As I’ve often said, I’m a firm advocate for reevaluating previous beliefs in the face of new information. But just having contradictory data doesn’t necessarily warrant a philosophical upheaval. Novel results must first be subject to the same level of scrutiny as any prior data, and they must be weighed against those opposing data to determine which body of evidence is stronger overall. It was with this approach that I read a recent study supporting the existence of a so-called “cholesterol paradox” – the idea, contrary to conventional medical wisdom, that low serum cholesterol is associated with elevated mortality risk, and conversely, that a history of hypercholesterolemia is associated with reduced mortality risk. So is there any merit to this idea?
What they did
Authors Rozanski et al. sought to evaluate the relationship between hypercholesterolemia and all-cause mortality (ACM) by retrospective analysis of observational cohorts consisting of patients who had been referred for one of a variety of cardiac imaging tests: coronary artery calcium (CAC) scanning, coronary computed tomography angiography (CCTA), or stress-rest single photon emission computed tomography myocardial perfusion imaging (SPECT-MPI). The CAC group consisted of 64,357 patients included in the CAC Consortium database, while the CCTA group of 10,814 participants came from the CONFIRM registry. The SPECT-MPI group of 36,462 patients from the Cedars-Sinai Medical Center was subdivided into 31,411 patients who had undergone diagnostic imaging (MPI: diagnostic) and 5,051 cases of known coronary artery disease (MPI: known CAD). For all four groups, Rozanski et al. excluded patients ages 75 and over.
Mortality was determined by national death databases or hospital records. Clinical variables and risk factors, including cholesterol metrics, were obtained via patient questionnaires, from which the investigators defined patients as hypercholesterolemic if they reported either a pre-existing diagnosis of high cholesterol or active treatment with lipid-lowering medications. Other variables, such as smoking status and presence of hypertension and diabetes, were likewise based on self-report. Based on these questionnaires, levels of low-density lipoprotein cholesterol (LDL-C) and non-high-density lipoprotein cholesterol (non-HDL-C) were binned into tertiles for comparing outcomes across different ranges: LDL-C bins were defined as <100 mg/dL, 100-130 mg/dL, and >130 mg/dL, and non-HDL-C bins were defined as <130 mg/dL, 130-159 mg/dL and >160 mg/dL.
What they found
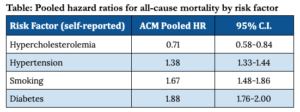
For three of the four cohorts – CCTA, MPI: diagnostic, and MPI: known CAD – the investigators reported that the presence of hypercholesterolemia was associated with greater survival than when hypercholesterolemia was absent. No positive or negative association was observed between hypercholesterolemia and survival for CAC patients. Pooled analyses likewise found that self-reported hypercholesterolemia was associated with lower mortality, with a hazard ratio of 0.71 (95% CI: 0.58-0.84). Contrastingly, self-reported diabetes, smoking, and hypertension were all found to be associated with higher ACM risk across all four groups. Results of pooled analyses are summarized in the table below. Additionally, in a subset of 7,744 CAC and CCTA patients who had also undergone serum lipid testing at the time of scanning, patients with the lowest LDL-C levels (<100 mg/dl) also had lowest survival compared to other LDL-C ranges, consistent with the overall inverse relationship between LDL-C and mortality reported by the investigators.
Where it falls apart
From these data, Rozanski et al. certainly seem to build a strong case for the “cholesterol paradox,” with each piece of evidence falling nicely into line. But a closer look uncovers critical flaws, revealing the theory to be as thin and shaky as a house of cards.
For all except the 7,744 patients who underwent lipid testing at the time of imaging (a mere 7% of study participants), hypercholesterolemia, LDL-C levels, and other clinically relevant variables were entirely based on self-report – a notoriously unreliable means of gathering information. The investigators also failed to assess the duration of hypercholesterolemia, which, because atherosclerotic CVD progresses over time as a function of cholesterol levels, is a key variable for estimating how advanced the disease might be and the magnitude of the associated mortality risk.
Further, the way in which Rozanski et al. defined the presence or absence of hypercholesterolemia – by pre-existing diagnosis or use of lipid-lowering medications – introduces the possibility of a healthy user bias, as those who have had a hypercholesterolemia diagnosis and are taking medications were presumably proactive enough about their health to have had their lipids monitored and to have followed up with treatment. (In other words, if two people are equally hypercholesterolemic, the more health-conscious of the two is also more likely to be aware of their hypercholesterolemia by virtue of additional check-ups.)
The impact of “treatment bias”
The most damning flaw comes from a phenomenon known as “treatment bias.” The authors themselves call attention to this problem, noting that it arises when a risk-associated variable (such as hypercholesterolemia) prompts “potent therapeutic interventions which then modify the outcomes” (such as initiation of lipid-lowering medications). That is to say, the patients with the highest LDL-C levels were also the most likely to receive the most aggressive lipid-lowering treatment – and those treatments work. So those who were categorized into the highest LDL-C tertile based on baseline LDL-C values may well have spent most of the follow-up period with LDL-C values in the lowest tertile – completely inverting the meaning of the study results.
Because the researchers only collected information on patient medications at baseline and had no knowledge of treatments patients may have started later, they could not determine the extent to which treatment bias impacted results. However, they concede that the effect was likely substantial.
A non-existent paradox
The “cholesterol paradox” holds a certain surface-level glamor. It plays on our natural fascination with mystery and desire to question convention. Wouldn’t it be revolutionary if it were true that high cholesterol had no impact on mortality – or was even potentially protective?
But upsetting conventional wisdom takes more than an appealing idea, particularly when convention is backed by reams of research ranging from countless human randomized clinical trials to Mendelian randomizations to (literally) millions of patient-years of epidemiology. With its significant shortcomings, the Rozanski et al. study simply doesn’t come close to providing a convincing argument against the long-held and well-supported wisdom that low LDL levels are associated with reduced risk of CVD and mortality. In the end, the “cholesterol paradox” appears to be little more than a flashy name for a fictitious phenomenon.
For a list of all previous weekly emails, click here.