Want to catch up with other articles from this series?
- The straight dope on cholesterol – Part I
- The straight dope on cholesterol – Part II
- The straight dope on cholesterol – Part III
- The straight dope on cholesterol – Part IV
- The straight dope on cholesterol – Part V
- The straight dope on cholesterol – Part VI
- The straight dope on cholesterol – Part VII
- The straight dope on cholesterol – Part VIII
- The straight dope on cholesterol – Part IX
I’ve been planning to write at length about this topic for a few months, but I’ve been hesitant to do so for several reasons:
- To discuss it properly requires great care and attention (mine and yours, respectively).
- My own education on this topic only really began about 9 months ago, and I’m still learning from my mentors at a geometric pace.
- This topic can’t be covered in one post, even a Peter-Attia-who-can’t-seem-to-say-anything-under-2,000-word post.
- I feel a bit like an imposter writing about lipidology because my mentors on this topic (below) have already addressed this topic so well, I’m not sure I have anything to add.
But here’s the thing. I am absolutely – perhaps pathologically – obsessed with lipidology, the science and study of lipids. Furthermore, I’m getting countless questions from you on this topic. Hence, despite my reservations above, I’m going to give this a shot.
A few thoughts before we begin.
- I’m not even going to attempt to cover this topic entirely in this post, so please hold off on asking questions beyond the scope of this post.
- Please resist the urge to send me your cholesterol numbers. I get about 30 such requests per day, and I cannot practice medicine over the internet. By all means, share your story with me and others, but understand that I can’t really comment other than to say what I pretty much say to everyone: standard cholesterol testing (including VAP) is largely irrelevant and you should have a lipoprotein analysis using NMR spectroscopy (if you don’t know what I mean by this, that’s ok… you will soon).
- This topic bears an upsettingly parallel reality to that of nutrition “science” in that virtually all health care providers have no understanding of it and seem to only reiterate conventional wisdom (e.g., “LDL is bad,” “HDL is good”). We’ll be blowing the doors off this fallacious logic.
By the end of this series, should you choose to internalize this content (and pick up a few homework assignments along the way), you will understand the field of lipidology and advanced lipid testing better than 95% of physicians in the United States. I am not being hyperbolic.
One last thing before jumping in: Everything I have learned and continue to learn on this topic has been patiently taught to me by the words and writings of my mentors on this subject: Dr. Tom Dayspring, Dr. Tara Dall, Dr. Bill Cromwell, and Dr. James Otvos. I am eternally in their debt and see it as my duty to pass this information on to everyone interested.
Are you ready to start an exciting journey?
Concept #1 – What is cholesterol?
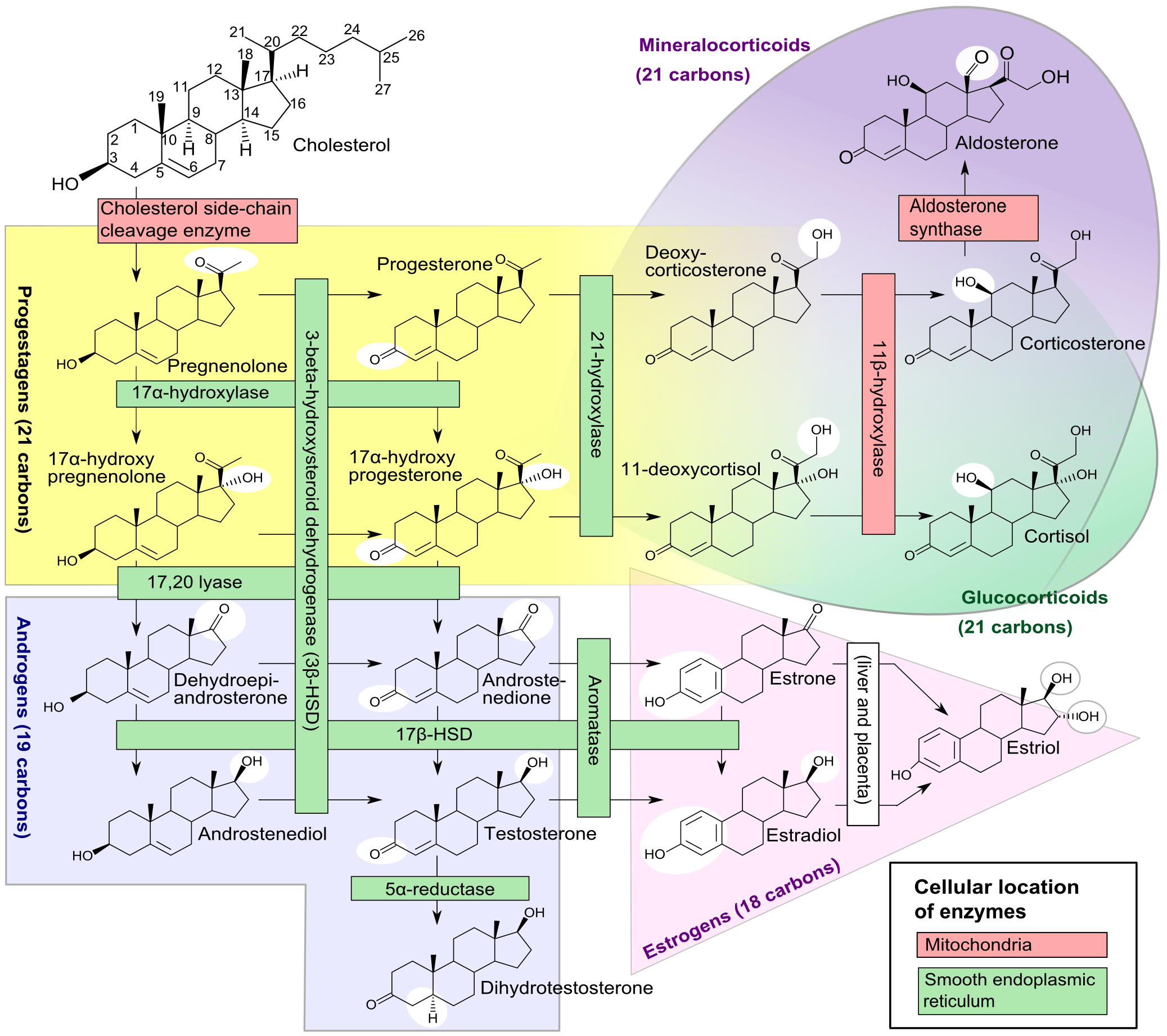
Cholesterol is a 27-carbon molecule shown in the figure below. Each line in this figure represents a bond between two carbon atoms. Sorry, I’ve got to get it out there. That’s it. Mystery over.
All this talk about “cholesterol” and most people don’t actually know what it is. So there you have it. Cholesterol is “just” another organic molecule in our body.
I need to make one important distinction that will be very important later. Cholesterol, a steroid alcohol, can be “free” or “unesterified” (“UC” as we say, which stands for unesterified cholesterol) which is its active form, or it can exist in its “esterified” or storage form which we call a cholesterol ester (“CE”). The diagram above shows a free (i.e., UC) molecule of cholesterol. An esterified variant (i.e., CE) would have an “attachment” where the arrow is pointing to the hydroxyl group on carbon #3, aptly named the “esterification site.”
Since cholesterol can only be produced by organisms in the Animal Kingdom it is termed a zoosterol. In a subsequent post I will write about a cousin of cholesterol called phytosterol, but at this time I think the introduction would only confuse matters. So, if you have a question about phytosterols, please hang on.
Concept #2 – What is the relationship between the cholesterol we eat and the cholesterol in our body?
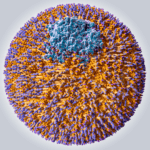
We ingest (i.e., take in) cholesterol in many of the foods we eat and our body produces (“synthesizes”) cholesterol de novo from various precursors. About 25% of our daily “intake” of cholesterol – roughly 300 to 500 mg — comes from what we eat (called exogenous cholesterol), and the remaining 75% of our “intake” of cholesterol — roughly 800 to 1,200 mg – is made by our body (called endogenous production). To put these amounts in context, consider that total body stores of cholesterol are about 30 to 40 gm (i.e., 30,000 to 40,000 mg) and most of this resides within our cell membranes. Every cell in the body can produce cholesterol and thus very few cells actually require a delivery of cholesterol. Cholesterol is required by all cell membranes and to produce steroid hormones and bile acids.
Of this “made” or “synthesized” cholesterol, our liver synthesizes about 20% of it and the remaining 80% is synthesized by other cells in our bodies. The synthesis of cholesterol is a complex four-step process (with 37 individual steps) that I will not cover here (though I will revisit), but I want to point out how tightly regulated this process is, with multiple feedback loops. In other words, the body works very hard (and very “smart”) to ensure cellular cholesterol levels are within a pretty narrow band (the overall process is called cholesterol homeostasis). Excess cellular cholesterol will crystalize and cause cellular apoptosis (programmed cell death). Plasma cholesterol levels (which is what clinicians measure with standard cholesterol tests) often have little to do with cellular cholesterol, especially artery cholesterol, which is what we really care about. For example, when cholesterol intake is decreased, the body will synthesize more cholesterol and/or absorb (i.e., recycle) more cholesterol from our gut. The way our body absorbs cholesterol is so amazing, so I want to spend a bit of time discussing it.
In medical school, whenever we had to study physiology or pathology I always had a tendency to want to anthropomorphize everything. It’s just how my brain works, I guess, and understanding cholesterol absorption is a great example of this sort of thinking. The figure below, from the Gastroenterology Journal, shows a cross-section of a cell in our small intestine (i.e., our “gut”) called an enterocyte that governs how stuff in our gut actually gets absorbed. The left side with the fuzzy border is the side facing the “lumen” (the inside of the “tube” that makes up our gut). You’ll notice two circles on that side of the cell, a blue one and a pink one.
[What follows is a bit more technical than I would have liked, but I think it’s very important to understand how this process of cholesterol absorption works. It’s certainly worth reading this a few times to make sure it sinks in.]
- The blue circle represents something called a Niemann-Pick C1-like 1 protein (NPC1L1). It sits at the apical surface of enterocytes and it promotes active influx (i.e., bringing in) of gut luminal unesterified cholesterol (UC) as well as unesterified phytosterols into the enterocyte. Think of this NPC1L1 as the ticket-taker at the door of the bar (where the enterocyte is the “bar”); he lets most cholesterol (“people”) in. However, NPC1L1 cannot distinguish between cholesterol (“good people”) and phytosterol (“bad people” – I will discuss these guys later, so no need to worry about it now) or even too much cholesterol (“too many people”). [I can’t take any credit for this anthropomorphization – this is how Tom Dayspring explained it to me!]
- The pink circle represents an adenosine triphosphate (ATP)-binding cassette (ABC) transporters ABCG5 and ABCG8. This complex promotes active efflux (i.e., kicking out) of unesterified sterols (cholesterol and plant sterols – of which over 40 exist) from enterocytes back into the intestinal lumen for excretion. Think of ABCG5,G8 as the bouncer at the bar; he gets rid of the really bad people (e.g., phytosterols as they serve no purpose in humans) you don’t want in the bar who snuck past the ticket-taker (NPC1L1). Of course in cases of hyperabsorption (i.e., in cases where the gut absorbs too much of a good thing) they can also efflux out un-needed cholesterol. Along this analogy, once too many “good people” get in the bar, fire laws are violated and some have to go. The enterocyte has “sterol-excess sensors” (a nuclear transcription factor called LXR) that do the monitoring and these sensors activate the genes that regulate NPC1L1 and ABCG5,G8).
There is another nuance to this, which is where the CE versus UC distinction comes in:
- Only free or unesterified cholesterol (UC) can be absorbed through gut enterocytes. In other words, cholesterol esters (CE) cannot be absorbed because of the bulky side chains they carry.
- Much (> 50%) of the cholesterol we ingest from food is esterified (CE), hence we don’t actually absorb much, if any, exogenous cholesterol (i.e., cholesterol in food). CE can be de-esterified by pancreatic lipases and esterolases – enzymes that break off the side branches and render CE back to UC — so some ingested CE can be converted to UC.
- Furthermore, most of the unesterified cholesterol (UC) in our gut (on the order of about 85%) is actually of endogenous origin (meaning it was synthesized in bodily cells and returned to the liver), which ends up in the gut via biliary secretion and ultimately gets re-absorbed by the gut enterocyte. The liver is only able to efflux (send out via bile into the gut) UC, but not CE, from hepatocytes (liver cells) to the biliary system. Liver CE cannot be excreted into bile. So, if the liver is going to excrete CE into bile and ultimately the gut, it needs to de-esterify it using enzymes called cholesterol esterolases which can convert liver CE to UC.
- Also realize that the number one way for the liver to rid itself of cholesterol is to convert the cholesterol into a bile acid, efflux that to the bile (via a transporter called ABCB11) and excrete the bile acids in the stool (typically most bile acids are reabsorbed at the ileum).
Concept #3 – Is cholesterol bad?
One of the biggest misconceptions out there (maybe second only to the idea that eating fat makes you fat) is that cholesterol is “bad.” This could not be further from the truth. Cholesterol is very good! In fact, there are (fortunately rare) genetic disorders in which people cannot properly synthesize cholesterol. Once such disease is Smith-Lemli-Opitz syndrome (also called “SLOS,” or 7-dehydrocholesterol reductase deficiency) which is a metabolic and congenital disorder leading to a number of problems including autism, mental retardation, lack of muscle, and many others.
Cholesterol is absolutely vital for our existence. Let me repeat: Cholesterol is absolutely vital for our existence. Every cell in our body is surrounded by a membrane. These membranes are largely responsible for fluidity and permeability, which essentially control how a cell moves, how it interacts with other cells, and how it transports “important” things in and out. Cholesterol is one of the main building blocks used to make cell membranes (in particular, the ever-important “lipid bilayer” of the cell membrane).
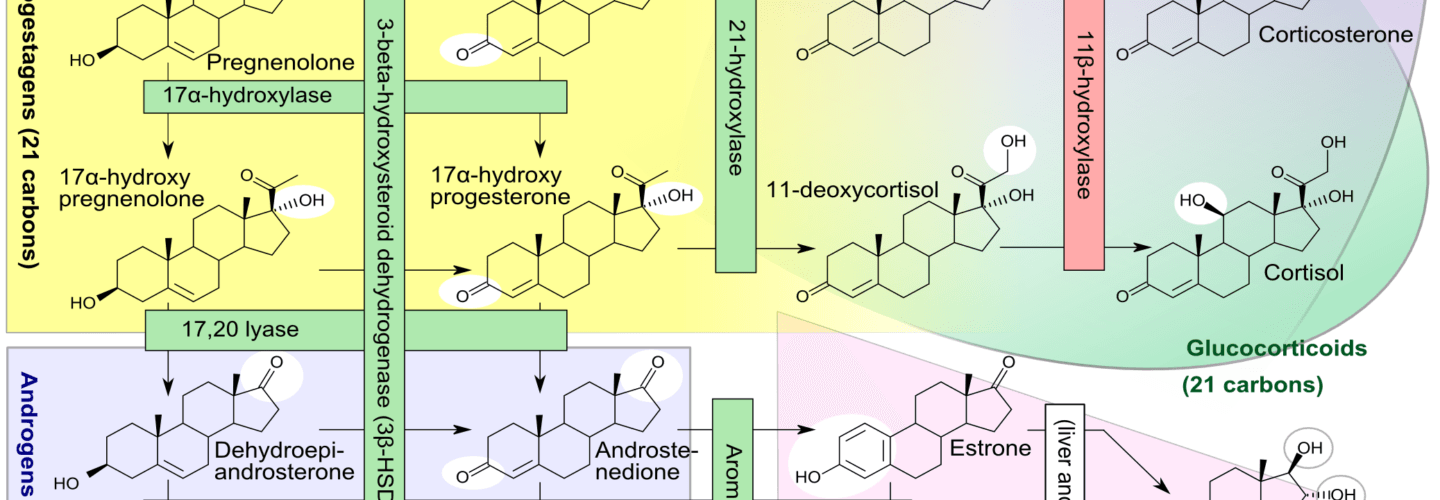
Beyond cholesterol’s role in allowing cells to even exist, it also serves an important role in the synthesis of vitamins and steroid hormones, including sex hormones and bile acids. Make sure you take a look at the picture of steroid hormones synthesis and compare it to that of cholesterol (above). If this comparison doesn’t convince you of the vital importance of cholesterol, nothing I say will.
One of the unfortunate results of the eternal need to simplify everything is that we (i.e., the medical establishment) have done the public a disservice by failing to communicate that there is no such thing as “bad” cholesterol or “good” cholesterol. All cholesterol is good!
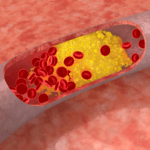
The only “bad” outcome is when cholesterol ends up inside of the wall of an artery, most famously the inside of a coronary artery or a carotid artery, AND leads to an inflammatory cascade which results in the obstruction of that artery (make sure you check out the pictures in the links, above). When one measures cholesterol in the blood – we really do not know the final destination of those cholesterol molecules!
And that’s where we’ll pick it up next time – how does “good” cholesterol end up in places it doesn’t belong and cause “bad” problems? If anyone is looking for a little extra understanding on this topic, please, please, please check out my absolute favorite reference for all of my cholesterol needs, LecturePad. It’s designed primarily for physicians, but I suspect many of you out there will find it helpful, if not now, certainly once we’re done with this series.
To summarize this somewhat complex issue
- Cholesterol is “just” another fancy organic molecule in our body, but with an interesting distinction: we eat it, we make it, we store it, and we excrete it – all in different amounts.
- The pool of cholesterol in our body is essential for life. No cholesterol = no life.
- Cholesterol exists in 2 forms – UC and CE – and the form determines if we can absorb it or not, or store it or not (among other things).
- Most of the cholesterol we eat is not absorbed and is excreted by our gut (i.e., leaves our body in stool). The reason is it not only has to be de-esterified, but it competes for absorption with the vastly larger amounts of UC supplied by the biliary route.
- Re-absorption of the cholesterol we synthesize in our body is the dominant source of the cholesterol in our body. That is, most of the cholesterol in our body was made by our body.
- The process of regulating cholesterol is very complex and multifaceted with multiple layers of control. I’ve only touched on the absorption side, but the synthesis side is also complex and highly regulated. You will discover that synthesis and absorption are very interrelated.
- Eating cholesterol has very little impact on the cholesterol levels in your body. This is a fact, not my opinion. Anyone who tells you different is, at best, ignorant of this topic. At worst, they are a deliberate charlatan. Years ago the Canadian Guidelines removed the limitation of dietary cholesterol. The rest of the world, especially the United States, needs to catch up.



I look forward to every new post on your blog, keep up this great work, u are a dynamo, how do u find the time?
Thank you so much for this great blog!
You said “Certainly possible with the right nutrient mix, but requires more attention.”
I am interested in some detail on the right nutrient mix for adding muscle mass. I hope you plan to address this in a post.
First, thank you for this incredible service. Really helpful.
Request: A major punchline here is the proportion of circulating cholesterol derived from the diet. You’ve got the numbers but it’s left to the reader to stitch them together (for example, 25% of cholesterol is exogenous, but then >50% of that is esterified and not absorbed, thus <12.5% of the cholesterol used by the body is derived from diet, which is similar to, perhaps the same number as, the 15% exogenous UC which is the complement of the 85% endogenous you cite…). A picture would be helpful; I'm imagining arrows of various thicknesses going from diet, liver, etc. into the gut and then into circulation, cells, etc.
On a related note: it would be nice, if the data are known, to know the relationship between change in cholesterol intake and change in circulating cholesterol. That is, if one quadruples the amount of cholesterol one eats, what is the effect on cholesterol in the body? The naive notion would be "it quadruples"; the prediction from cholesterol being tightly regulated would be "it does not change". Has such a study been done?
Allan, for some people, LDL cholesterol and LDL-P can go up markedly on a high fat low carb diet, particularly with consumption of large amounts of saturated fat and dietary cholesterol. This effect is unpredictable and could be limited to people who have genetic mutations in intestinal transporter genes – we really don’t know. Some people think it is related to ApoE status. The only way to know is to draw measurements before and after diet. This was true of my case, in which low carb / high fat normalized by triglyercides, HDL and hs CRP, but radically increased my total and LDL cholesterol (I am still waiting for the LDL-P to come back from the lab). The result is that I had to cut down on my dietary fat consumption, switching more to lean proteins, and start taking a statin. Even to begin with, my LDL was a bit on the high side, but nothing like it was after the diet. So to say there is no relationship between the cholesterol or fat in the diet and the cholesterol (or fat) in the blood is really a stretch….
Note I’ve seen this phenomenon in others too, and it has been amply documented in the literature since the 1940’s.
Thank you so much for all of your hard work Peter! For the first time ever, I will miss not having my computer on vacation! I will be reading for hours when I get back.
Thank you to all who post comments, too. It is nice to have a thoughtful, enthusiastic, eager-to-learn community of like-minded people to exchange ideas with, and such a one-of-a-kind teacher in charge of it all.
We have taken Red Yeast Rice, phytosterols and sytrinol to lower our cholesterol. Are these things harmful?
Great post Peter, I look forward to the continuation of the series, thank you! Maryann
No role for phytosterols whatsoever. I’ll address this at a later time.
Can you add a print button to your blog so I could print this post and read it on the bus? I spend too much time in front of a computer screen already. IMO all blogs should be printer friendly.
Why not just copy it into WORD and print from there?
Tara Dall’s video series on Lecturepad was beyond impressive. Thanks for the lead.
Hi:
If it is LDL particles being lodged in the artery wall and the cholesterol in the LDL particle that then causes a plaque( along with other things) would having less cholesterol in the LDL particle be beneficial? Seems to me not from the info you have provided above, and yet many Lipidologists continue to stress avoidance of saturated fat(raises cholesterol in their view)and emphasize mono and poly fats.
Where do your mentors Dayspring, Dall, Cromwell, etc stand on the diet recommendations? They may all agree with less carbs, but on the type of fat?
Also, what is the best strategy for reversing coronary plaque, with diet and what resulting NMR profile- How low must particles be? Thanks.
Patience, Steve…. If I answer every (great) question being asked that is beyond the scope of THIS post, I’ll have to quit my job, divorce my wife, and take up a nasty cocaine habit. And I still won’t have enough time.
wouldn’t want you to do any of that; nor would i want you to neglect your kids,if you have them! Thanks.
Thanks for understanding.
lol!
RE the question of where do Drs. Dayspring, Dall, et al, stand on dietary recommendations; I was surprised to find on Tara Dall’s site a testimonial from a patient stating that Dr. Dall advised removal of red meat from the diet. Can you comment on this subject yet?
I can’t really speak for her. It’s quite likely that just as my understanding of lipoproteins is evolving, so too is Dr. Dall’s understanding of nutrition. They may not represent her current views.
Hi Peter,
I’m curious about statins. It seems bizarre how popular they are, given the information above.
Anna
Statins are great drugs, IF they are used to treat the right problem. I’ll get into this later in the series. Think of statins like a hammer — great for hammering nails; lousy for cleaning your window.
“Think of statins like a hammer — great for hammering nails; lousy for cleaning your window.”
Just keep it up, you’ll have us all understanding this in no time.
Peter, thank you so much for this website. Like many women, I have dieted since my first child ( yes, a long time ago!). My husband found Gary Taubes and it lead me to your website. I am on my 31st day of ketosis and very energetic and happy!! I feel amazing and ummmm…according to me, starting to look good as well! I have devoured this website and think I am caught up on my reading and the rest of the gang! Thank you! Thank you!
Thank you. Glad you’re finding it helpful.
A little off-topic, but I was wondering if you had an opinion on the necessity (or lack thereof) of taking a CoQ10 supplement along with statins. I’ve read that statins can deplete CoQ10 and that supplementation might help with potential side effects but haven’t seen a whole lot written about it by people who seem to really understand lipidology.
James, sorry to do this, but I need to quote, directly from the post, not just because of your question, but because so many others have missed my request: “I’m not even going to attempt to cover this topic entirely in this post, so please hold off on asking questions beyond the scope of this post.”
I will address this in the future.
Completely fair. I had searched for any other posts where you might have mentioned it to see if there was somewhere more appropriate to ask that question. Knowing that it’s on your radar is sufficient for me at this point.
No problem. Thanks for your patience.
Interesting. Keep up the good work!
Hi Peter,
Does the NMR reflect just a snapsot of what is happening in the body at the time? Or is it the picture of years of the body’s state of health? And can lipid testing be affected by exercise? Should exercising be avoided the morning of blood work to ensure accurate results? Thanks, Maryann
NMR, per se, reflects what’s going at a moment in time, but of course it’s highly dependent on what’s BEEN going on up to that point. Nothing is really static.
Coincidentally, reading this chapter in “Good Calories Bad Calories” right now. I just finished reading “Real Food” by Nina Planck where she draws this picture: Where you see a fire, you’ll probably see firemen. Blaming cholesterol for Atherosclerosis is like blaming the firemen for starting the fire.
I believe the internet will be the new tool for mass re-indoctrination on the health front. Unfortunately, I couldn’t get most of my friends and family to read and digest this article without a fantastic infographic.
“The only “bad” outcome is when cholesterol ends up inside of the wall of an artery, most famously the inside of a coronary artery or a carotid artery, AND leads to an inflammatory cascade which results in the obstruction of that artery (make sure you check out the pictures in the links, above).”
Really good point and might be analogous to the idea that there’s always an “excess” of nutrients sitting outside cells (something Craig Thompson at Sloan-Kettering pointed out in a paper in Science), but cells won’t take them up unless they are told to (like insulin and glucose). The mere presence of “too much” of a substance in the blood stream isn’t really the issue. There is almost always an “excess” of fat, cholesterol, and nutrients in the body.
You are not what you eat; you are what you do with what you eat. The same can be applied to the different molecules and compounds inside and outside of cells.
Exactly. Worth re-stating: You are not WHAT you eat…You are what your body DOES with what you eat.
Absolutely FANTASTIC explanation! Most useful blog on ketosis and general health I’m following so far, keep up the good work!
It begins…
https://www.carolinajournal.com/exclusives/display_exclusive.html?id=8992
Everyone who cares about the freedom of people like Peter to continue to do what they do needs to read this.
Very scary, this guy lives close by me here in NC.
Thank you so much Peter for your work and sharing with us. I like so many others are eternally greatful that you are taking the time to supply this information. I am learning much more about the human body than I ever thought I would.
It truly is disappointing that cholesterol has been made out as a bad actor in our minds. I like so many others, before I discovered low carb thought it (cholesterol) was something to be scared of. So refreshing to actually learn.
I made a comment that I started VLC eating in March and have dropped 23 pounds since then, your reply was to keep up the work, Peter eating VLC is NOT work. It’s a joy to finally eat what I have always enjoyed eating and it’s a joy to stop eating so much sugar and grain. I feel fantastic. The only work is getting over my anger at the medical community and US government for not looking into this “alternative” way of eating.
Thank you again
Really glad to hear, Mark. Keep up the “pleasure!”
Thanks for the clear and informative post and for all your hard work in ths area, you are delivering an amazing public service as these posts are shared on many other sites. Look forward to the rest of the series.
SKYROCKETING LDL-P(as measured by Apo-B) on a VLC diet:
Your post is extremely timely for me because I just learned last week that my LDL and Apo-B (my particles are large) has SKYROCKETED on a LC diet (not ketogenic, prob 100g day in non starchy vegetables), and from the comments here I am probably in the very small minority but certainly not alone. PLEASE if you share this same experience, contact me and let’s share notes. I will attempt to contact Dan who also posted on this. 2 months into my LC diet, I had my best numbers ever… 200 TC, 120 LDL, good HDL and TG (which was 60 points less than before the LC diet, as way of reference). My LDL-C is now 300, and TC is 400. ApoB of 200 suggests I have 2x the number of particles that they use as a cutoff. This is way higher than when I was fat!
The interesting thing is that low carbing clearly has helped me in almost all measures except my Apo-B/ LDL-C. My weight, blood pressure, energy levels, HDL, Triglycerides… all improved. My CRP after 3 months of LC was barely measurable. My LDL levels initially responded the way that is predicted by most Low Carb diet trials. HDL up significantly, TG way down, and LDL flattish… in fact, my LDL improved a bit at one point. All this news came at the same time with Gary Taubes life changing book, so it was self reinforcing.
I’ve been low carb for almost exactly 1 year… completely transformed my body in a positive way, but this LDL phenomenon is a MAJOR wakeup call that maybe I shouldn’t be as zealous as I have been advocating low carb.
My 3 avenues for follow up (as of now) are:
1) Thyroid hormone. There has been some chatter in LC circles that LC can reduce Thyroid, or specificially TSH to T3 conversion and increase in reverse T3. I havent explored this in depth, but a first pass google search reveals that T3 is related to LDL receptor activity. Since Familial Hyperchosteremia is a result of poor LDL receptor function, clearly, a down-regulation in LDL receptor activity would increase plasma levels of LDL-C and presumably LDL-P. But can changes in thyroid hormone explain that much a change in LDL? I wish there was some clinical data accessible about that. Peter- I hope you address this in your next post.
I also recall from somewhere that LDL receptor activity may be influenced by insulin levels. There is also the potential and paradoxical issue of INCREASED INSULIN RESISTANCE on a low carb diet, as your body becomes more insulin resistant in an attempt to conserve glucose levels for the brain. I thought one extremely interesting clinical application from Dr Dall’s lecture was the use of Metformin to cut LDL-P by almost 50% in one case. Peter, if you get a moment to comment on what mechanism might be at work there, it would be helpful, but I’m guessing it would have something to do with insulin signaling and probably related to LDL receptor activity.
So I had my first sweet potato last night, and a little bit of rice… I didn’t like the fact that my glucose level shot up from 95 to 140 in the first hour but perhaps that’s another sign that my insulin sensitivity has gotten worse since going on LC. Perhaps it’s just a little TOO LC.
2) Gut absorption. Perhaps I’m an over absorber. I hate to go into this level of detail but one downside of LC has been changes in bowel movement patterns. Maybe something has changed the efflux/influx ratio of cholesterol from bile since I went low carb. One thing that Dr Dayspring mentioned was to check lathosterol/desmosterol because that gives some indication whether you are producing too much or absorbing too much.
3) Dietary fat. This seems less likely, but there are classes of saturated fats that seem to raise blood cholesterol levels differently, and dairy is high in palmitate. Seems unlikely but I didn’t eat a lot of dairy a year ago and my cholesterol was a lot lower so I’ll give that a try.
FINALLY, WHAT ARE THE REAL CLINICAL IMPLICATIONS AND WHO ELSE FALLS INTO THIS CATEGORY?
Yes, there is a clear association between LDL-C, LDL-P and atherogenesis. And LDL-P appears to be a stronger association than LDP-C. But if there is no inflammatory cascade, is it a problem to have high LDL-P? How does this risk factor stack up against other risk factors such as high Blood Pressure, Increased adiposity, etc? One thing that doesn’t seem to make a lot of sense to me is that if you have 1000 particles its OK, but somehow at 2000 you are going to get atherosclerosis? One particle is ok but 2 isnt? Plus, even with these risk associations, it seems as if there are plenty of people with high LDL-P that don’t get CVD and some people with Low LDL-P that do. Maybe I’m wrong… maybe everyone with high LDL-P has atherosclerosis but no measured CVD event. Peter can you elaborate?
Any other patients out there with a similar experience? Lets share data. [email protected]. One frustration I have from reading studies is that the numbers are always shown in averages. We are not averages.
NMR vs VAP vs Standard Lipid PaneI:
I totally understand your bias for getting particle counts which is much better than knowing the amount of serum cholesterol. You are measuring smoke, not the fire. But why would you consider the VAP panel inferior to NMR? You get an Apo-B stat out of a VAP Panel, and as I understand it, LDL particles only have 1 Apo-B molecule, so that essentially gives you a particle count. I know that Chylomicrons, VLDL, IDL also have 1 Apo-B per particle as well, so there could be some discrepancies if the ratio of those other Apo-B particles to LDL changes (as Dr Dall alluded to in her clinical application talk on LecturePad). I know VAP provides an estimated Apo-B, and perhaps the estimation correlations are poor, but assuming their Apo-B numbers are good, one would think this would be just as useful as an LDL-P stat. From what I have read, all Apo-B particles could have some atherogenic qualities, so wouldn’t you want to know stats for these other classes of lipoproteins? Plus, wouldn’t you want to see the various levels of Lipoprotein subclasses to give a window into how these lipoproteins are being metabolized/catabolized in your body? When I see an NMR panel, it doesn’t seem to show anything about these other subclasses or particles.
VAP estimates apoB, which is known to have mistakes. Furthermore, there are examples of apoB – LDL-P discordance. The NMR test is so simple. There is little need to avoid it.
Completely agree with your point. We are not averages!
I thought from reading Taubes’ Good Calories Bad Calories, that LDL-C was only very weakly correlated with atherosclerosis and heart disease risk — so I’m not sure why you’re saying that there is a clear association between LDL-C and atherosclerosis. Your triglycerides, HDL, and VAP/NMR are much more important measures. If everything else is going well, why get hung up over a number? I don’t this is an indication that you’re going too low carb at all!
Ed, On your low carb and thyroid issue, this has come up for me again just yesterday, after listening to a podcast at Jimmy Moore’s featuring Chris Kresser who spoke on this very issue. Here’s a copy of my comment on that podcast posted below.
“As a thyroid patient, struggling with all the issues that thyroid patients struggle with, I had been aware of, and concerned by, the reduced T3/increased rT3 levels associated with carbohydrate restricted and calorie restricted diets. I read a lot of the literature, including the old stuff from way back in the 50’s and a couple of textbooks, and while it confirms the changes in the levels of the hormones with carb/calorie restriction, generally it appears that resting energy expenditure only decreases on severely restricted caloric diets. So, are the changes in T3 and rT3 levels really clinically significant; ie, do the changes in the levels mean that thyroid function itself is harmed by carbohydrate restriction? A discussion of this question appears in a 2004 paper by Wolfgang Kopp in the journal Medical Hypotheses in which the author reviews the literature on the topic and indicates that, “The sharp decline in T3 levels as a result of very low carbohydrate diets is not associated with a reduction in the resting oxygen uptake, or symptoms of functional hypothyroidism (cold intolerance, dry skin, increased need for sleep). Despite decreased T3 concentrations, basal TSH levels are normal or even mildly decreased. The lack of clinical symptoms, together with normal or mildly decreased TSH levels suggest that the organism does not suffer from a deprivation in thyroid hormone in association with carbohydrate restriction.” His rationale is that our modern “normal” levels of T3 may be quite higher than our paleo ancestors exactly because of the carbohydrate load of modern diets. He concludes that “the metabolism of dietary carbohydrate is a thyroid hormone consuming process.” I really liked this guest and felt he had a great command of the thyroid and how it works. However, I felt he implied that carb restricted diets decrease thyroid function (not just thyroid hormone levels), sort of like you should watch out that if you carb restrict and lower your insulin levels that you won’t be able to convert T4 to T3, and you’ll go down this metabolic dead end with production of rT3. It appears there is a reasonable argument to be made that in the carb restricted state, you don’t need as much T3, and that this lower level of thyroid hormone is more aligned with that of our paleo ancestors.”
I see that there is another interview that Chris Kresser does on his website with Chris Masterjohn that gets into some of this, which I have not yet listened to, so who knows if there’s a wider perspective that I lack.
Lorraine-
Thanks for your comment! The internet is a great community and helps provide better suggestions or ideas than my own doctor.
Thanks to the power of google, and my sudden fascination on the subject, I managed to find that very same interview and listened to it on my commute to work. So my Thyroid testing panel is definitely on my “TO DO LIST”.
Another post I found which very topical to the SOARING LDL-C/LDL-P/Apo-B vs Thyroid discussion is here on Paul Jaminet’s website. https://perfecthealthdiet.com/?p=4457
Anyone worried with soaring LDL as a result of low carb should take a look at that one, too. Now what’s great about this is that it has a personal story chronicled by someone with this exact issue, that has kept clinical records of his “self-experimentation”. His TC went from 250 to 360 back to 200 very quickly with T3 supplementation. Now I know his data doesnt include the NMR or VAP results, but I think it gives a good ideas of the magnitudes of changes that can be involved if this is the root cause.
There obviously is a much broader question here, and perhaps Peter is going to address this in his next post. Should we care about LDL-C, LDL-P at all? For example, if T3 is causing LDL receptor activity to diminish, and LDL-P and LDL-C rise dramatically as a result, does this imply more CVD risk, if all other biomarkers associated as risk factors such as HDL, TG, Blood Pressure, HbA1C, weight are improved?
I will be addressing this, but not this week. LOTS to learn before we can have that discussion. This week will cover cholesterol transport.
Anu-
I agree that LDL-C is probably a weaker association with atherosclerosis than those other measures. In fact, I thought a very funny study recently came out that surveyed hospitals and CVD events over the last 5 years and showed that average LDL-C for those patients were BELOW national averages. But I have seen enough epidemiological data (including those in Asia, as I am of asian descent) that suggest that CVD is more common in those with higher levels of LDL-C. Should we fixate on LDL-C, LDL-P? No, I doubt it, and perhaps Peter will shed more light on this in his next post, but I think a very elevated level (above 95th percentile according to Dr Dall’s lecture) should at least cause one to “think it through”.
But it is a good question. What should one do if you have 1 very elevated risk factor, but have reduced risk factors for everything else? Thats something I cant seem to find good information on. You cant live your life trying to manage every single number that might be deemed a risk factor.
Ed, like you my LDL soared on low carb high fat diet. According to a meta-analysis of >900,000 patients published in The Lancet in 2007, I increased my risk of dying from coronary disease by somewhere between 8 and 16-fold (the exact number is about 8 x sqrt(2) – I have not yet done the math). All other parameters that you mention including BP, triglycerides, CRP, glucose, insulin, A1c have fabulously improved. I am still waiting for my LDL-P to come back but I am scared enough from the epidemiological data to cut my intake of red meat, cheese, whipping cream and the like, and pursue lean protein sources instead. I have not increased my carbohydrate intake and my TSH/fT4/T3 levels were all within normal range. I have also started a statin, which we know from 15-year follow-up of hyperlipidemic individuals does reduce mortality. In our case, there is no need to abandon low carb, but I would recommend abandoning high fat, or at least replacing high fat with healthier fat sources and protein. I realize this will be very controversial here but I don’t know of another way to proceed (and I’m not waiting for my LDL-P to take action). Like you, I am probably very sensitive to the effects of saturated fat and dietary cholesterol.
Dan,
I guess you already investigated the thyroid connection and didn’t find any issues. That in itself is another datapoint.
I was on a statin at one point, but after improving all my other risk factors on an LC diet (except for LDL-C and LDL-P), i decided to ditch them for a while… especially after thinking through how they work. I started to question how I should weigh the well-documented potential improvements in heart health against the anectodal body of evidence that statins might impair brain health long term. So for now I am taking my chances… but this latest test result might swing me in the other direction.
Ed, I checked TSH, fT4, fT3. I did not check rT3. However, I also checked am cortisol and insulin.
If you are convinced you are hyper-absorbing, there are drugs which block intestinal cholesterol absorption such as ezetimibe, colesevelam, cholestipol and cholestyramine. For myself, I prefer a statin, as my LDL at trough on a high carb low fat diet was quite high (and even worse on low carb high fat). Also, statins are much more evidence-based (of those 4 medications, only cholestyramine has a positive clinical trial but this dates to >30 years ago, and it’s a real hassle to take).
To be honest, I am not sure what to make of the “rT3” story. Looking to first principles, it is pretty clear from the literature that adding sat. fat and dietary cholesterol can alone boost LDL to tremendous levels (when I showed 2 cardiologists my lipid panel, they thought I had genetic familial hypercholesterolemia).
Apparently you don’t necessarily need high fat for a ketogenic diet. But probably has to be calorie restricted. It can lower LDL.
The Effects of a High-protein, Low-fat, Ketogenic Diet on Adolescents
https://pediatrics.aappublications.org/content/101/1/61.abstract
@JohnJ: well yeah, at an unsustainable “650 to 725 calories” a day for 8 weeks, these kids had to be in ketosis to keep from dropping dead. But I’m guessing they couldn’t have added much more protein than what they ate and still be ketotic … the “high fat” diet comes into play on the assumption that you don’t want to be starving. A more interesting question is whether these kids could have still lost a lot of weight if they’d been allowed a few more hundred cals of fat per day.
It is not about a fixed ratio there are just general suggestions for people wanting to become keto adapted. You don’t have to stuff yourself with fat to get to a certain ratio, if you are losing weight the amount of fat you lose will contribute to your fat ratio. How sensitive you are to carbohydrates and protein with your insulin response will also have to be taken into account. If you have very high insulin resistance leaving insulin around longer it will also influence how hard it will be to become keto adapted. Each individual has to experiment see what works for him according to his goals, the meter testing can be expensive, but the Ketosis urine test strip even not the best are cheap.
I’m thinking, if you pushed up your cholesterol by eating lots of sugar, that would be harmful high cholesterol.
If you elevated it by eating lots of healthy animal fats, that would be healthy high cholesterol.
Cholesterol testing doesn’t really distinguish between the very different scenarios that the lipids are one symptom of.
It’s like weight: you can weigh a certain amount sitting at home because of the gravitational effect of the Earth on your mass;
or you can weigh the exact same amount in zero gravity because you’re in a rocket accelerating away into empty space.
The exact same phenomenon, weight, and the same weight, as far as you’re concerned, but the consequences for you over time will be very different…