Want to catch up with other articles from this series?
- The straight dope on cholesterol – Part I
- The straight dope on cholesterol – Part II
- The straight dope on cholesterol – Part III
- The straight dope on cholesterol – Part IV
- The straight dope on cholesterol – Part V
- The straight dope on cholesterol – Part VI
- The straight dope on cholesterol – Part VII
- The straight dope on cholesterol – Part VIII
- The straight dope on cholesterol – Part IX
In Part I, Part II, Part III and Part IV of this series, we addressed these 6 concepts:
#1 — What is cholesterol?
#2 — What is the relationship between the cholesterol we eat and the cholesterol in our body?
#3 — Is cholesterol bad?
#4 — How does cholesterol move around our body?
#5 – How do we measure cholesterol?
#6 – How does cholesterol actually cause problems?
Quick refresher on take-away points from previous posts, should you need it:
- Cholesterol is “just” another fancy organic molecule in our body but with an interesting distinction: we eat it, we make it, we store it, and we excrete it – all in different amounts.
- The pool of cholesterol in our body is essential for life. No cholesterol = no life.
- Cholesterol exists in 2 forms – unesterified or “free” (UC) and esterified (CE) – and the form determines if we can absorb it or not, or store it or not (among other things).
- Much of the cholesterol we eat is in the form of CE. It is not absorbed and is excreted by our gut (i.e., leaves our body in stool). The reason this occurs is that CE not only has to be de-esterified, but it competes for absorption with the vastly larger amounts of UC supplied by the biliary route.
- Re-absorption of the cholesterol we synthesize in our body (i.e., endogenous produced cholesterol) is the dominant source of the cholesterol in our body. That is, most of the cholesterol in our body was made by our body.
- The process of regulating cholesterol is very complex and multifaceted with multiple layers of control. I’ve only touched on the absorption side, but the synthesis side is also complex and highly regulated. You will discover that synthesis and absorption are very interrelated.
- Eating cholesterol has very little impact on the cholesterol levels in your body. This is a fact, not my opinion. Anyone who tells you different is, at best, ignorant of this topic. At worst, they are a deliberate charlatan. Years ago the Canadian Guidelines removed the limitation of dietary cholesterol. The rest of the world, especially the United States, needs to catch up. To see an important reference on this topic, please look here.
- Cholesterol and triglycerides are not soluble in plasma (i.e., they can’t dissolve in water) and are therefore said to be hydrophobic.
- To be carried anywhere in our body, say from your liver to your coronary artery, they need to be carried by a special protein-wrapped transport vessel called a lipoprotein.
- As these “ships” called lipoproteins leave the liver they undergo a process of maturation where they shed much of their triglyceride “cargo” in the form of free fatty acid, and doing so makes them smaller and richer in cholesterol.
- Special proteins, apoproteins, play an important role in moving lipoproteins around the body and facilitating their interactions with other cells. The most important of these are the apoB class, residing on VLDL, IDL, and LDL particles, and the apoA-I class, residing for the most part on the HDL particles.
- Cholesterol transport in plasma occurs in both directions, from the liver and small intestine towards the periphery and back to the liver and small intestine (the “gut”).
- The major function of the apoB-containing particles is to traffic energy (triglycerides) to muscles and phospholipids to all cells. Their cholesterol is trafficked back to the liver. The apoA-I containing particles traffic cholesterol to steroidogenic tissues, adipocytes (a storage organ for cholesterol ester) and ultimately back to the liver, gut, or steroidogenic tissue.
- All lipoproteins are part of the human lipid transportation system and work harmoniously together to efficiently traffic lipids. As you are probably starting to appreciate, the trafficking pattern is highly complex and the lipoproteins constantly exchange their core and surface lipids.
- The measurement of cholesterol has undergone a dramatic evolution over the past 70 years with technology at the heart of the advance.
- Currently, most people in the United States (and the world for that matter) undergo a “standard” lipid panel, which only directly measures TC, TG, and HDL-C. LDL-C is measured or most often estimated.
- More advanced cholesterol measuring tests do exist to directly measure LDL-C (though none are standardized), along with the cholesterol content of other lipoproteins (e.g., VLDL, IDL) or lipoprotein subparticles.
- The most frequently used and guideline-recommended test that can count the number of LDL particles is either apolipoprotein B or LDL-P NMR, which is part of the NMR LipoProfile. NMR can also measure the size of LDL and other lipoprotein particles, which is valuable for predicting insulin resistance in drug naïve patients, before changes are noted in glucose or insulin levels.
- The progression from a completely normal artery to a “clogged” or atherosclerotic one follows a very clear path: an apoB containing particle gets past the endothelial layer into the subendothelial space, the particle and its cholesterol content is retained, immune cells arrive, an inflammatory response ensues “fixing” the apoB containing particles in place AND making more space for more of them.
- While inflammation plays a key role in this process, it’s the penetration of the endothelium and retention within the endothelium that drive the process.
- The most common apoB containing lipoprotein in this process is certainly the LDL particle. However, Lp(a) and apoB containing lipoproteins play a role also, especially in the insulin resistant person.
- If you want to stop atherosclerosis, you must lower the LDL particle number.
Concept #7 – Does the size of an LDL particle matter?
There are few, if any, topics in lipidology that generate more confusion and argument that this one. I’ve been leading up to it all month, so I think the time is here to address this issue head on. I’ve read many papers and seen many lectures on this topic, but the one that stole my heart was a lecture given by Jim Otvos at the ADA 66th Scientific Sessions in Washington, DC. Some of the figures I am using in this post are taken directly or modified from his talk or subsequent discussions.
At the outset of this discussion I want to point out two clinical scenarios to keep in mind:
- The most lethal lipoprotein disorder is familial hypercholesterolemia, which I have discussed in previous posts. Such patients all have large LDL particles, but most of these patients die in childhood or early adulthood if not treated with medications to reduce particle number.
- Conversely, diabetic patients and other patients with advanced metabolic syndrome have small LDL particles, yet often live well into their 50s and 60s before succumbing to atherosclerotic diseases.
The common denominator is that both sets of patients in (1) and (2) have high LDL-P. What I’m going to attempt to show you today is that once adjusted for particle number, particle size has no statistically significant relationship to cardiovascular risk. But first, some geometry.
“Pattern A” versus “Pattern B” LDL
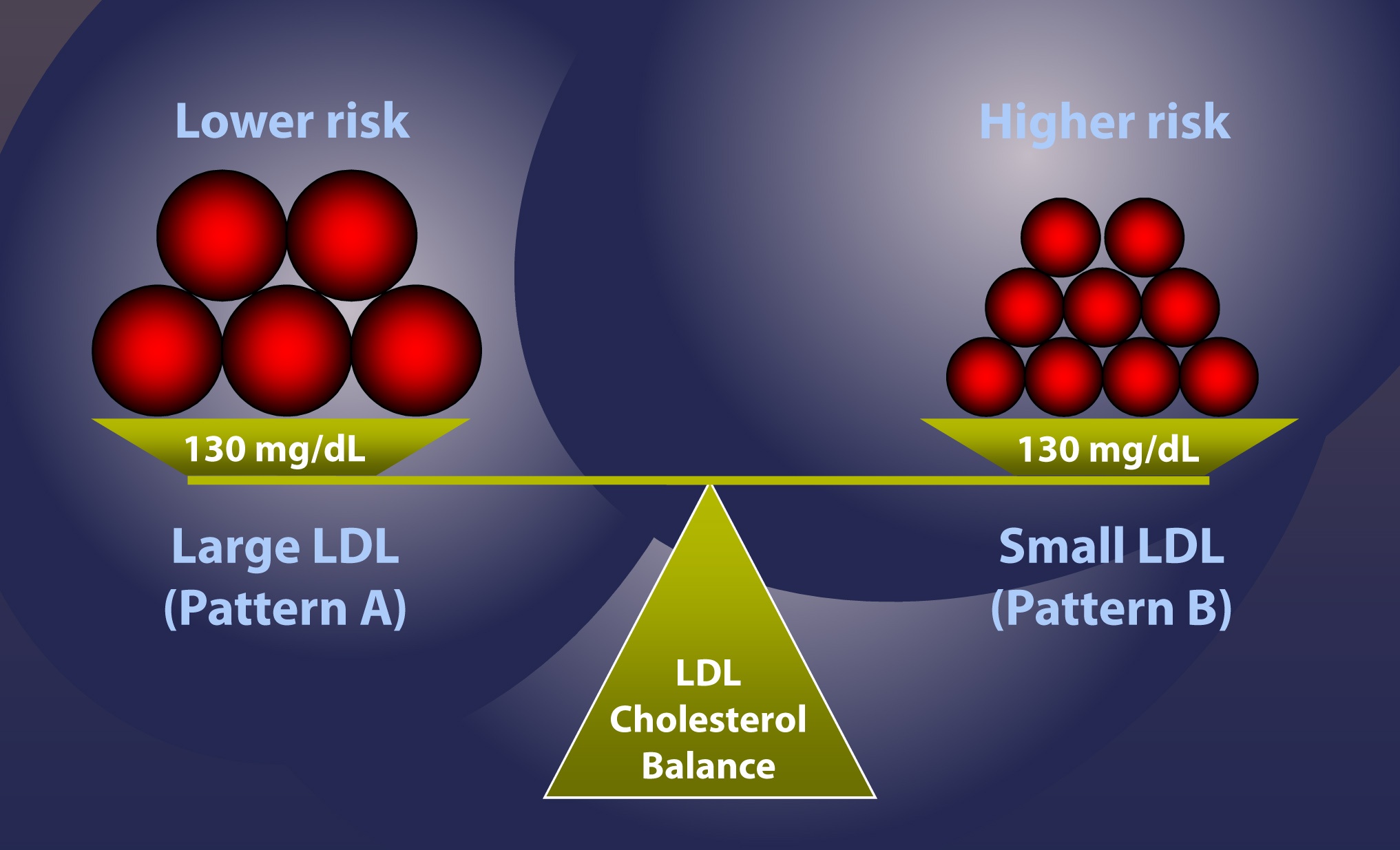
The introduction of gradient gel electrophoresis about 30 years ago is what really got people interested in the size of LDL particles. There is no shortage of studies of the past 25 years demonstrating that of the following 2 scenarios, one has higher risk, all other things equal. [This is a big disclaimer and I went back and forth for a while before deciding to include this point. It is an uncharacteristic oversimplification. If you’ve been reading this blog for a while, you’ll know I’m rarely accused of that sin – but I’m about to be].
Here’s the example: Consider 2 patients, both with the same total content of cholesterol in their LDL particles, say, 130 mg/dL. Furthermore, assume each has the “ideal” ratio of core cholesterol ester-to-triglyceride (recall from Part I and III of this series, this ratio is 4:1). I’m going to explain in a subsequent post why this assumption is probably wrong as often as it’s right, but for the purpose of simplicity I want to make a geometric point.
- LDL-C = 130 mg/dL, Pattern A (large particles) – person on the left in the figure below
- LDL-C = 130 mg/dL, Pattern B (small particles) – person on the right in the figure below
Under the set of assumptions I’ve laid out, case #2 is the higher risk case. In other words, at the same concentration of cholesterol within LDL particles, assuming the same ratio of CE:TG, it is mathematically necessary the person on the right, case #2, has more particles, and therefore has greater risk.
Bonus concept: What one really must know is how many cholesterol molecules there are per LDL particle. It always requires more cholesterol-depleted LDL particles than cholesterol-rich LDL particles to traffic cholesterol in plasma, and the number of cholesterol molecules depends on both size and core TG content. The more TG in the particle, the less the cholesterol in the particle.
So why does the person on the right have greater risk? Is it because they have more particles? Or is it because they have smaller particles?
This is the jugular question I want to address today.
If you understand that the person on the right, under the very careful and admittedly overly simplified assumptions I’ve given, is at higher risk than the person on the left, there are only 4 possible reasons:
- Small LDL particles are more atherogenic than large ones, independent of number.
- The number of particles is what increases atherogenic risk, independent of size.
- Both size and number matter, and so the person on the right is “doubly” at risk.
- Neither feature matters and these attributes (i.e., size and number) are markers for something else that does matter.
Anyone who knows me well knows I love to think in MECE terms whenever possible. This is a good place to do so.
I’m going to rule out Reason #4 right now because if I have not yet convinced you that LDL particles are the causative agent for atherosclerosis, nothing else I say matters. The trial data are unimpeachable and there are now 7 guidelines around the world advocating particle number measurement for risk assessment. The more LDL particles you have, the greater your risk of atherosclerosis.
But how do we know if Reason #1, #2, or #3 is correct?
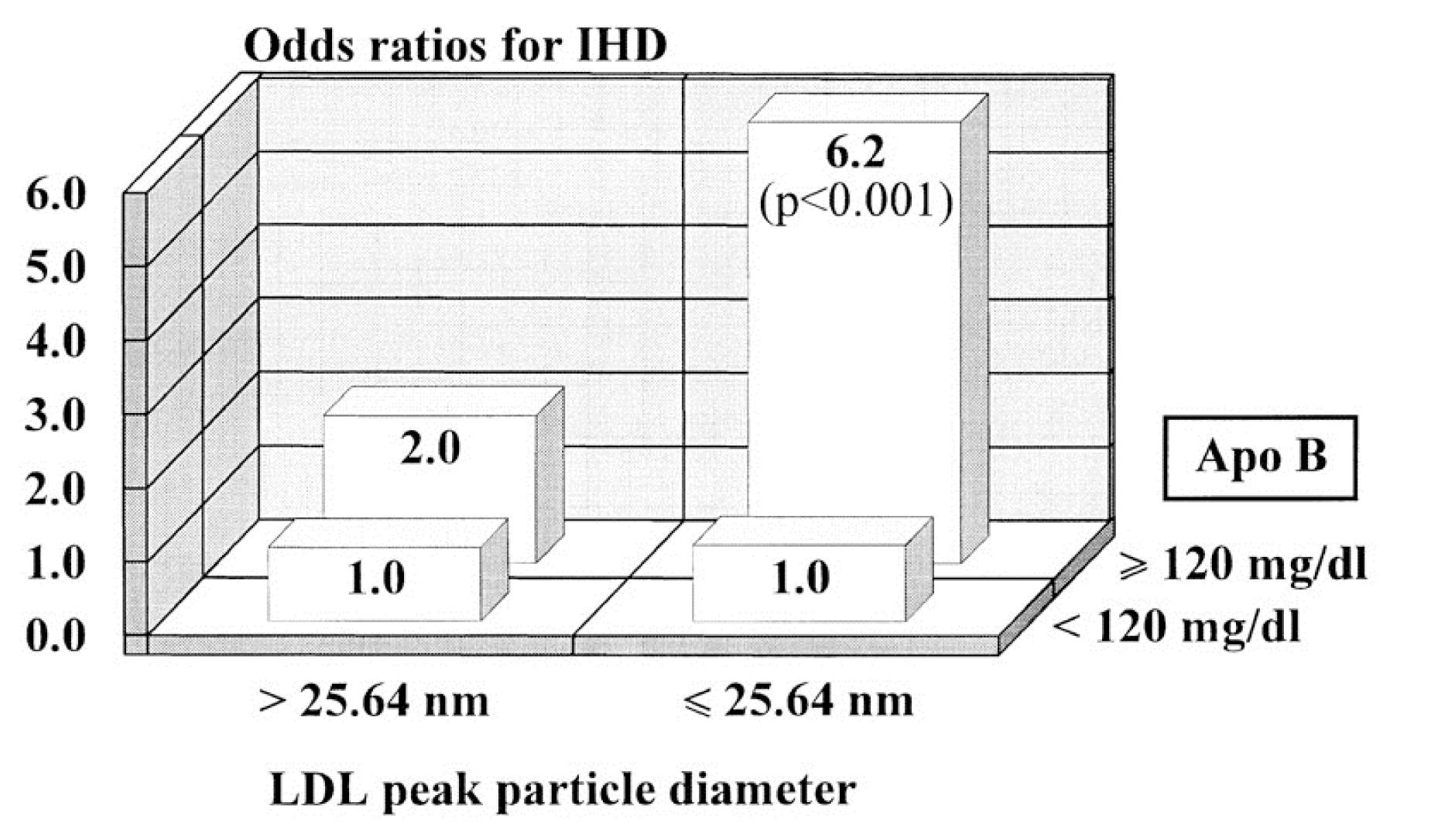
This figure (one of the most famous in this debate) is from the Quebec Cardiovascular Study, published in 1997, in Circulation. You can find this study here.
This is kind of a complex graph if you’re not used to looking at these. It shows relative risk – but in 2 dimensions. It’s looking at the role of LDL size and apoB (a proxy for LDL-P, you’ll recall from previous posts). What seems clear is that in patients with low LDL-P (i.e., apoB < 120 mg/dl), size does not matter. The relative risk is 1.0 in both cases, regardless of peak LDL size. However, in patients with lots of LDL particles (i.e., apoB > 120 mg/dl), smaller peak LDL size seems to carry a much greater risk – 6.2X.
If you just looked at this figure, you might end up drawing the conclusion that both size and number are independently predictive of risk (i.e., Reason #3, above). Not an illogical conclusion…
What is not often mentioned, however, is what is in the text of the article:
“Among lipid, lipoprotein,and apolipoprotein variables, apo B [LDL-P] came out as the best and only significant predictor of ischemic heart disease (IHD) risk in multivariate stepwiselogistic analyses (P=.002).”
“LDL-PPD [peak LDL particle diameter] — as a continuous variable did not contribute to the risk of IHD after the contribution of apo B levels to IHD risk had been considered.”
What’s a continuous variable? Something like height or weight, where the possible values are infinite between a range. Contrast this with discrete variables like “tall” or “short,” where there are only two categories. For example, if I define “tall” as greater than or equal to 6 feet, the entire population of the world could be placed in two buckets: Those who are “short” (i.e., less than 6 feet tall) and those who are “tall” (i.e., those who are 6 feet tall and taller). This figure shows LDL size like it’s a discrete variable – “large” or “small” – but obviously it is not. It’s continuous, meaning it can take on any value, not just “large” or “small.” When this same analysis is done using LDL size as the continuous variable it is, the influence of size goes away and only apoB (i.e., LDL-P) matters.
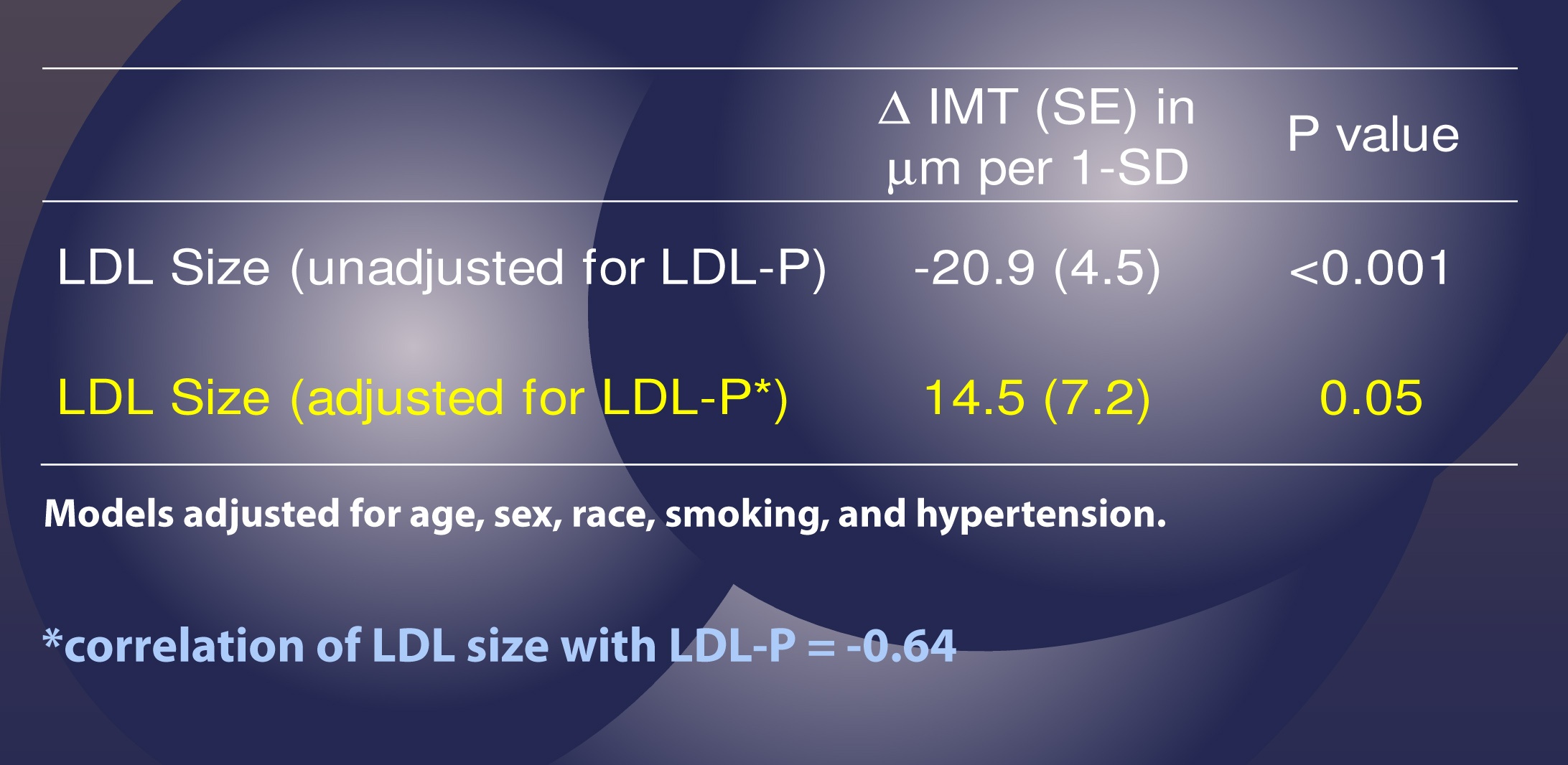
This effect has been observed subsequently, including the famous Multi-Ethnic Study of Atherosclerosis (MESA) trial, which you can read here. The MESA trial looked at the association between LDL-P, LDL-C, LDL size, IMT (intima-media thickness – the best non-invasive marker we have for atherosclerosis), and many other parameters in about 5,500 men and women over a several year period.
This study used the same sort of statistical analysis as the study above to parse out the real role of LDL-P versus particle size, as summarized in the table below.
This table shows us that when LDL-P is NOT taken into account (i.e., “unadjusted” analysis), an increase of one standard deviation in particle size is associated with 20.9 microns of LESS atherosclerosis, what one might expect if one believes particle size matters. Bigger particles, less atherosclerosis.
However, and this is the important part, when the authors adjusted for the number of LDL particles (in yellow), the same phenomenon was not observed. Now an increase in LDL particle size by 1 standard deviation was associated with an ADDITIONAL 14.5 microns of atherosclerosis, albeit of barely any significance (p=0.05).
Let me repeat this point: Once you account for LDL-P, the relationship of atherosclerosis to particle size is abolished (and even trends towards moving in the “wrong” direction – i.e., bigger particles, more atherosclerosis).
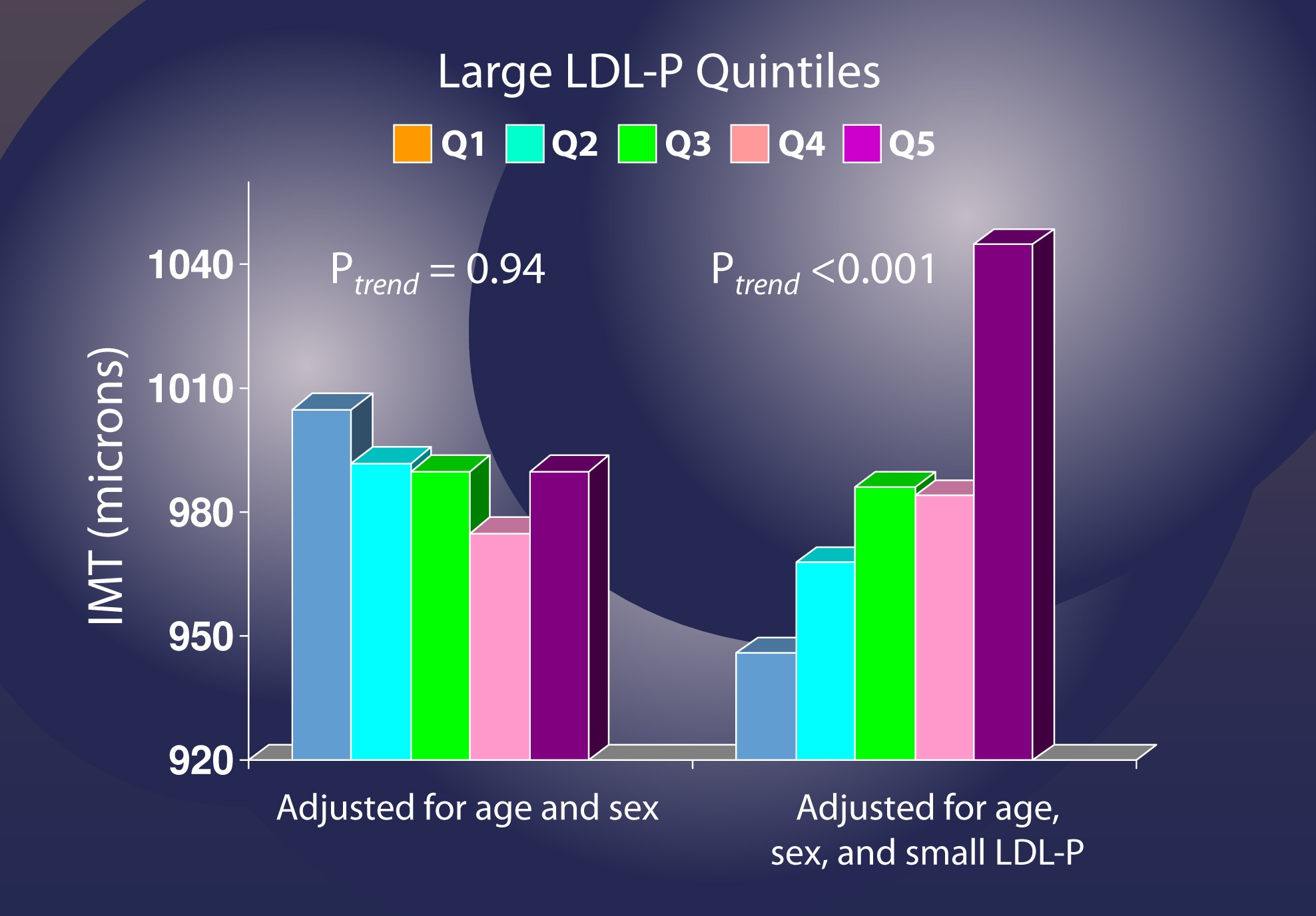
Let me use another analysis to illustrate this point again. If you adjust for age and sex, but not LDL-P [left graph, below], changes in the number of LDL particles (shown in quintiles, so each group shows changes by 20% fractions) seem to have no relationship with IMT (i.e., atherosclerosis).
However, when you adjust for small LDL-P [right graph, below], it becomes clear that increased numbers of large LDL particles significantly increase risk.
I’ve only covered a small amount of the work addressing this question, but this issue is now quite clear. A small LDL particle is no more atherogenic than a large one, but only by removing confounding factors is this clear. So, if you look back at the figure I used to address this question, it should now be clear that Reason #2 is the correct one.
This does not imply that the “average” person walking around with small particles is not at risk. It only implies the following:
- The small size of their particles is probably a marker for something else (e.g., metabolic derangement due to higher trafficking of triglycerides within LDL particles);
- Unless you know their particle number (i.e., LDL-P or apoB), you actually don’t know their risk.
Let’s wrap it up here for this week. Next week we’ll address another question that’s probably been on your mind: Why do we need to measure LDL-P or apoB? Isn’t the LDL-C test my doctor orders enough to predict my risk?
Summary
- At first glance it would seem that patients with smaller LDL particles are at greater risk for atherosclerosis than patients with large LDL particles, all things equal. Hence, this idea that Pattern A is “good” and Pattern “B” is bad has become quite popular.
- To address this question, however, one must look at changes in cardiovascular events or direct markers of atherosclerosis (e.g., IMT) while holding LDL-P constant and then again holding LDL size constant. Only when you do this can you see that the relationship between size and event vanishes. The only thing that matters is the number of LDL particles – large, small, or mixed.
- “A particle is a particle is a particle.” If you don’t know the number, you don’t know the risk.
By NASA Mercury image: JHUAPLVenus image: JPLMars image: HST [Public domain], via Wikimedia Commons



Dear Dr. Attia: Great series of posts! Then the only way to get one’s LDL-P is through an NMR test? If so, would you consider Acessa Lab as a decent online lab?
Thanks!
If and only if they have Liposcience do the NMR part. No other company has FDA approval to do this. The other option is to have an approved ApoB test as reasonable proxy.
I suggest that soon you will be taking and passing the certifying exam for Lipidologist! We non M.D.’s will know more than our docs and might pass a junior level exam!
IMT is not perfect in assessing coronary artery disease. I have a normal IMT score with no plaque ,but CAD determined through CAC score. While it appears that small particles may not matter, I just wonder a bit given that my plaque buid up is in a narrower smaller artery, but not in the main larger ones which are plaque free. All this in the face of lots of small LDL(now corrected with meds) The carotid artery and architecture of the heart are different and it may be that if you have issues with the IMT you will have issues in the heart, but just because the IMT is clear does not mean no issues with the heart. The more I learn the more I become convinced that genetics play an overwhelming role in this disease. Will be interested in your take on diet and sat fat in regard to this subject because one view can be if size of particles do not matter can be that diet does not matter if particle number is at acceptable level. Be interested in your thoughts!
Dr. Attia:
I checked with Accesa, and they process NMR through a company called LabCorp., not Liposcience. I checked the web site of Liposcience, and they apparently do not process requests online, etc. So my question is, if this test is so critical, why is it so hard to get one? My doctor just blinks his eyes when I say NMR.
Any suggestions?
Thanks!
Get an apoB test instead.
I had my NMR done several years ago through LabCorps. They do it through LipoScience. It cost $98.
I don’t understand why Berkeley Heart Labs won’t do any tests without a prescription.
DirectLabs.com
No prescription needed in most states. My doctor wouldnt order an NMR and I didnt want to push him. He let me get my thyroid panels but wouldnt prescribe rT3, so I had some tests via labcorp and some tests via directlab. Turns out Directlab uses labcorp so I got both sets of tests at the same blood draw… the only diff is that the prescription goes through insurance and the results go to my doc… and I get the results from directlab directly (and my doc doesnt get the info). How F&&&ked up is that? Oh well… at least you can do it.
Labcorp sends the blood to LipoScience — so get the LDL-P via Accesa.
Dear Joe,
the LipoScience website says that LabCorp (with a certain order number) sends those NMR tests to LipoScience. I think that’s what they’re saying. So you may be able to get it through your Accessa LabCorp thing after all.
Quest’s DirectPay program has a comprehensive wellness test that includes, amongst other things, Total cholesterol, High Density Lipoprotein Cholesterol (HDL), calculated Low Density Lipoprotein Cholesterol (LDL), Triglycerides, calculated cholesterol/HDL ratio.
https://my.blueprintforwellness.com/direct/
Peter,
Nothing you have written in the previous posts comes even close to establishing this “I’m going to rule out Reason #4 right now because if I have not yet convinced you that LDL particles are the causative agent for atherosclerosis, nothing else I say matters.” Weak associations, no matter how many times it appears is not causation. The seat belt analogy is not a valid analogy. The MESA study that you have done a nice job rehashing was interpretted in a manner consistant with the funding source and the authors interests. Concentration gradient may likely be a factor once damage begins, particularly when the LDL-p are damaged, but it is not root cause for the initial damage. Undamaged LDL-p, regardless of the concentration, don’t damage the healthy artery.
Stuart, what experiment would you suggest to resolve this? In other words, in a human, how would you manipulate the variables DIRECTLY in a controlled manner? The role of LDL in atherosclerosis is, unfortunately, in the same category as seat belts and smoking. It’s very difficult to do the PERFECT experiment. However, the associations are very strong – much stronger than the associations in nutrition. When a RR difference is 1.3 (“strong” by nutrition standards), it’s hard to make a link. But when it’s 10x AND you have no other way to do the experiment, it becomes more compelling. Ultimately, though, I would ask you, if you’d don’t buy the role of LDL-P reduction in the treatment of atherosclerosis, what treatment are you proposing to reduce atherosclerosis?
Ultimately it is nutrition. Damage to the artery is caused by many things but it is minimized by adequate nutrition and avoiding toxins. There is no evidence that decreasing LDL-p with conventional treatment descreases overall mortality.
“There is no evidence that decreasing LDL-p with conventional treatment descreases overall mortality.” Categorically false, but I’ll let your peers call you out on this.
An apoB test appears to be more affordable than the NMR test. Is it an acceptable subsitute? What are the reference ranges?
https://www.lef.org/Vitamins-Supplements/ItemLC216010/Apolipoprotein-Assessment-Apo-A1–B–Ratio-Blood-Test.html
Yes, apoB, provided it is measured not estimated, is acceptable.
For apoB and LDL-P study see
https://www.lipidcenter.com/pdf/Framingham.pdf
Hello Dr. Attia: Thanks for the informing posts. I understand that dietary fat can increase Pattern A LDL. If so, is there a ceiling point to which the increase will cease or will it continue to increase leading to an elevated particle number? After reading your personal diet it is unlikely to be the latter however, I would like to hear your input on the matter.
Thanks,
Nathan
Reducing carb and specifically sugar intake, even in the presence of very high amounts of fat does push most people more to the pattern A side, but this is a side issue and is only relevant if LDL-P is being reduced.
With respect to this point, doesn’t there seem to be a correlation (though maybe not always, or maybe only in some people) between more pattern A LDL-p and overall lower levels of LDL-p (because larger particles are carrying more cholesterol, reducing the amount of particles needed to carry the cholesterol around the body), or am I reading this into the posts mistakenly?
Also, given some peoples’ comments regarding seeing increases in LDL-p in their NMR tests despite being low carb high fat, I am interested to know what your experience has been with your LDL-p levels througout your journey. Were they high to begin with, low; did they go up at any point, down; where were you in your most recent NMR test?
And lastly, since it seems as though your research (or review of the research of the leaders in the field) has led you to believe LDL-p is the single most important, and possibly the only relvant, factor to assess risk of artherosclerosis (I hope I’m correct in that assumption), if reducing carb and sugar intake is not lowering LDL-p, independent of the amount and/or type of fat consumed, then a) why is this relevant to the War on Insulin and low carb high fat nutrition, b) what would need to be done in conjunction with low carb to achieve a reduction in LDL-p, and c) what’s the point of going low carb to reduce metabolic disease risk factors if you raise LDL-p and put yourself at higher risk of artherosclerosis?
Sorry for all the compound questions, and if some or all of this will be addressed in later posts I’ll certainly be reading. Thanks Peter!
Jon, you’re correct that there is a strong correlation between particle size and particle number. In most cases, those with many particles have small particles. Plenty of exceptions, but this is the rule of thumb. My point this post was that there is nothing “special” about a small particle, in terms of atherogenic “ability.” In other words, 1,500 small LDL particles are no more or less harmful than 1,500 large particles. In part VI, which I’m writing now, this point will be made more clear, as will the superiority of LDL-P for predicting heart disease.
Unfortunately, my understanding of this topic was diminutive in 2009 when I began my “transformation,” so I do not know how bad my LDL-P was 3 years ago. I would not be surprised, given my other biomarkers, if I was north of 2,000 nmol/L, but I’m not willing to go back to my previous way of eating for 6 months to find out.
Well I certainly wouldn’t expect you to do that, given the risks you believe it would entail! Maybe you can ask this guy though!
https://gma.yahoo.com/video/wellness-29137617/drew-manning-goes-from-fit-2-fat-2-fit-29550692.html
Quite a transformation. Although, I do recall you saying in an interview I listened to that you may be moving out of ketosis for some self-experimentation regarding athletic performance this summer. Would be interested to know what impact that has on LDL-p. Regardless, looking forward to reading on and getting the rest of the info, thanks!
My doctor uses Spectracell, which gives me a breakdown of LDL particle counts. How does this compare with the NMR test, as far as validity? Is one better than the other?
Thanks.
Unfortunately not. If your doctor get get your blood to Liposcience, get an apoB direct measurement instead.
Spectracell uses ultracentrifugation with particle staining. It is a nonvalidated methodolgy – Do not use it. Get the NMR at any Labcorp
Just Adding my thanks for supplying such detailed and fascinating information. Much appreciated.
As an aside, I’ve heard another low carb, high fat proponent place particular importance on HbA1c levels, something I’m not overly familiar with. Is it a significant risk factor or does it pale in comparison to LDL-P? Is it likely that they’re not correlated in a non-diabetic person?
By the way, it seems that in Australia information on NMR is scarce. I’m pretty sure a few Universities have the equipment to do them, but as for being used for the general public – it doesn’t appear so. If anyone here has information to the contrary, I’d be interested to hear it.
I had an Apo B test done 5 years ago and I’m in the process of ordering another. Both times the docs were puzzled as to why I was requesting it – I presume because they knew very little about it. I’m crossing my fingers that I’m not one of the people whose Apo B increases with increased saturated fat intake. I’m loving my sausages and bacon too much to quit now.
Thanks again.
A1c measures the amount of glucose on hemoglobin molecules, which is a different issue. I’m not sure of the correlation between A1c and LDL-P, but I’m sure someone has analyzed. If you can’t get NMR from Liposcience, get measured apoB.
I’m in SF Bay area — East Bay side. Anyone know where to get an NMR? Is there a competent lab. Quest doesn’t do it. From your comments, Peter, it appears that LabCorp is not reliable. Kaiser doesn’t do it, but my cardiologist sent me a prescription. Anyone know?
Mike N. at 20, you are asking my question — what do we do? I’ve had one heart attack, six years ago. I know I have 40% blockage in my LAD. I take a statin, and I exercise. I’m thin. I limit my carbs to under 200 g daily — a moderate amount compared to the standard American diet. Suppose my NMR shows high LDL-P: what do I do?
Looking forward to further posts.
Lizzy, check this website for a potential lipidologist near you: https://www.lipidboard.org/lookup
Lizzy, You can order the LipoProfile NMR from Liposcience by ordering retail through Life Extension Foundation. They use LabCorp to collect your blood sample. I’m a Life Extension member and just got off the phone with their blood lab, and they confirmed that upon collection of your blood at Lab Corp, your specimen is sent to Liposcience. I called because yours was the second post I read that mentioned there was something funky with LabCorp.
Life Extension reports your results to you, although I always also get a report from Lab Corp.
The test is $98 for members and includes a lipid profile as well. It’s closer to $200 for non-members. The $75.00 membership is worth it to me just for the savings on labs because I always want to look at more stuff than a doc typically wants to order.
For others interested in this, if you are in NJ, NY, RI and MA, there’s some mess with prohibitions against third party billing, so you can’t pay Life Extension or any other retail provider of labs for blood work and then go to their contractor (Lab Corp etc) in those states. Most other retail providers (HealthcheckUSA/Directlabs etc) won’t even take customers from these 4 states, but Life Extension Foundation has a work around. I live right on the Delaware River, so I just go over the border to PA where it’s no problem even though I’m a NJ resident. Those residing in the 4 states mentioned and not close to a state without this prohibition have a little more complicated procedure to follow, but can still get this test and all their lab needs done thru Life Extension.
Here’s the link to the particle test thru Life Extension
https://www.lef.org/Vitamins-Supplements/ItemLC884247/NMR-LipoProfile-Blood-Test.html
directlabs.com ($129… no membership)… uses labcorp facilities.
Any LabCorp will do the NMR LipoProfile
Hi Dr. Peter,
I saw Dr. Dayspring’s lecture about why we should not be supplementing with phytosterols. There is a USA Today article out today linking calcium supplements with heart attacks. I have heard this before. Women are often advised to supplement calcium to avoid osteosporosis. Is this calcium depositing in our arteries as the “calcium score” previously discussed? Thank you very much, maryann
I’m not sure about the cause and effect mechanism of calcium supplementation.
Oh great –
The recommendation on calcium has been too high. Calcium and magnesium need to be in a ratio; at least as much cal as mag, but not more than twice as much. For example, if 400 mg mag, then at least 400 mg cal, but not more than 800 mg cal.
Also, cal is constricting, mag is relaxing; you need both, but not at the same time. Get cal from food or supps morning and/or afternoon, mag before bed.
Maryann, where did you see that lecture, on LECTUREPAD? Do you have the link?
Hi Claudia, The lecture is “Cholesterol Absorption and Synthesis Markers”. The entire 4-part lecture builds the foundation for the recommendation; but you can find the conclusion in lecture 4 beginning at slide 22. The body has a built-in mechanism to reject phytosterols and prevent their absorption. Some people are hyper-absorbers, in whom this natural defense system is not functioning. Supplementing with phytosterols in a person who hyperabsorbs results in very premature atherosclerosis. Before supplementing, a patient should be tested to see if they are vulnerable to hyper-absorption; however, the bottom line is that there is no data to suggest that phytosterols reduce CAD risk. (Plant stanols, however, are not absorbed and their use may be indicated.) The ubiquitous addition of phytosterols to food products, and the intentional consumption of supplements, is a risk factor for premature atherosclerosis in an unsuspecting population.
Thanks so much Maryann, ever so kind. I’ll have a look.
Take look at vitamin K2. It ultimately spurs the enzymes that carboxylate MGla and osteocalcin that direct the calcium and minerals to the right places. This may be a major factor in preventing heart disease and likely much more important than LDL-p.
I approve all comments, include those I don’t agree with. This is an example of one such comment. To say vit K is more important in preventing heart disease than lowering LDL-p is like saying the music choice on the Titanic was more important to saving lives than the lifeboats.
Maryann: I am impressed with your understanding of my sterol lecture. If you want to take it to the next level visit: https://www.biomarkerbliki.org/bliki-completed-chapters-noncholesterol-sterols-stanols-overview.html
Dr Lipid
I doubt it’s the most important factor but Stuart may have a point about K2 supplementation and coronary calcification…. consider:
Nutr Metab Cardiovasc Dis. 2009 Jan 27.
A high menaquinone reduces the incidence of coronary heart disease in women.
Gast GC, de Roos NM, Sluijs I, Bots ML, Beulens JW, Geleijnse JM, Witteman JC, Grobbee DE, Peeters PH, van der Schouw YT.
Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, The Netherlands; Department of Human Nutrition, Wageningen University, The Netherlands.
BACKGROUND AND AIM: Vitamin K dependent proteins have been demonstrated to inhibit vascular calcification. Data on the effect of vitamin K intake on coronary heart disease (CHD) risk, however, are scarce. OBJECTIVE: To examine the relationship between dietary vitamins K(1) and K(2) intake, and its subtypes, and the incidence of CHD. METHODS AND RESULTS: We used data from the Prospect-EPIC cohort consisting of 16,057 women, enrolled between 1993 and 1997 and aged 49-70 years, who were free of cardiovascular diseases at baseline. Intake of vitamin K and other nutrients was estimated with a food frequency questionnaire. Multivariate Cox proportional hazards models were used to analyse the data. RESULTS: After a mean+/-SD follow-up of 8.1+/-1.6 years, we identified 480 incident cases of CHD. Mean vitamin K(1) intake was 211.7+/-100.3mug/d and vitamin K(2) intake was 29.1+/-12.8mug/d. After adjustment for traditional risk factors and dietary factors, we observed an inverse association between vitamin K(2) and risk of CHD with a Hazard Ratio (HR) of 0.91 [95% CI 0.85-1.00] per 10mug/d vitamin K(2) intake. This association was mainly due to vitamin K(2) subtypes MK-7, MK-8 and MK-9. Vitamin K(1) intake was not significantly related to CHD. CONCLUSIONS: A high intake of menoquinones, especially MK-7, MK-8 and MK-9, could protect against CHD. However, more research is necessary to define optimal intake levels of vitamin K intake for the prevention of CHD.
PMID: 19179058
I think it’s time for folks to re-read the post: https://eatingacademy.com/nutrition/irisin-the-magic-exercise-hormone
Why? Because some folks seem to be forgetting about the concept of “ordered terms.” IF Vit K plays a role in this, it’s a higher-order. I realize folks like to quibble over this stuff, but let’s get the first- and second-order term right. Then we can debate the merits of the 9th- versus 11th-order terms.
Dear Dr. Dayspring,
Thank you so much! I have no science or math background, so if I understand anything at all it is due to your considerable skill as a teacher. I really enjoyed your lecture immensely and I thank you very much for the link you sent me. I also read “Understanding the Entire Lipid Profile” and learned a lot and enjoyed it. I am presently reading your “Moving Beyond LDL-C…” case report. If it is not too much trouble, could you please tell me what a half life is?
Would everyone benefit from taking Benecol; and is there a way to undo damage that may have occurred by mega doses of phytosterols?
When I finished your lecturepad series, I drew a conclusion and I am wondering if I extrapolated it correctly. Many people use the supplement Red Yeast Rice (1200mg twice per day)as a natural alternative to a statin. Since it acts like a statin in the body, I imagine that this would need to be monitored in the same way that you monitor statins; because in cases where the patient experiences increased absorption on a statin, monotherapy is inappropriate, and combination therapy would be needed. In the same way that phytosterol supplementation can range from innocuous to potentially dangerous, it seems that Red Yeast Rice supplementation might be also have the same potential to be harmful. Am I correct?
Thank you very much, Maryann
Isn’t arterial plaque mostly calcium? Vit K2 does a good job of directing calcium to the bones (with help from vits A and D) while preventing calcification of the arteries. Maybe you should read up on the topic before assigning such a low priority to K2 and calcium.
https://trabajos.cin2011.uninet.edu/379/fusaro.pdf
Sure plaques contain calcium, but reducing plasma levels of calcium is a very downstream way to address the problem. I’m not suggesting it wouldn’t be interesting to see a trial that compared LDL-P reduction alone vs. LDL-P reduction PLUS vit K, but my instinct tells me the addition of K2 would have a small impact, if any. Furthermore, I have never seen (which doesn’t mean anything other than me saying that) convincing data that K2 alone can reduce death from cardiovascular disease.
In your haste to provide a sarcastic comment (“Maybe you should read up on the topic…”), Peter-NZ, you’ve missed the point. The question isn’t whether people with heart disease have low levels of vit K, which some do. Nor is the question if supplementing vit K can increase osteoclast activity, which it obviously does. The question is, or should be, does giving vit K to someone reduce their risk of heart disease? If I’m missing the trial that has made this clear, please share it with me.
Here’s the problem with your logic, Peter-NZ. Let’s say you reduce the concentration of plasma calcium by 10%, is that preventing sufficient calcium from getting into the artery wall when all other factors are present? What about reducing the volume of circulating macrophages by 10% via plasmapheresis? Would that do the trick? I don’t know. The study hasn’t done. But the in medicine it’s very rare that minor alterations — and let’s be clear, that’s what you’re arguing for — of DOWNSTREAM factors can stop a problem of this magnitude. You’ve got to address the problem at the UPSTREAM driver.
While this analogy is not perfect, I could say the same thing about tuberculosis. These patients die from calcium-containing granulomas in their lungs and elsewhere in their body. What should we do to stop this? Reduce their calcium levels by 10 or 20%? It doesn’t help. The only treatment is killing the bacteria, mycobacterium tuberculosis, that CAUSES the problem to start.
Forgive me if I came across sarcastic, my comment suggesting you to familiarise yourself with K2 and CHD was not meant that way. Here is the study I base my argument on:
https://jn.nutrition.org/content/134/11/3100.full
Peter, I appreciate your apology. I am familiar with this study, but it does suffer the same problems many such studies suffer from. It is an observational study without intervention. In other words, we have no way of knowing if the differences they observed in the populations were CAUSED by differences in vit-K proteins, OR if that is just a correlation and a MARKER for some other cause.
Sometimes observational studies are helpful, especially for identifying problems that should be studied prospectively with controlled experiments. But typically, the “effect” is much larger. In this study the hazard ratios are quite small, suggesting *IF* vit K has anything to do with it, the effect is very small.
I’m not against this type of work for some questions, such as the role of smoking in lung cancer (where a study may be unethical) or LDL-P in heart disease (where the perfect experiment is metaphysically impossible – read Part VI of this series to see why), but a question like this could by addressed rigorously. And it should before we start over-dosing on vit K.
All of this said, I still stand 100% by my previous assertion and the analogy to tuberculosis. I do not believe the impact of vit K in most people is significant.
I hear you Peter but may I ask why you consider the RRs for the mid and top terciles (0.73/0.43 for CHD mortality and 0.71/0.48 for severe aortic calcification) to be insignificant?
On another topic, blood triglycerides are an independent risk factor for heart disease. Do you know how this fits in with your cholesterol theory (which is nicely put together)?
It’s less about the RR value and more about the idea that in observational studies, unless the RR is quite large, it’s very tough to draw conclusions. If this were a well controlled randomized experiment with perfect compliance, that would be a different story. Basically, the less control over the experiment, the greater demand you’d made on the RR to *suggest* (never prove) the association.
As far as TG go, it’s actually not clear they are an INDEPENDENT risk factor. In fact, many deep, deep, in the know would argue that once other variables are correct for, they are not. However, they are certainly a very strong predictor and marker of risk. The story fits perfectly, regardless of independent or dependent predictive power, though. More TG means less CE in apoB trafficking particles. Less CE per particle almost always points to…more particles to move the same amount of CE.
Cheers Peter. How muck stock do you put on trials with rats where K2 inhibit arterial calcification?
https://content.karger.com/ProdukteDB/produkte.asp?doi=10.1159/000075344
I hope everyone is reading this one. This is one of the few comments I write for everyone. It’s a good question, Peter, but here’s a better question: Ask yourself (this is a personal question, for which I can’t provide insight), which is bigger risk you take:
1. NOT taking vit K, assuming the results of this trial WOULD hold up as valid in well-controlled prospective randomized experiment? OR
2. Taking vit K, assuming the opposite?
In essence, this is the question EVERYONE should be asking themselves about ALL drug (or diet) therapy.
As a general question it’s a valid one but doesn’t really apply to me or even vit K. I get my K2 (MK-7)from natto and in Japan natto consumption, which varies by region, is associated with better regional CV health (I know, one can always say it’s something else). MK-4 is used there as a therapeutic tool in very large doses, 45 mg (not 45 mcg), per day to treat osteoporosis without ill effects. Vit K may be toxic to those who cannot process high doses (kidney patients, newborns) or those on blood thinners. I would worry more about overdosing on Vits A & D from pills. Incidentally, Vit D seems to manifest it’s toxicity by depleating Vit K which means high vit K(2) protects from vit D overdose.
Thanks, Peter. Appreciated.
Does anyone know how & where to get an apoB test in the UK, privately if possible (to avoid hassle of GP appointments)?
help peter iam totaly confused after years of trying to uderstand that ldl and total cholesteol doe not matter andthe most importiant is tg to be low hdl to be hi.
IAM EATING Hi fat mediam protien low carb
coconut oil lard ghee raw milk and meat all from grass feed animials and eggs 4 aday . I have had two stadard cholesterol test first one was tg 0.7 ldl 4.12 hdl 1.75 total 6.1 2 test tg 0.8 ldl 4.55 hdl 1.61 totol 7.5.HAVE i incress my heartdesease risk ijust finnished talling my doctor ldl does not matter after all th reserch that i have read. what am i doing wrong.
Drew, I’m helping as much as I can. I can’t really play doctor for everyone, on top of writing a blog 20 hours a week, on top of 2 full time jobs, on top of all other obligations. Sorry, man.
I am really grateful for your heroic efforts Peter. If you said you also had a part-time job as a Navy Seal…it wouldnt suprise me 🙂 I hope that you and your wife have some vacation time planned soon! Thank you so much, maryann
Can someone please provide a conversion factor for apoB? Here in Canada it is given in g/L rather than nmol/L — with the guidelines setting a target of <0.80g/L
Many thanks
80 gmL is 80 mg/dL which is the 20th percentile cutpoint. ApoB is not reported in molar concentration. It is a normal value. LDL-P is in nmol/L and LDL-P has nothing to do with apoB – apoB is a protein on LDL particles and LDL-P is a measurement of the entire particle. ApoB and LDL-P are two very different ways of counting LDL particle concentration
Thanks again for a very well written and explained article, Peter.
I do have one question: what is the value of ApoB for the highest risk quintile on that last picture? (if the study doesn’t show ApoB, then let us know the respective LDL-P and how we can convert between LDL-P and ApoB, please.)
I understand that absolute values only make sense within the conditions of the specific trial, but I’ve been looking to contextualize my ApoB counts and this looks like a good place to start.
I believe the top quintile in MESA was above 1,600 nmol/L, but if you dig through the paper you can find the exact number.
You cannot covert apoB to LDL-P but you can look at poopulation studies and see what the various equivalent cutpoints are: visit this website for the values in the Framingham Offspring Study
https://www.lipidcenter.com/pdf/Framingham.pdf
I don’t think I’ve ever felt like a blog post is taking an eternity to finish like this one. LOL Thanks for your great work!
If you think it takes an eternity to read…imagine how it feels to write.
I’m still not sold on the whole “concentration gradient is what drives ApoB-containing particles into the artery wall” idea.
Granted, you’ve shown us the studies that clearly show a positive correlation between ApoB particle number and CVD risk.
But I think that this is not enough information and that it is perfectly possible to have some very serious confounding factors that obscure these clinical and observational trials.
Beating the not-so-dead horse again, I believe that infection has a lot more bearing on the subject than you’re willing to believe.
Reading the definition of the Chronic endothelial injury hypothesis, it becomes clear how common lifelong infections like Helicobacter Pylori (extremely common in the carb-munching western population) can slowly but cumulatively chip away our endothelial surface, exposing us to higher CVD risk. And they don’t even have to be clinically detectable – most of us have more pathogenic bacteria than we should in our digestive tracts, and yet we carry on blissfully ignorant of the fact.
There was even a study that proved that eradication of bacterial infection restores endothelial function.
This whole picture (pathogens releasing toxins in blood that disrupt endothelial cell function allowing ApoB carrying particles to penetrate artery wall) makes a lot more sense to me than just “there’s so many particles that they just pierce the wall”. Unless you assume that LDLs burrowing into the artery wall is something that is quite natural to happen all the time. From an evolutionary point of view, I find that extremely hard (improbable) to swallow.
You mention your using HDL labs for NMR test and some other tests. What other tests would make sense besides NMR. Thanks.
I will, in a subsequent post, review the labs done by HDL. You’ll get a sense of what is out there and how it can enable better decision making.
Love your work and appretiate it more than you know. You’ll still get to the role omega-3/6 have in all of this?
Yes, that series is on the list, also. Hopefully it won’t be as long as this one.
If the endothelial layer is healthy and strong the particles won’t penetrate.
I don’t know if this is true. I think a healthy endothelial layer is less likely to be penetrated, but if the gradient of particles is high enough, I don’t know that none get across.
“If the endothelial layer is healthy and strong the particles won’t penetrate.”
Now THAT is something worth investigating. 🙂
Does anyone have any hard info on this?
You do not have to have endothelial dysfunction for apoB particles to penetrate. However once they do the maladaptive inflammatory process poccurs and endothelial dysfunction soonfollows the apoB invasion