancer because we have different treatment programs for each of the different subtypes of breast cancer
- If you look very broadly across the board, there are roughly 275,000 cases of breast cancer in the United States every year, and there are roughly 38,000 deaths
- If you assume a steady state, we are curing 80-85% of women with breast cancer, but roughly 15-18% are still at jeopardy for recurrence and death from the disease
The anatomy of the breast and the complex factors behind breast cancer development [6:30]
- One of the challenges of diagnosing breast cancer is that you don’t get to look directly at the place where the tumor arises, the way you do, for example, with colon cancer or skin cancer or cervical cancer
- It probably behooves us to spend some time explaining everything from the embryology to the prepubescent anatomy to the maturation process of the breast, and then perhaps even what happens during menopause
How would you describe the development and changes of a breast during a woman’s life with a specific nod to how this will factor into helping us understand the pathology of breast cancer development during some of those stages?
- The breast is a gland
- It is fundamentally a sweat gland
- If you look at the pure embryology of it, it is the defining feature of what it is to be a mammal
- The breast goes through different stages of maturation and development in the life of a woman
- It begins as a quiescent area of tissue and then during puberty, because of the hormonal changes, develops enlargement and maturation of the glands such that they become able to eventually secrete milk if the woman becomes pregnant
- The breast is largely composed of two types of tissue
- 1 – The majority of the volume is actually just fat and non-specific stromal elements and the thing that determines the size of the breast in a woman is just really how much non glandular tissue there is
- 2 – Glandular tissue
- All women more or less have the same amount of glandular tissue in the breast (the milk generating component of the breast), and those ducks radiate from the various breast tissues into the nipple
- The nipple has multiple orifices, and the God-given purpose here is to nurse the child
Breast cancers largely arise from the ductal or the glandular tissue, and in this respect, breast cancer shares its origins with almost all common cancers, prostate cancer, colon cancer, lung cancer, where it is the glandular part of the organ from which arises the malignant cell
- One of the interesting things about breast cancer and normal breast development is that there has been over the past decades, a rise in the incidence of breast cancer (the rate of breast cancer), and one of the likely contributors relates to the early puberty that we are now seeing in women
- Girls are starting to menstruate at a far younger age in the 2020s than they were 100 years ago or certainly 150 years ago, owing probably to better nutrition and better general health
- That means that the breast development and the exposure of the breast to estrogens starts earlier
- And women are also menstruating for longer, again, largely owing to better health
- Women are having, at the population level in the developed countries at least, fewer children, and they tend to nurse those children for a shorter duration of time
- Again, this rarely describes an individual patient, but at the population level
The rates of breast cancer are highest in the most developed societies, and many people think it relates to these issues of childhood nutrition, pubescent nutrition, number of pregnancies, duration of nursing, and that accounts for a lot of the difference in the incidence rates that we see between the United States and other parts of the world
- As other societies become more developed, their rates of breast cancer tend to go up to mirror those of the US or Western European populations
Peter remembers from medical school
- A study of Japanese women (nearly 30 years ago) who moved to the United States and within a generation went from very, very low rates of breast cancer to assuming the same high rate of breast cancer as American women
- For Peter, the takeaway of that was we could never know what the causative driver was, given that there are so many things that are happening
- But clearly there’s an environmental component to this, whether it’s some combination of food, exercise, hormones, stress levels, pollution
- You would have a very long list of things that could change, that could amount for such a dramatic shift as opposed to saying, for example, there’s genetic differences that are accounting for this
- We’re obviously going to talk at length about the genetic drivers of this, but that wouldn’t explain the one generation shift
Hal points out historical epidemiology on two cancers you can see
- Back to the 19th century, one of the first cancer epidemiological findings was that nuns who never became pregnant were at greater risk for developing breast cancer
- Peter asks how high the hazard ratios were for nuns versus non-nuns, but Hal isn’t sure they even articulated hazard ratios at that time
- This predates radiology
- Nowadays we would say their risk is higher because they were never pregnant or nursing
- Along with the discovery of scrotal cancers in chimney sweeps, it was one of the first real steps forward in the epidemiology of cancer biology to help people begin to get a sense of what was causing cancer
- The hazard ratios were alarmingly high, around 4, 5, or 6
- It was very easy to make the causal link
- Hal agrees that the environment in which a person grows up is going to have an impact on their breast cancer risk
- By which he doesn’t specifically mean the atmosphere or the pollutants or all those kinds of things
- The dilemma here is that for any given individual, we almost never have a good sense of what their intrinsic risk of breast cancer is aside from the family history in genetic cancers
- Why they get breast cancer now
- Why they got it in one breast and not the other breast
- All those things remain very mysterious
- For someone who takes care of breast cancer patients, it’s a source of real frustration
- There are some tumors where we really think we understand why they’re at greater risk
- The smoking and lung cancer, at least you can imagine how this arose
- Whereas breast cancer is often a disease of very healthy women, women who have gone to great lengths to care for themselves, and despite that, they are encountering breast cancer diagnosis (which is often frustrating)
Things that drive risk of developing breast cancer
The interaction between pregnancy and breast cancer risk is both very interesting and complicated
- Multiple pregnancies lower the risk of breast cancer
- 1 – Pregnancy transiently increases the risk, and then it comes down as time goes by and no pregnancies are associated with a slightly higher risk of developing breast cancer
- And that’s not related to the in vitro fertilization or other hormonal supplements
- They’ve looked at that with a lot of rigor, particularly the Scandinavian databases where they have outstanding public health registries of all the patients in the Scandinavian countries
- Infertility, for instance, is a slight risk for breast cancer, but the treatments for infertility per se are not
When we talk about increased risk, there’s a huge difference between a population increased risk and the risk for a given patient
- At the outset, we said 1 in 8 lifetime risk in the United States (that’s 12-13%)
- A woman who has early onset of menstruation or hormone replacement therapy such that they have longer estrogen exposure or shorter period of nursing or fewer pregnancies, they might have a 25 or 30% greater risk of breast cancer
- But that only moves the needle from around 12% to around 15%
- Hal points out, “The risk at the population level is big, the risk for an individual is still pretty small for these kinds of factors.”
Do we have a sense of the difference between things that drive the increase in risk versus things that drive an increase in mortality? [15:15]
- Peter points out, “In prostate cancer, it’s generally well understood that the prevalence of prostate cancer approximates the decade of life of the male.”
- Basically half of men in their 50s have some prostate cancer (Gleason 3+3)
- This is not a prostate cancer you would take out, but on autopsy you would find it
- By the time a guy is in his 70s, you might expect there’s a 70% chance he has prostate cancer
- Of course the challenge then of the urologist is understanding which man is going to die from versus with prostate cancer
- Basically half of men in their 50s have some prostate cancer (Gleason 3+3)
- Peter has covered the topic of hormone replacement therapy (HRT) in such detail that it needs no further rehashing, but the punchline is while the Women’s Health Initiative demonstrated that women taking conjugated equine estrogen plus MPA had a 25% increase in the risk of breast cancer, it never translated to an increase in mortality
Do we have a sense of which risk factors are driving mortality versus just incidence?
- No and yes
- At the population level, this gets us into the subsets of the different cancers that we speak about
The three main categories of breast cancer [16:45]
There are really three major flavors of breast cancer
{end of show notes preview}

Harold Burstein, M.D., Ph.D.
Harold Burstein earned his M.D. at Harvard Medical School. He also earned his Ph.D. in cellular immunology and a master’s degree in the history of science from Harvard. He completed his residency in internal medicine at Massachusetts General Hospital and a hematology/oncology fellowship at Dana-Farber Cancer Institute. Dr. Burstein is a clinician and clinical investigator in the Breast Oncology Center at Dana-Farber Cancer Institute, a Professor of Medicine at Harvard Medical School, and a staff physician at Brigham and Women’s Hospital. He has led and participated in multiple clinical trials, and developed national and international breast cancer treatment guidelines. Recognized as one of the leading breast oncologists, he is a perennial “Top Doctor” in the US for breast cancer care. He teaches students, residents and fellows at Harvard Medical School and Dana-Farber. [Dana-Farber Cancer Institute]





How do I know my oncologist is up to date with the treatments they are prescribing?
This was a great. I appreciate all the information and extra push to get genetic counseling. My mother is a three time breast cancer survivor, and my maternal grandmother is a one time breast cancer survivor, yet my mother has recently tested negative for the BRAC genes. She also has breast cancer on her father’s side, to us daughters is concerning to say the least. And as a breast cancer advocate in our country, as well as running a non profit in our country, breast cancer is a daily topic and a concern for myself as well the rest of my family.
Thank you
Great comprehensive look at breast cancer! Thanks. Surprising though that there was no discussion of lifestyle modification both during cancer treatment and during survivorship where exercise alone reduces recurrence rates by over 40% approaching the impact of anti-estrogen strategies. Combining exercise with weight loss (if obese), diet, good sleep and stress reduction is likely more beneficial than any conventional approach to recurrence reduction.