I wrote this post at about the same time Germany won the World Cup in Rio de Janeiro in 2014. There’s been a lot of moving and shaking in the world of exogenous ketones since then, not to mention soccer. Looking back on my post, I still consider it relevant in terms of what exogenous ketones possibly can (and cannot) do for performance. In this case, to see if exogenous ketone esters provide me a “boost” by allowing me to do the same amount of work while expending less energy (and work at a relatively lower VO2) compared to no supplementation.
I’m getting an increasing number of questions about exogenous ketones. Are they good? Do they work for performance? Is there a dose-response curve? If I’m fasting, can I consume them without “breaking” the fast? Am I in ketosis if my liver isn’t producing ketones, but my BOHB is 1.5 mmol/L after ingesting ketones? Can they “ramp-up” ketogenesis? Are they a “smart drug?” What happens if someone has high levels of both glucose and ketones? Are some products better than others? Salts vs esters? BHB vs AcAc? Can taking exogenous ketones reduce endogenous production on a ketogenic diet? What’s the difference between racemic mixtures, D-form, and L-form? What’s your experience with MCTs and C8?
Caveat emptor: the following post doesn’t come close to answering most of these questions. I only document my experience with BHB salts (and a non-commercial version at that), but say little to nothing about my experience with BHB esters or AcAc esters. But it will provide you will some context and understanding about what exogenous ketones are, and what they might do for athletic performance. We’ll likely podcast about the questions and topics above and cover other aspects of exogenous ketones in more detail.
—P.A., June 2018
§
Original publication date: August 14, 2014
Last year I wrote a couple of posts on the nuances and complexities of ketosis, with an emphasis on nutritional ketosis (but some discussion of other states of ketosis—starvation ketosis and diabetic ketoacidosis, or DKA). To understand this post, you’ll want to at least be familiar with the ideas in those posts, which can be found here and here.
In the second of these posts I discuss the Delta G implications of the body using ketones (specifically, beta-hydroxybutyrate, or BHB, and acetoacetate, or AcAc) for ATP generation, instead of glucose and free fatty acid (FFA). At the time I wrote that post I was particularly (read: personally) interested in the Delta G arbitrage. Stated simply, per unit of carbon, utilization of BHB offers more ATP for the same amount of oxygen consumption (as corollary, generation of the same amount of ATP requires less oxygen consumption, when compared to glucose or FFA).
I also concluded that post by discussing the possibility of testing this (theoretical) idea in a real person, with the help of exogenous (i.e., synthetic) ketones. I have seen this effect in (unpublished) data in world class athletes not on a ketogenic diet who have supplemented with exogenous ketones (more on that, below). Case after case showed a small, but significant increase in sub-threshold performance (as an example, efforts longer than about 4 minutes all-out).
So I decided to find out for myself if ketones could, indeed, offer up the same amount of usable energy with less oxygen consumption. Some housekeeping issues before getting into it.
- This is a self-experiment, not real “data”—“N of 1” stuff is suggestive, but it prevents the use of nifty little things likes error bars and p-values. Please don’t over interpret these results. My reason for sharing this is to spark a discussion and hope that a more systematic and rigorous approach can be undertaken.
- All of the data I’ll present below were from an experiment I did with the help of Dominic D’Agostino and Pat Jak (who did the indirect calorimetry) in the summer of 2013. (I wrote this up immediately, but I’ve only got around to blogging about it now.) Dom is, far and away, the most knowledgeable person on the topic of exogenous ketones. Others have been at it longer, but none have the vast experiences with all possible modalities (i.e., esters versus salts, BHB versus AcAc) and the concurrent understanding of how nutritional ketosis works. If people call me keto-man (some do, as silly as it sounds), they should call Dom keto-king.
- I have tried the following preparations of exogenous ketones: BHB monoester, AcAc di-ester, BHB mineral salt (BHB combined with Na+, K+, and Ca2+). I have consumed these at different concentrations and in combination with different mixing agents, including MCT oil, pure caprylic acid (C8), branch-chained amino acids, and lemon juice (to lower the pH). I won’t go into the details of each, though, for the sake of time.
- The ketone esters are, hands-down, the worst tasting compounds I have ever put in my body. The world’s worst scotch tastes like spring water compared to these things. The first time I tried 50 mL of BHB monoester, I failed to mix it with anything (Dom warned me, but I was too eager to try them to actually read his instructions). Strategic error. It tasted as I imagine jet fuel would taste. I thought I was going to go blind. I didn’t stop gagging for 10 minutes. (I did this before an early morning bike ride, and I was gagging so loudly in the kitchen that I woke up my wife, who was still sleeping in our bedroom.) The taste of the AcAc di-ester is at least masked by the fact that Dom was able to put it into capsules. But they are still categorically horrible. The salts are definitely better, but despite experimenting with them for months, I was unable to consistently ingest them without experiencing GI side-effects; often I was fine, but enough times I was not, which left me concluding that I still needed to work out the kinks. From my discussions with others using the BHB salts, it seems I have a particularly sensitive GI system.
The hypothesis we sought out to test
A keto-adapted subject (who may already benefit from some Delta G arbitrage) will, under fixed work load, require less oxygen when ingesting exogenous ketones than when not.
Posed as a question: At a given rate of mechanical work, would the addition of exogenous ketones reduce a subject’s oxygen consumption?
The “experiment”
- A keto-adapted subject (me) completed two 20-minute test rides at approximately 60% of VO2 max on a load generator (CompuTrainer); such a device allows one to “fix” the work requirement by fixing the power demand to pedal the bike
- This fixed load was chosen to be 180 watts which resulted in approximately 3 L/min of VO2—minute ventilation of oxygen (this was an aerobic effort at a power output of approximately 60% of functional threshold power, FTP, which also corresponded to a minute ventilation of approximately 60% of VO2 max)
- Test set #1—done under conditions of mild nutritional ketosis, while still fasted
- Test set #2—60 minutes following ingestion of 15.6 g BHB mineral salt to produce instant “artificial ketosis,” which took place immediately following Test set #1
- Measurements taken included whole blood glucose and BHB (every 5 minutes); VO2 and VCO2 (every 15 seconds); HR (continuous); RQ is calculated as the ratio of VO2 and VCO2. In the video of this post I explain what VO2, VCO2, and RQ tell us about energy expenditure and substrate use—very quickly, RQ typically varies between about 0.7 and 1.0—the closer RQ is to 0.7, the more fat is being oxidized; the reverse is true as RQ approaches 1.0
Results
Test set #1 (control—mild nutritional ketosis)
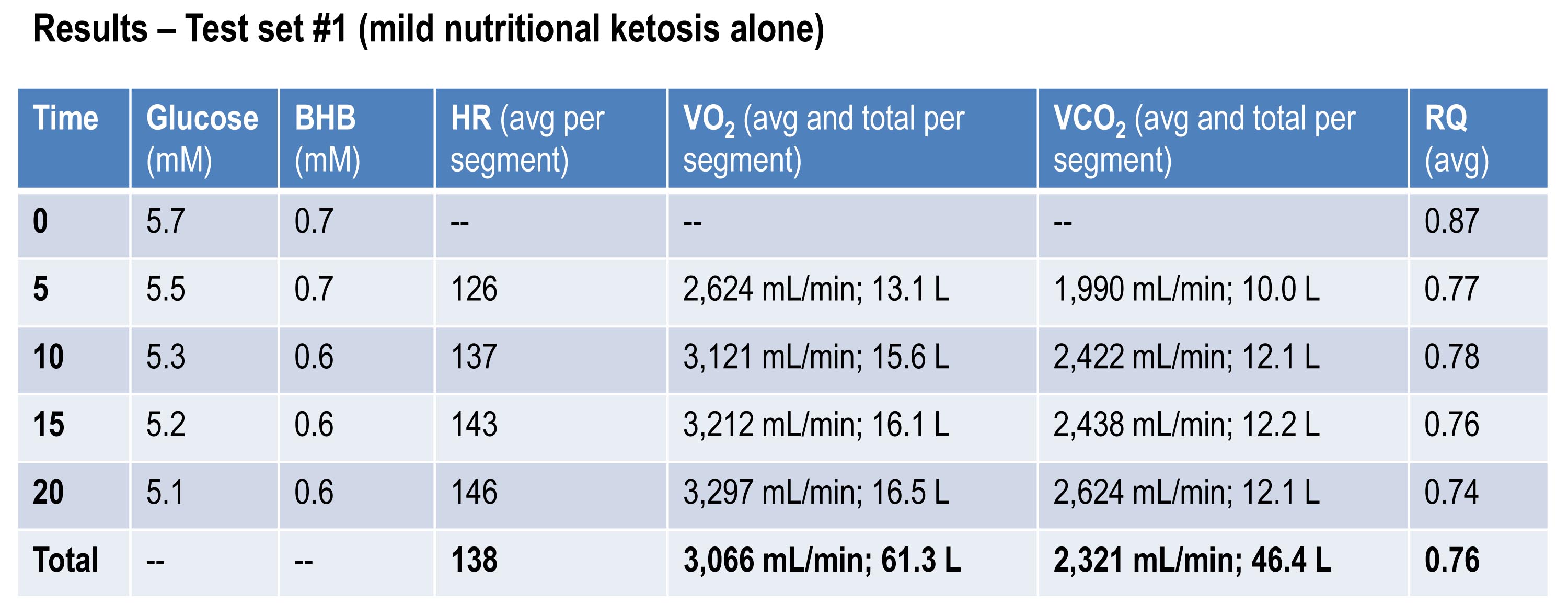
The table below shows the data collected over the first 20 minute effort. The 20 minute effort was continuous, but for the purpose of presenting the data, I’ve shown the segmental values—end of segment for glucose and BHB; segment average for HR, minute ventilation (in mL per min), and RQ; and segment total for minute ventilation (in liters).
Glucose and BHB went down slightly throughout the effort and RQ fell, implying a high rate of fat oxidation. We can calculate fat oxidation from these data. Energy expenditure (EE), in kcal/min, can be derived from the VO2 and VCO2 data and the Weir equation. For this effort, EE was 14.66 kcal/min; RQ gives us a good representation of how much of the energy used during the exercise bout was derived from FFA vs. glucose—in this case about 87% FFA and 13% glucose. So fat oxidation was approximately 12.7 kcal/min or 1.41 g/min. It’s worth pointing out that “traditional” sports physiology preaches that fat oxidation peaks in a well-trained athlete at about 1 g/min. Clearly this is context limited (i.e., only true, if true at all, in athletes on high carb diets with high RQ). I’ve done several tests on myself to see how high I could push fat oxidation rate. So far my max is about 1.6 g/min. This suggests to me that very elite athletes (which I am not) who are highly fat adapted could approach 2 g/min of fat oxidation. Jeff Volek has done testing on elites and by personal communication he has recorded levels at 1.81 g/min. A very close friend of mine is contemplating a run at the 24 hour world record (cycling). I think it’s likely we’ll be able to get him to 2 g/min of fat oxidation on the correct diet.
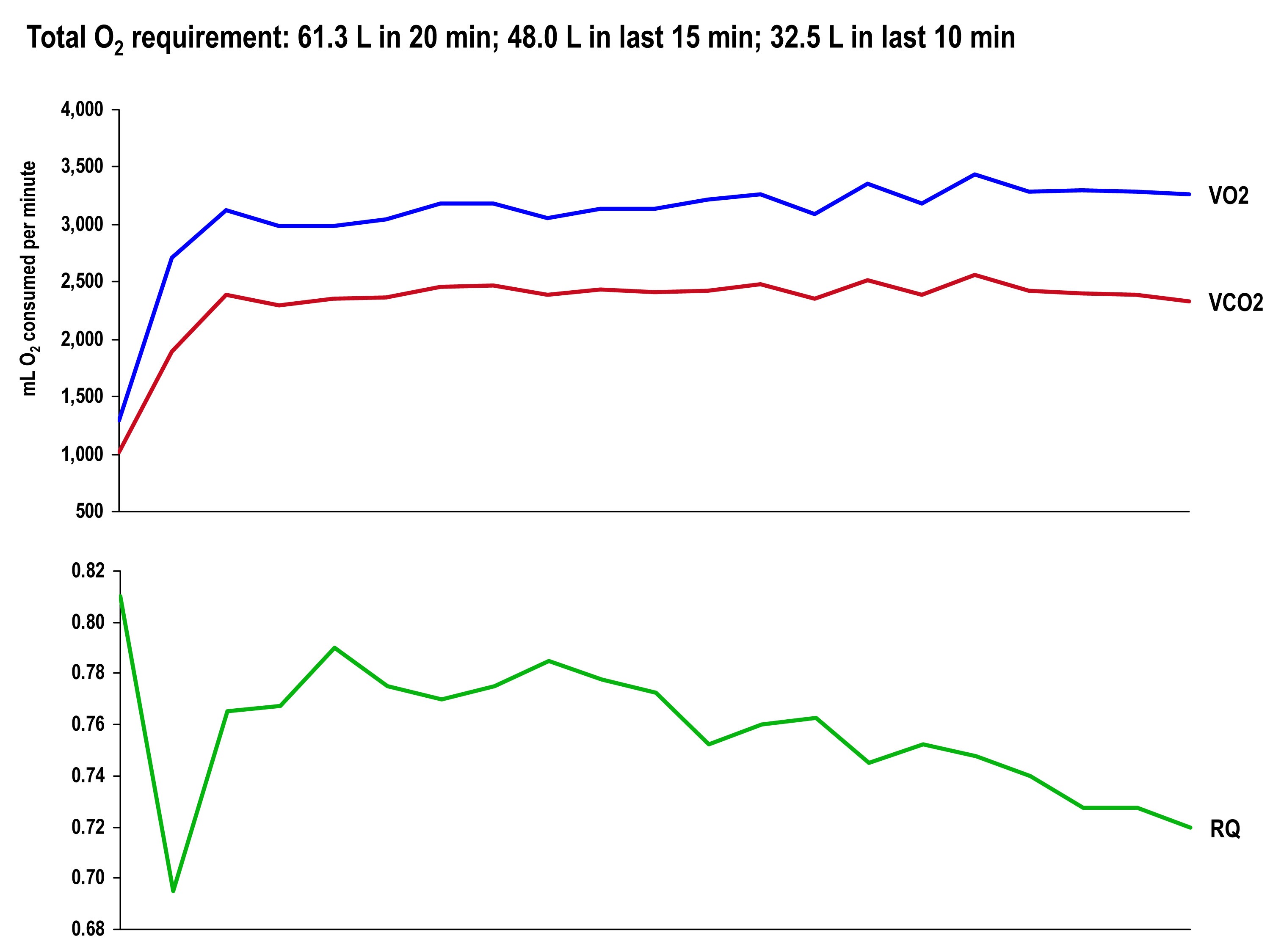
The graph, below, shows the continuous data for VO2, VCO2 (measured), and RQ (calculated).
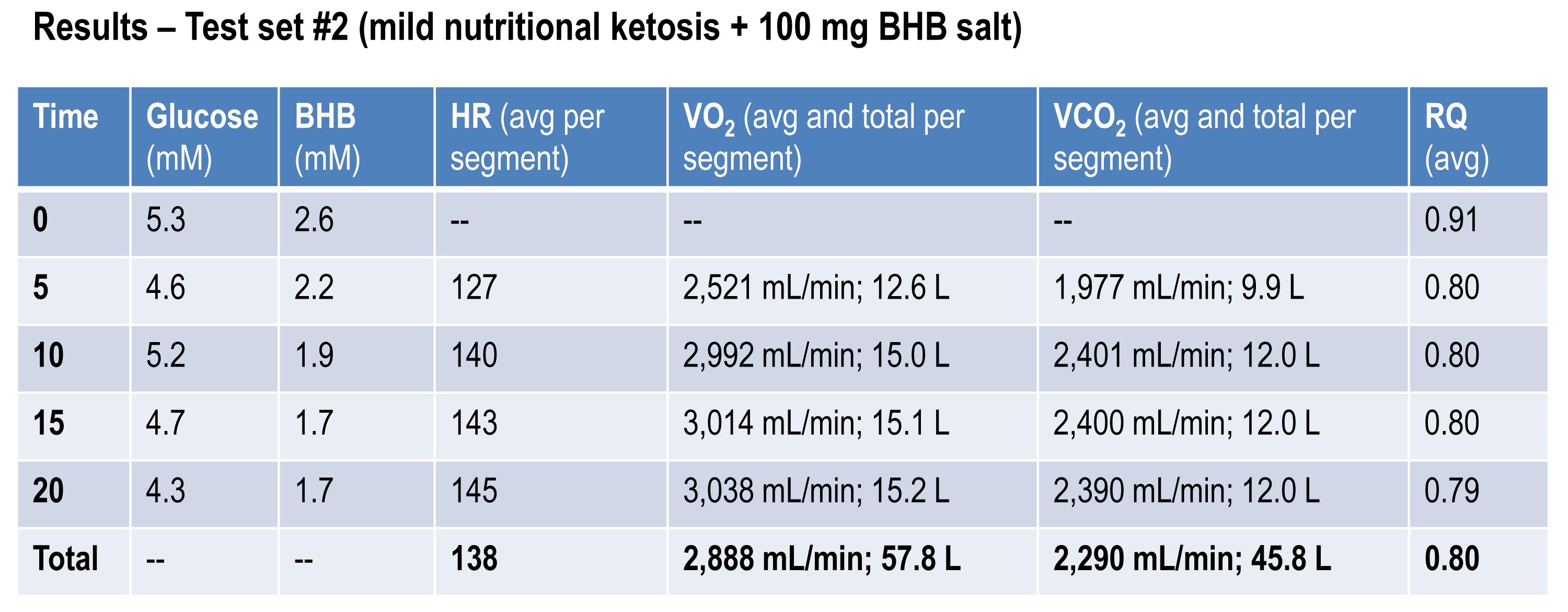
Test set #2 (ingestion of 15.6 g BHB salt 60 minutes prior)
The table below shows the same measurements and calculations as the above table, but under the test conditions. You’ll note that BHB is higher at the start and falls more rapidly, as does glucose (for reasons I’ll explain below). HR data are almost identical to the control test, but VO2 and VCO2 are both lower. RQ, however, is slightly higher, implying that the reduction in oxygen consumption was greater than the reduction in carbon dioxide production.
If you do the same calculations as I did above for estimating fat oxidation, you’ll see that EE in this case was approximately 13.92 kcal/min, while fat oxidation was only 67% of this, or 9.28 kcal/min, or 1.03 g/min. So, for this second effort (the test set) my body did about 5% less mechanical work, while oxidizing about 25% less of my own fat. The majority of this difference, I assume, is from the utilization of the exogenous BHB, and not glucose (again, I will address below what I think is happening with glucose levels).
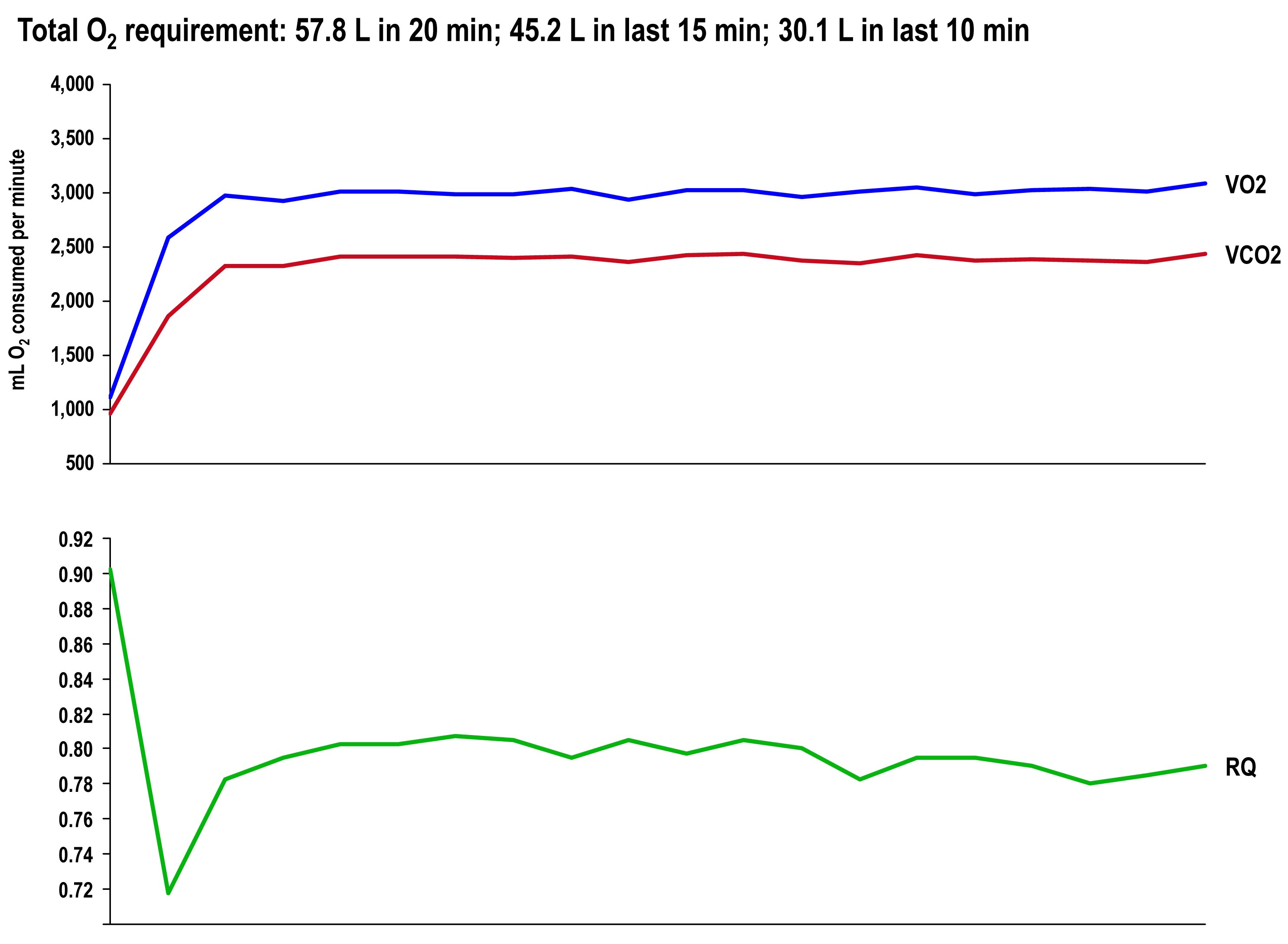
The graph once again shows the continuous data for VO2, VCO2 (measured), and RQ (calculated).
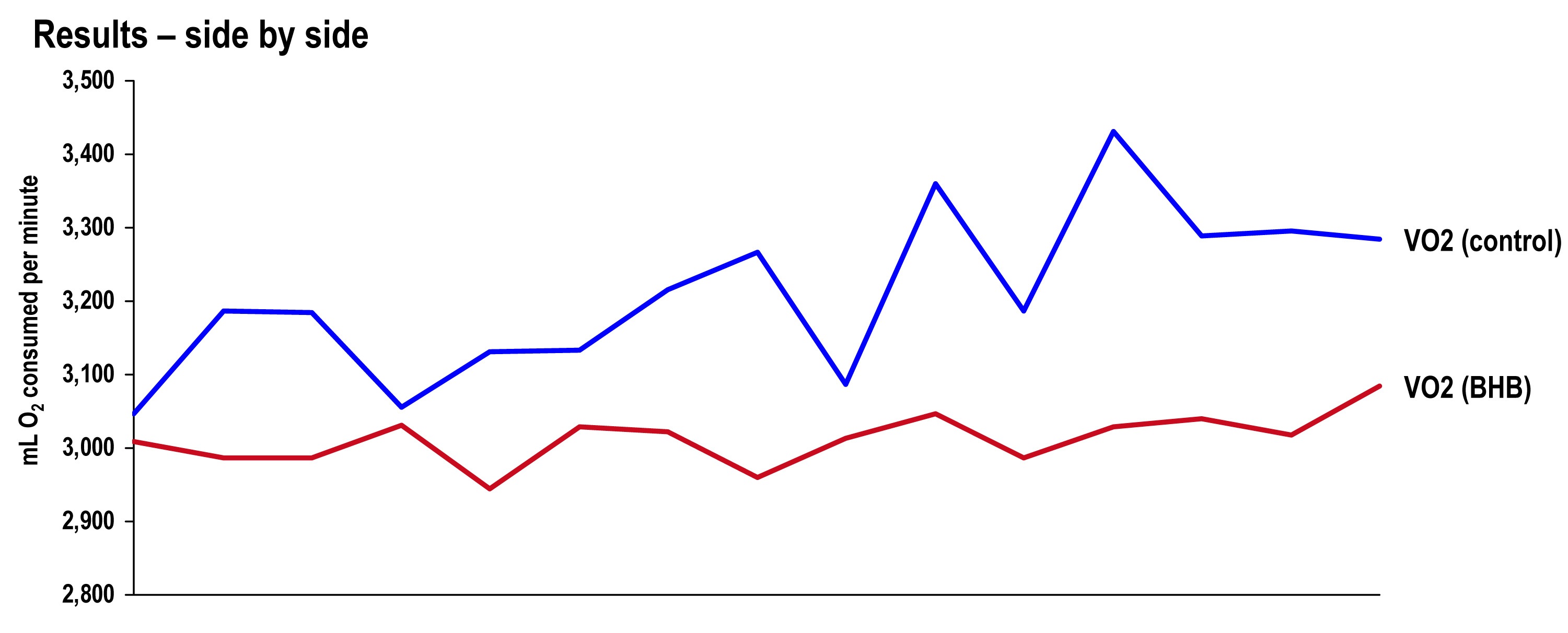
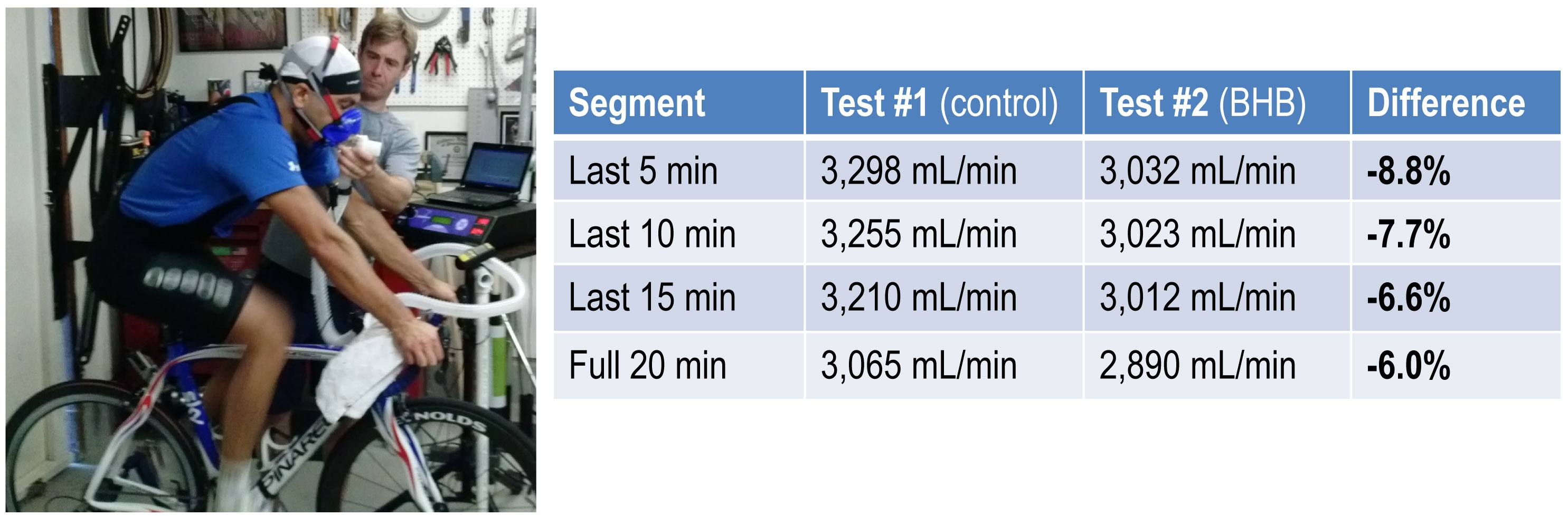
Side-by-side difference
The final graph, below, shows the continuous data for only VO2 side-by-side for the 20 minute period. The upper (blue) line represents oxygen consumption under control conditions, while the lower line (red) represents oxygen consumption following the BHB ingestion. In theory, given that the same load was being overcome, and the same amount of mechanical work was being done, these lines should be identical.
The hypothesis being tested in this “experiment” is that they would not be the same. Beyond visual inspection, the difference between the lines appears to grow as the test goes on, which is captured in the tabular data showing 5 minute segmental data.
Limitations
The most obvious limitation of this endeavor is the fact that it’s not an appropriately controlled experiment. Putting that aside, I want to focus on the nuanced limitations—which don’t impact the primary outcome of oxygen consumption—even if one were appropriately doing a real experiment.
- It’s not clear that the Weir coefficients used to estimate EE are relevant for someone in ketosis, let alone someone ingesting exogenous BHB. (The Weir formula states that EE is approximated by 3.94 * VO2 + 1.11 * VCO2, where VO2 and VCO2 are measured in L/min; 3.94 and 1.11 are the Weir coefficients, and they are derived by tabulating the stoichiometry of lipid synthesis and oxidation of fat and glucose and calculating the amount of oxygen consumed and carbon dioxide generated.) While this doesn’t impact the main observation—less oxygen was consumed with higher ketones—it does impact the estimation of EE and substrate use.
- In addition to the Weir coefficients being potentially off (which impacts EE), the RQ interpretation may be incorrect in the presence of endogenous or exogenous ketones. As a result, the estimation of fat and glucose oxidation may be off (though it’s directionally correct). That said, the current interpretation seems quite plausible—greater fat oxidation when I had to make my ketones; less when I got my ketones for “free.”
Observations from this “experiment” (and my experience, in general)
Animal models (e.g., using rat hearts) and unpublished case reports in elite athletes suggest supplemented BHB produces more ATP per unit carbon and per unit oxygen consumed than glycogen and FFA. This appears to have been the case in my anecdotal exercise.
The energy necessary to perform the mechanical work did not appear to change much between tests, though the amount of oxygen utilization and fat oxidation did go down measurably. The latter finding is not surprising since the body was not sitting on an abundant and available source of BHB—there was less need to make BHB “the old fashioned way.”
As seen in this exercise, glucose tends to fall quite precipitously following exogenous ketone ingestions. Without exception, every time I ingested these compounds (which I’ve probably done a total of 25 to 30 times), my glucose would fall, sometimes as low as 3 mM (just below 60 mg/dL). Despite this, I never felt symptomatic from hypoglycemia. Richard Veech (NIH) one of the pioneers of exogenous ketones, has suggested this phenomenon is the result of the ketones activating pyruvate dehydogenase (PDH), which enhances insulin-mediated glucose uptake. (At some point I will also write a post on Alzheimer’s disease, which almost always involves sluggish PDH activity —in animal models acute bolus of insulin transiently improves symptoms and administration of exogenous ketones does the same, even without glucose.)
In addition, the body regulates ketone production via ketonuria (peeing out excess ketones) and ketone-induced insulin release, which shuts off hepatic ketogenesis (the liver making more ketones when you have enough). The insulin from this process could be increasing glucose disposal which, when coupled with PDH activation, could drive glucose levels quite low.
If that explains the hypoglycemia, it would seem the absence of symptoms can be explained by the work of George Cahill (back in the day; see bottom figure in this post)—when ketone levels are high enough they can dominate brain fuel, even ahead of glucose.
Finally, these compounds seemed to have a profound impact on my appetite (they produced a strong tendency towards appetite suppression). I think there are at least two good explanations for this, which I plan to write about in a dedicated post. This particular topic—appetite regulation—is too interesting to warrant anything less.
Open questions to be tested in real experiments
- Are these results reproducible? If so, how variable are the results across individuals (by baseline metabolic state, diet, fitness)?
- Would the difference in oxygen consumption be larger (or smaller) in an athlete not already keto-adapted (i.e., not producing endogenous ketones)?
- Would the observed effect be greater at higher plasma levels of BHB (e.g., 5 to 7 mM), which is “easily” achievable with exogenous ketones?
- Would the observed effect be the same or different at higher levels of ATP demand (e.g., at FTP or at 85-95% of VO2 max)?
- Would the trend towards improved energy efficiency continue if the exercise bout was longer in duration (say, greater than 2 hours)?
- How will exogenous ketones impact exercise duration and lactate buffering?
- Why do exogenous ketones (both BHB and AcAc it seems) reduce blood glucose levels so much, and can this feature be exploited to treat type 2 diabetes?
- Are there deleterious effects from using exogenous ketones, besides GI side-effects?
- What are the differences between exogenous BHB and AcAc (which in vivo exist in a reversible equilibrium) on this particular phenomenon? (Work by Dom D’Agostino’s group and others have shown other differences in metabolic response and clinical application, including their relative impact on neurons.)
Photo by Alexey Lin on Unsplash







Peter,
Super interesting stuff here. I was just started trying to get keto-adapted drinking a whiskey soda with my buddy John Markell, he said to look you up. I did and this stuff is great. As an exercise endurance nerd scientist myself I love this stuff. I tried to get in the FAT-ADAPT study on ultra runners, but was in the middle diet wise.
So now my question. As for the lower O2 consumption on BHOB I wonder if any of that is from the extra energy is takes to makes BHOH from fatty acids rather than having directly at your disposal. You previously showed that it you lose about 20% of energy from deriving the ketones from fatty acids versus an exogenous supply, the aptly named Hall effect. Could this (in part) explain the -6% change in VO2 on exogenous BHOB?
This maybe herisay, but what about a 3rd trial with an isocaloric CHO supplement? Of course being keto-adapted this would be tough to interpret. Double blind crossover study anyone?
Last side point. I’m currently doing aging research and the NIA has an intervention testing program for potential anti-aging compounds. I was thinking about proposing BHOB although MCT had no effect (https://www.ncbi.nlm.nih.gov/pubmed/22451473).
Looking forward to the next n=1 experiment.
Matthew, Veech et al. showed in rat hearts (the most “pure” model for work vs. O2 consumption) something like a 38% reduction in O2 requirement for a fixed work output. This was using BHB ester, which is what gave me the idea to try this “experiment.” Your question is a good one–is the same effect found in NK. I suspect the answer is yes, because the arbitrage of energy comes from the krebs cycle, where BHB is “consumed” not from the process of generating ketones, I can’t be sure without an experiment, preferably much more rigorous than the one I did.
Matthew,
Why not propose BHB, or a BHB/ACA combination in physiologic proportions?
1: Edwards C, Canfield J, Copes N, Rehan M, Lipps D, Bradshaw PC.
D-beta-hydroxybutyrate extends lifespan in C. elegans. Aging (Albany NY). 2014
Aug;6(8):621-44. PubMed PMID: 25127866; PubMed Central PMCID: PMC4169858.
…This effect appears related to HDAC inhibition, about which it’s also quite worthwhile to read the reviews from Eric Verdin and JC Newman. Also,
1: Scheibye-Knudsen M, Mitchell SJ, Fang EF, Iyama T, Ward T, Wang J, Dunn CA,
Singh N, Veith S, Hasan-Olive MM, Mangerich A, Wilson MA, Mattson MP, Bergersen
LH, Cogger VC, Warren A, Le Couteur DG, Moaddel R, Wilson DM 3rd, Croteau DL, de
Cabo R, Bohr VA. A high-fat diet and NAD(+) activate Sirt1 to rescue premature
aging in cockayne syndrome. Cell Metab. 2014 Nov 4;20(5):840-55. doi:
10.1016/j.cmet.2014.10.005. Epub 2014 Nov 4. PubMed PMID: 25440059; PubMed
Central PMCID: PMC4261735.
…Plenty of thought-provoking stuff here, BHB is one of the experimental conditions in play, appears that both BHB and the sirtuin cofactor NAD+ can activate SIRT1 and rescue a premature aging phenotype.
Its a good point Rob and I am actually quite familiar with the Verdin paper (and the lifespan extension in worms). The BHB HDAC connection is an interesting one that we are playing with a little in lab also.
A recent paper did look at the effects of exogenous BHB supplementation during exercise and at rest, showing a decrease in circulating glucose AND lipolysis (without an increase in insulin) suggesting a mechanism distinct from merely having low glycogen stores and low insulin in regulating lipolysis.
Systemic, cerebral and skeletal muscle ketone body and energy metabolism during acute hyper-D-?-hydroxybutyrataemia in post-absorptive healthy males.
J Clin Endocrinol Metab. 2014 Nov 21;:jc20142608
Authors: Mikkelsen KH, Seifert T, Secher NH, Grøndal T, van Hall G
The main conclusions: “Results: 1. An increase in HOB from the basal 160 to 450 ?mol/L elicited 14±2% reduction (P=0.03) in glucose appearance and 37±4% decrease (P=0.03) in lipolytic rate while insulin and glucagon were unchanged; 2. Endogenous HOB appearance was reduced in a dose-dependent manner with complete inhibition at the highest HOB concentration (1.7 mmol/L); 3. Cerebral HOB uptake and subsequent oxidation was linearly related to the arterial HOB concentration; 4. Resting skeletal muscle HOB uptake showed saturation kinetics.”
Re your August 31 post.
Stumbled on this website today. Seems like work and analysis done to a reasonably high standard. But, there is an enormous argument against using ketones as fuel, and that is the inescapable concomitant damage to the endothelium. Not by the ketones themselves (I am unaware of any studies showing direct harm) but by the diet necessary to achieve ketosis.
Chronic damage to the endothelium is the gateway to atherosclerotic heart disease. Caldwell Esselstyn has been instrumental in bringing attention to this.
So, I started reading this blog back in April. On the 20th of April I went lchf. 50+ lbs later i don’t even use a scale anymore because look and feel so good. Hiking for hours is super easy, eating 1-2 times a day is so convenient, and not restricting portions is a huge stress relief.
Thank you, I really appreciate the information and recommend it often to those that are interested. Again thank you. Cant wait for the next post.
Great to hear Lewis.
Peter, I was wondering whether you can discuss at some point the interaction between a LCHF diet and Tamixifen. Been taking Tamoxifen for almost two years and following a LCHF diet but have belly fat accumulation that is really demoralizing. Exercising 3x/wk also. Tamixifen did get me to menopause…any help appreciated.
Hi Peter,
I’m seriously considering a career as a dietitian as I would like to a) learn more about the “science” behind nutrition for my personal benefit and b) be able to disseminate this information and encourage others to lead healthier lives, specifically the geriatric population for whom a healthy lifestyle is paramount. I’m glad I came across your TED talk and blog at this time; your commitment to bringing the “real science” to the fore of nutrition education is exactly what I hope to embody in my future (potential) career. Do you have an opinion on the current standards required of Registered Dietitians? I’ve searched “dietitian” on your blog and it seems you lump them with other licensed healthcare workers that subscribe to the conventional and problematic wisdom about nutrition. Since registered dietitians are at the front line of being the “authority” on diet in hospital settings, restaurants, prisons, schools, the world over, what would you say to aspiring dietitians such that they could be assets in this movement you are spearheading (hope you don’t mind if I put it that way) to conscientiously purvey the current and evolving science of nutrition?
Typically an RD is earned after a bachelor’s degree.
I stumbled onto you blog earlier this year and my life has not been the same since. It took me a while to adjust and fine tune my eating. I currently maintain a diet that is 75% Fat, 25% Protein, and 5% Carbs. I have never felt better and I’ve also lost 30 lbs in about 4 months. Thank you for all that you do, I am sure you are helping many to get control of they lives. Merry Christmas and Happy New Year!!
Thank you, Dominick, and congrats on your journey.
Hi Peter,
I’ve been ‘keto-adapted’ for a year (and feel the many benefits of it). I recently had a few nosebleeds (three this week) and in my quick online search, found a lack of vitamin k could be the culprit. I do eat salads and veggies, and the occasional wilted kale or swiss chard, but could probably increase those a bit. But in my search, I also came across a number of discussions regarding the “fact” (?) that a ketogenic diet makes the blood “sticky” and several people (online) related that to their own blood clots/embolism events. Can you weigh-in on this topic, and the risks associated (and how to mitigate?). Thanks in advance for your reply.
News to me. Also, if ketosis leads to hypercoagulability, wouldn’t you be less likely to have nosebleeds?
I’m very confused about the digestion of Fat.
I read that solid human waste typically contains between 10 to 20% Cholesterol and other Fats.
So… The calories from those fats were never absorbed or metabolized and you never had to burn them.
To my limited knowledge… Fats are the only type of digestible, food-stuff in human waste.
Everything else – If we can digest it and metabolize it then we eventually need to burn it.
But – How does that work?
Why is there any Fat at all in Human Waste? Why don’t we absorb and metabolize 100% of the Fat we eat like we do with every other type of digestible food we eat?
And – What is the Fat content of waste from a person who lives on a diet that’s 80% fat?
What % of Calories from Fat passes through the body without being absorbed and metabolized?
Thanks for all your hard work.
Dave, except in cases of malabsorption, there is actually very little fat in human stool. We’re pretty efficient at absorbing it.
Dave – I have heard of a couple of studies where high dairy/calcium diets can increase fat excretion but this is likely related to malabsorption as per Peter’s comments.
Peter – Thanks for recent talk with Ben Greenfield & podcast with Tim Ferriss -> both excellent. A Christmas bonus for a geek like me. Your fans will know you do not make many appearances (given constraints on your time), but when you do, standard of info is second to none.
PS, Is NuSi due to publish results of Energy Balance Consortium study anytime soon? (think it was due to close last June?)
I think Tim and I will do a part II in early ’15. Long way from pub.
Always happy to wait as standard is so high (you have a small captive audience I imagine).
Looking forward to round 2 with Tim.
FYI, not a wealthy chap but just donated to the NAFLD study ($200K of donations are being matched, how great is that?!), tis the season – hope you have a great one.
Forever thankful for all your hard work, means the world to a time-starved, information-starved geek like me.
Thanks very much JJ.
Hi Peter
I have only recently discovered your blog and there is much to learn. I have a question re serum insulin levels. I am currently in my fourth week of lchf diet. Before I started fasting bg was 5.9 mmol/l and fasting insulin was sitting at 27.
Do you have information regarding how insulin levels reduce with this type of diet. I’m currently in ketosis levels any where between 2.7 to 1.00mmol/l and i have noticed fasting bg now sitting at ave 5.4mmol/l. I’m curious to see how longit will take to get normal insulin levels again.
Highly variable–and in some people, for reasons we don’t know, it may get worse–but improved hyperinsulinemia can improve inside of 3 months.
Hi Peter,
Loved your interview with Tim Ferriss. And this Blog. Great stuff. Although I am not a researcher by profession I’ve done quite a bit research on cancer and “best” supplements.
If I may ask, what are you thoughts on the following:
(I take all of these for optional health)
1) Baking Soda: I take this daily based on the Italian Oncologist Dr.Simoncini’s research it kills cancer cells.
2) Royal Jelly: For anti-aging and immune support. And overall superhumaness. =)
3) Colostrum: Miracle food for immune support and recovery.
4) Bee Pollen
When was younger I would get colds often and was told by a microbiologist that I was “Strong as a horse but have a weak immune system” The above-mentioned made a drastic change in my health and have not had a cold for over a day in 3 years.
Your thoughts on the above?
Also any recommendations for elevated liver enzymes? 3 years ago I ruptured a disc deadlifling and over did it on Ibuprofen. (I foolishly did not bother to research the side affects of this)
Thanks Peter.
Interesting that in the second trial, glucose went down, VCO2 and RQ increased (versus first trial). I know you phrased the explanation as the “VCO2 didn’t go down as much as the VO2”, but if someone just put the numbers for glucose, VCO2 and RQ in front of me without the addition of the BHB data, I’d say the person was utilizing more carbohydrate. Is it possible the exogenous BHB allows for greater non-oxidative glycolysis at lower VO2’s? You didn’t happen to measure lactate, did you? Also, were the differences between the trials significant? Thanks for your always great posts
I didn’t measure lactate on this one.
I have just read far enough down in the comments to find that you have a new baby. Congratulations to you and your family!
I’ve been amazed that you’ve continued to blog at all since the founding of NuSI. I, for one, have learned so much from this blog, that if you never write another word (including the final cholesterol, insulin and/or thyroid posts – did that just make you break out into an anxiety sweat? haha), I would be a happy camper because you dropped crumbs and laid foundations for people to easily continue their self education with a strong direction.
Maybe with a new baby, you’re getting even less sleep, so you blog on, but no matter what or when you choose to write, it’s very much appreciated
Thanks, JB. Little guy is 4 months old today, actually. I’m not sure one could say that I “continue” blogging, but I guess I still keep the blog up…
I want to pass along appreciation for you work. After my dad had a stent and was treated for prostate cancer he followed Esselstyn’s very low fat diet, ground his own grains, made his own sour dough starter ; did all the “right” things. Initially he felt better, perhaps because he cut out the cookies and other sugars, but after about a year of that he was feeling tired. His cholesterol had gone up, and he needed 3 more stents. He was pretty disappointed. Then he found your blog. He has cut out all grains, eats animal fats and non starchy veggies, feels better and last cholesterol check was down. I’m also following a much lower carb diet and feeling better. Thank you for putting your work out there, and providing the information for people to improve health and life.
Susan, thanks for sharing your experience (and especially that of your dad). I do hope your dad has a thoughtful cardiologist looking after him who is more interested in his LDL-P and Lp(a)-P than just “cholesterol.” Advanced testing of lipoproteins is essential, in my opinion, for anyone with a significant risk profile for CHD.
Hi Peter,
As you are one of the few people I truly trust in this emerging and controversial field, I was hoping for some (quick) advice about how to eat while pregnant. I know this is a upcoming topic on your blog, but I am newly pregnant and anxious to do the right thing.
I’ve been mostly in ketosis since September, normal weight, and workout (Pure Barre) about 3x/week. My only negative symptoms from this diet is my hair started falling out a bit more in month 3, and my blood pressure is even lower than normal (so I have to stand up slowly, but it’s not a big deal). I eat a salad (and a prenatal) a day, but way fewer fruits than I used to. I know the research is mixed at best about fruits and veggies being good for you, but it’s still a bit scary not focusing on those when I’m pregnant.
In sum, would you recommend being in nutritional ketosis while pregnant? I just can’t find solid research where I’ve been looking.
Thanks for your time and for everything you’re doing. Your efforts mean so much to so many people.
Anna
Anna, there are no data to my knowledge that a ketogenic diet is ideal during pregnancy, and I would be reluctant to suggest it is. So knowing nothing, I would *assume* the optimal diet would contain some starch, in addition the foods you’re probably already eating.
My guess, by the way, based on the FGF-21 literature, is that ketosis would not support fertility in females.
Peter, have you done any research on MAP a “master amino acid” supplement. I have been using MAP as part of my training which is nothing compared to the stuff you are discussing.
Here is my problem, when I use MAP in conjunction with other supplement, my heart rate during a run is very slow. Yesterday I did a 4.5 mile run. My average rate 89 bpm. For the first 3 miles my hr climbed from 55 bpm to 75 bpm. At about the three mile mark my hear rate went from 75 to 150-160 range.
I am trying to understand if this is an energy metabolism issue and if there are health risks associated with the protocol. I am going to discuss with my family doctor could address but I am not sure if he has the necessary background in area of bio energy and supplement… (I was thinking of your ketosis warning to your patient on the Atkins’ diet). MAP seems to be the common element in my the slow heart rate while racing or training. When I don’t follow the protocol my heart rate would climb quickly to 125 and then gradually increase to 145…165 depending on speed and distance. Any thoughts on MAP? NOTHING ON THE MAP SITE ABOUT ANY AFFECT ON HEART RATE.
I have not.
Hey Peter! Greetings from Spain! Huge fan of your work.
I wanted to ask you a question from the evolutionary standpoint. I always think that when we’re discussing the ideal diet and lifestyle for the human being, we must consider evolutionary biology and what we evolved to thrive on. But when I try to figure out what that is, there seems to be something missing.
Our ancestors were hunter-gatherers, and their diet was probably mainly composed by nuts and seeds, plants and vegetables available in their surroundings and the occasional hunt and access to animal protein and fat. But here’s my question: doesn’t it seem like compared to today, our ancestors would only have access to far less calories and yet not only did they survive but they supposedly thrived on that? I just find it almost impossible that our ancestors would be able to find that many calories on a daily basis. And being in the wild, they needed to have adequate muscle mass and energy to survive yet alone to thrive.
The only possible explanation I see is efficiency. Their energy expenditure and micronutrient use must have been vastly more efficient. Their lifestyle would probably be much closer to Intermittent Fasting, which stimulates the body to be more efficient because of the scarcity of food. I know IF is on your ‘coming soon’ list and this a very broad question but I wanted to get your thoughts on that since to me there seems to be a huge disconnect between the daily caloric consumption, and yet that’s how our ancestors have lived for millions of years and supposedly thrived on that.
Certainly long enough periods of exposure to fasting could lower energy expenditure (i.e., more “efficiency”), but it’s also worth noting that studies of modern day HG societies with doubly-labeled water suggest they actually expend less overall energy (deliberate + nondeliberate) that “modern” man, in part because when they aren’t looking for food or reproducing, they are laying low and preserving energy.
I came across your blog after the Tim Ferris show. I’m training for an Ironman August ’15 (completed a half years ago). I generally eat low carb anyway so I’m enjoying reading how to utilize energy.
Also, I’m shopping for synthetic ketones because like you, I assume I can tolerate poor tasting supplements. I found KetoForce, but I’ll keep looking.
Thanks!
Mike
The new one tastes really good.
*Always* stimulating to end my night reading your thoughts, thank you for your focused & steady work 🙂
1) Why do you think you start out w/ such high RQ? Is this more measurement error due to being rested while using a high-flow cart?
2) Along the same thoughts, should we not ignore the first 5-min avg since it includes that ramping up time (probably a lot of error before reaching steady HR)?
3) What happened during those two ^–^ during the third quarter of Test set #1? Did someone make you laugh?
4) Mon morning QB comment here: upon viewing these two results, I did not see a difference — instead, I would be back to the drawing board. Will you go back to the drawing board?
Lastly, the first table has an error, and I notice an unlikely coincidence: the first 5min of O2 consumed is equivalent to the last 5min of CO2 exhaled, the latter out of place. CO2 out was dropping in last 5 min.
I hope this is constructive contribution to your efforts. I’m nose-to-the drawing board, seeing if I can prep to detect EPOC. Best cheers and wishes for you & yours, DJ
I have no plans any time soon to work on this. Not high enough on the priority list relative to other demands. Hope others do.
Understood, and respected.
BTW, after listening intently and repeatedly to your Tim Ferris discussion, I gobbled up “Mistakes were made … BUT NOT BY ME!” (emphasis mine, reflecting my own struggles with this very issue). Many thanks for recommending it in the public space!
A quote, “Science, a form of arrogance control”
Love it!
Again, best to your and yours!
DJ
Glad you enjoyed. Since reading this book, Carol has become a close friend and is now an adviser to NuSI.
Great post. I’m struggling to find any toxicology reports on 1-3 butanediol. Specifically I’m interested in the enantiomers. I’ve ordered a racemic mixture which should negate any issues as Veech, R. L (2003) states we utilise both forms of Beta-Hydroxybutyrate. Just wondered if you had more insight? Cheers, Will.
I didn’t think L-beta-hydroxybutyrate had a particular metabolic path. Re the enantiomers of the BHB and the butanediol, Clarke and Veech’s most recent patent of the ester (there is a series of them, this is 2014), US 8,642,654 B2 elaborates:
“…one particular enantiomer of one particular ester of 3-hydroxybutyrate is an effective and palatable precursor to the ketone body (3R) hydroxybutyrate.Accordingly,the present invention provides a compound which is 3-hydroxybutyl 3-hydroxybutyrate enantiomerically enriched with respect to (3R)-hydroxybutyl (3R)-hydroxybutyrate… prepared by a process which comprises carrying out a trans-esterification reaction between ethyl (3R)-hydroxybutyrate and (3R)-1, 3-butanediol in the presence of a lipase enzyme… Two particular advantages are…First, the (3R, 3R‘) enantiomer is palatable and is less bitter-tasting than other ketone bodies.It is therefore particularly well-suited for oral administration. This contrasts with many other ketone bodies, and their precursors, which are notoriously bad-tasting and thus difficult to tolerate when taken orally.Second,the(3R,3R‘)enantiomer is cleaved in vivo to form(3R)-hydroxybutyrate and (R)-1,3 butanediol. The (3R)-hydroxybutyrate is released immediately,giving a rapid effect following ingestion.The(R)-1,3 butanediol is converted in the liver to (3R)-hydroxybutyrate which is then released into blood.Overall this gives a favourable pharmacokinetic profile,since raised blood levels of the desired(R)-3-hydroxybutyrate are both achieved quickly and then sustained over a period of time following ingestion of the compound of the invention.”
Hi Dr. Attia,
I would like to know what is your VO2 max? On the basis data from this experiment, I guess 5 000 L/min (78 kg = 64.1 ml/kg/min)
But after your first 12-weeks experiment your VO2 max go down from 4 960 mL/min (63.5 mL/min/kg) to 4 350 mL/min (55.7 mL/min/kg). https://eatingacademy.com/how-a-low-carb-diet-affected-my-athletic-performance
I think it was caused maybe because you couldn´t ride more in low glycogen state. What you think?
Thank you
Respectively, did increase NK your VO2 max? Dr. Jack Kruse claims that NK increasing VO2 max, but it may takes 26-36 months. And it should be connect with cold thermogenesis (CT)- https://jackkruse.com/cold-thermogenesis-1-theory-to-practice-begins/
Do you practice CT?
So I have 3 Q:
What is your VO2 max?
Did increase NK your VO2 max?
Do you practice CT?
Thank you
I don’t practice CT, but I’m looking into WBC. Not sure if NK impacted (long term) my VO2 max. Also not sure VO2 max matters that much.
Over the past 2 years it has varied quite a bit by weight and training. “Good” is in the range of 5.2 to 5.3 L/min at 76 to 77 kg (67 to 70 ml/min/kg). “Bad” is in the range of 4.7 to 4.9 L/min at 78 to 79 kg (59 to 63 ml/min/kg).