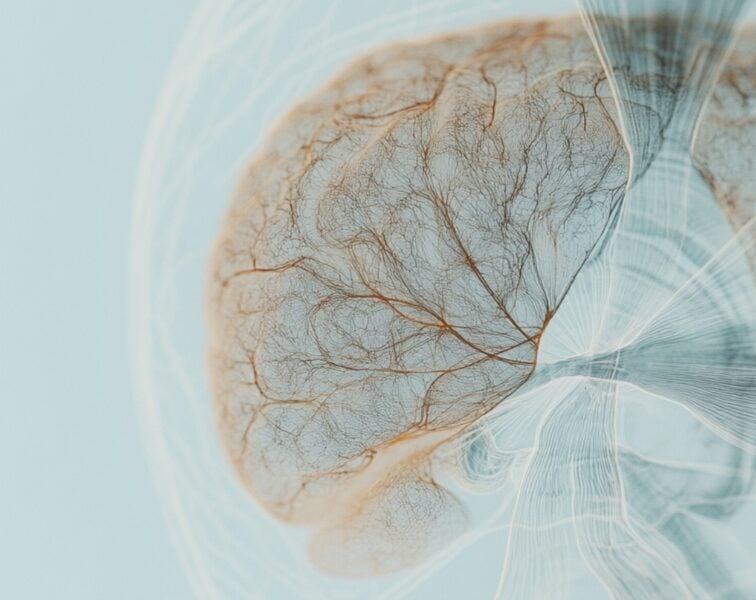
Dan Rader is a Professor at the Perelman School of Medicine at the University of Pennsylvania, where he conducts translational research on lipoprotein metabolism and atherosclerosis with a particular focus on the function of high-density lipoproteins (HDLs). In this episode, Dan goes in-depth on HDL biology, including the genesis of HDL, its metabolism, function, and how this relates to atherosclerotic cardiovascular disease (ASCVD). He explains why having high HDL-C levels does not directly translate to a low risk of cardiovascular disease and reveals research pointing to a better way to measure the functionality of HDL and predict disease risk. He also goes into detail on the role of HDL in reverse cholesterol transport and the benefits this has for reducing ASCVD. Additionally, Dan discusses the latest thinking around the association between HDL cholesterol and neurodegenerative diseases and ends the conversation with a discussion of how the latest research on HDL provides a promising outlook for ongoing trials and future therapeutic interventions.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER

We discuss:
- The lipidology of apoB and apoA [4:00];
- A primer on the high-density lipoprotein (HDL): genesis, structure, and more [9:30];
- How the lipoprotein system differs in humans compared to other mammals [20:00];
- Clarifying the terminology around HDL and apoA [25:30];
- HDL metabolism [31:45];
- CETP inhibitors for raising HDL-C: does it reduce CVD risk? [34:45];
- Why it’s so important to have hard outcome trials in the field of cardiovascular medicine [42:30];
- SR-B1: an HDL receptor important for cholesterol efflux [48:00];
- The association between HDL levels and atherosclerosis: are they causally linked? [53:15];
- How insulin resistance is impacting HDL, and how HDL-C provides insights into triglyceride metabolism [58:00];
- Disappointing results from the studies of niacin—a drug that raises HDL-C and lowers apoB [1:08:15];
- HDL lipidation, dilapidation, and reverse cholesterol transport [1:12:00];
- Measuring the cholesterol efflux capacity of HDL: a better predictor of ASCVD risk than HDL-C? [1:22:00];
- A promising new intervention that may promote cholesterol efflux and reverse cholesterol transport [1:32:45];
- The association between HDL cholesterol and neurodegenerative diseases [1:34:00];
- Challenges ahead, a promising outlook, and the next frontier in lipidology [1:44:45]; and
- More
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
The lipidology of apoB and apoA [4:00]
- Broadly speaking, there are two families of lipids‒ the apoB family and the apoA family
- We have spent much more time talking about the apoB family, and our understanding of its causal relationship to pathology is more clear
Where do these two families fit into the border architecture of our existence?
- Lipoproteins are these big complexes that evolved to transport lipids within the blood
- Lipids are like oil: they don’t mix well with water
- Oil droplets float to the top of a puddle
- We wouldn’t be able to transport lipids in the blood if we hadn’t evolved a mechanism to do that; and lipoproteins are that mechanism
- As their names suggest, lipoproteins have lipid in their core, and then they have proteins that dot the surface
- The proteins allow them to be transported in very complex and sophisticated ways within the bloodstream
- In terms of how they’re metabolized in terms of the receptors they bind to
- In terms of the specific proteins and lipids that they carry
- The proteins allow them to be transported in very complex and sophisticated ways within the bloodstream
- Peter has talked a lot about apoB lipoproteins in previous podcasts; they’re really fabulous
- ApoB lipoproteins evolved to transport triglycerides as a source of energy, from the gut to adipose and muscle and heart, as well as from the liver (during times when we’re fasting)
- They’re very important in terms of causal relationship to atherosclerotic cardiovascular disease (ASCVD)
- HDL is a very complex lipoprotein
- HDL doesn’t have this key protein apoB
- This is why we often refer to the apoB-containing lipoproteins and HDL (the other half)
- HDL is characterized by a different protein called apoA-I
- HDL also transports cholesterol and other complex lipids
Lipoproteins are lipid transport vehicles within the blood; that is the function they evolved to do
- Peter adds, “Unlike glucose, electrolytes (things that we take for granted that are water soluble), we use our circulatory system as the freeway to move these things around. Unfortunately, because of the insolubility of both cholesterol, triglyceride, lipids, etc., we have to come up with this more complicated system.”
The nomenclature gets confusing; clarify the difference between apoA and Lp(a)
- When you talk about apoA, it’s important to realize we are not talking about Lp(a)
- Lp(a) is not the topic of today’s discussion; this is totally different
- ApoA has a capital A after it, and the most important one is ApoA-I
Technically there are two lineages of apoBs
- ApoB-100 is what we refer to virtually all the time we say apoB
- This is in contrast to apoB-48, which is on chylomicrons used to transport lipids/ energy from the gut
A primer on the high-density lipoprotein (HDL): genesis, structure, and more [9:30]
The genesis of the high density lipoprotein (HDL)
- HDL metabolism is perhaps an order of magnitude even more complex than LDL
- Peter agrees, “It is hands down the most confusing stuff in the lipid space”
- ApoA-I as the key protein with HDL
- The analogy is to apoB [on LDL] as Peter alluded to
- Although one big difference is apoB stays with the LDL particle throughout its lifetime
- ApoB gets made by the intestine as B48 or the liver as B100, and it stays with that particle
- Each LDL has one molecule of this huge apoB protein, and then it ultimately gets taken up mostly by the liver after its time in the blood
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Dan Rader, M.D.
Daniel Radar earned his BA at Lehigh University and MD from the Medical College of Pennsylvania. He then trained in internal medicine at Yale-New Haven Hospital. He further trained in human genetics and the physiology of lipoprotein metabolism at the National Institutes of Health.
Dr. Rader is the Seymour Gray Professor of Molecular Medicine at the Perelman School of Medicine at the University of Pennsylvania. There he serves as the Chair of the Department of Genetics as well as the Chief of the Division of Translational Medicine and Human Genetics in the Department of Medicine. He is also the Director of Preventive Cardiovascular Medicine and Lipid Clinic, the Associate Director of the Institute for Translational Medicine and Therapeutics, and the Director of the Cardiovascular Metabolism Unit, Institute for Diabetes, Obesity and Metabolism.
Dr. Rader’s research focuses on the human genetics and functional genomics of lipoprotein metabolism and atherosclerosis, as well as the translational implications for novel therapeutic approaches. He has had a long interest in novel therapeutic approaches to unmet medical needs in the treatment of severe dyslipidemia. He led the scientific and clinical development of a first-in-class inhibitor of microsomal transfer protein for the treatment of homozygous familial hypercholesterolemia. He also has a particular interest in HDL metabolism and function, and novel approaches to targeting HDL metabolism and reverse cholesterol transport in the treatment, prevention, and regression of atherosclerosis.
Dr Rader is a recipient of several national awards, including the Clinical Research Award from the American Heart Association. He is currently the deputy editor of the journal Arteriosclerosis, Thrombosis and Vascular Biology, the Chief Scientific Advisor to the Familial Hypercholesterolemia Foundation, and serves on the Board of Directors of the International Society for Atherosclerosis, the Board of External Experts of the National Heart Lung and Blood Institute, and the Advisory Board for Clinical Research for the NIH. Dr. Rader has been elected to the American Society of Clinical Investigation, the Association of American Physicians, and the Institute of Medicine of the National Academy of Sciences (now the National Academy of Medicine). [Penn Center for Precision Medicine]