You’ll recall from last week’s post I did a self-experiment to see if I could learn something about the interplay of exercise and ketosis, at least in myself. To understand this discussion, you’ll want to have read Part I of this post.
However, before getting to this, I want to digress and briefly address two unrelated issues:
- Some of you (about 67 or 68 as of this writing) have sent me various links to news reports released yesterday reporting on a study out of Harvard’s School of Public Health. I was planning to eventually write a post about how observational epidemiology is effectively at the heart of the nutritional crises we face – virtually every nutrition-based recommendation (e.g., eat fiber, don’t eat fat, salt is bad for you, red meat is bad for you) we hear is based on this sort of work. Given this study, and the press it’s getting, I will be writing the post on observational epidemiology next week. However, I’m going to ask you all to undertake a little “homework assignment.” Before next week I would suggest you read this article by Gary Taubes from the New York Times Magazine in 2007 which deals with this exact problem.
- I confirmed this week that someone (i.e., me) can actually eat too much of my wife’s ice cream (recipe already posted here –pretty please with lard on top no more requests for it). On two consecutive nights I ate about 4 or 5 bowls of the stuff. Holy cow did I feel like hell for a few hours. The amazing part is that I did this on two consecutive nights. Talk about addictive potential. Don’t say I didn’t warn you…
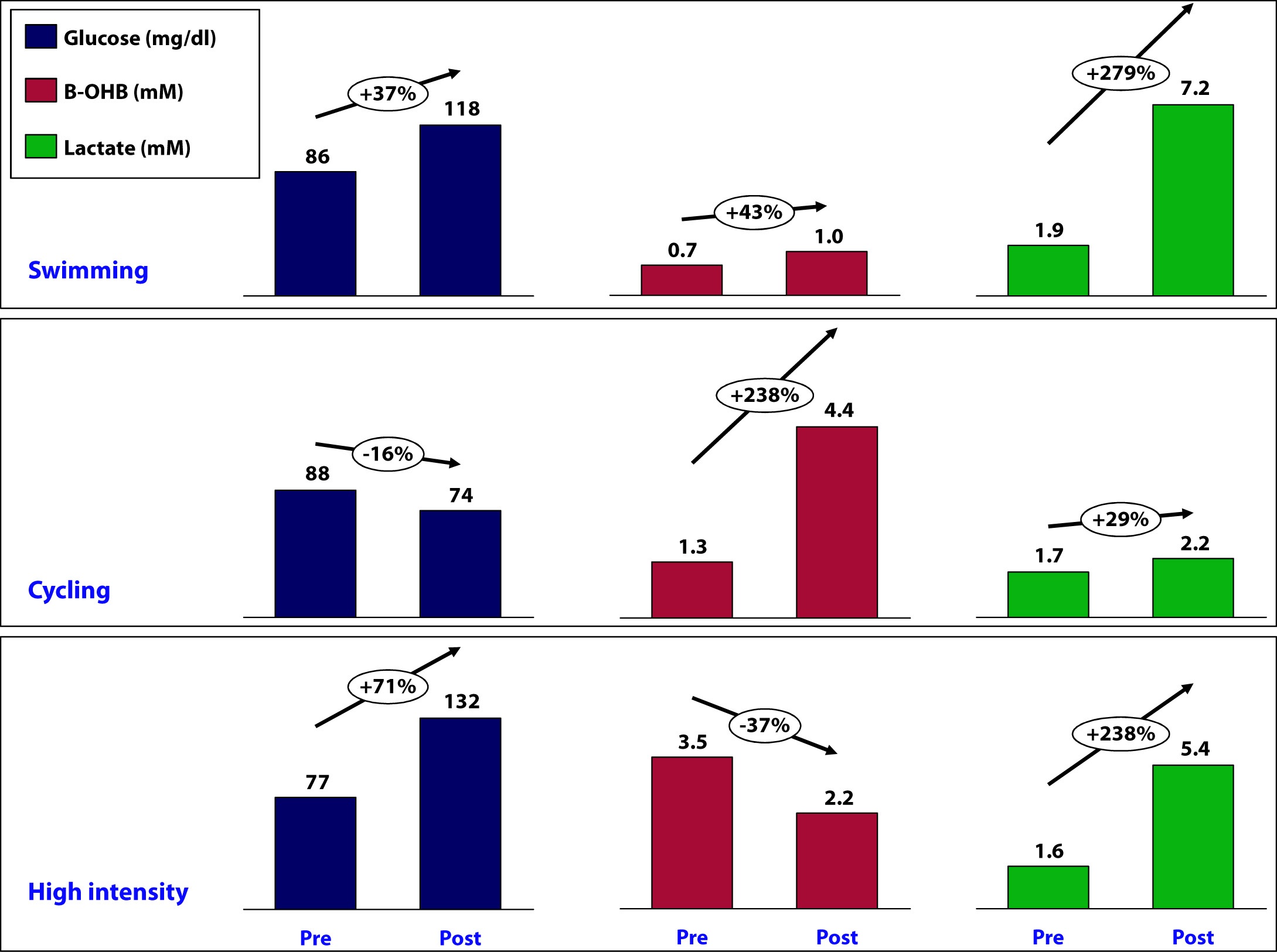
OK, back to the purpose of this post: How is ketosis impacting my ability to exercise? Here is the summary of the results from my personal experiment:
Let’s take a closer look at what may have been going on in each workout and see what we can learn.
Swimming
This workout probably produced the most lactate of the three workouts (we don’t know for sure because I only measured immediate pre- and post- levels without measuring in-workout levels). My glucose level rose by nearly 40% during this workout despite the fact that I did not consume anything.
How does this happen? Our bodies store glucose in the liver and in muscles in a “storage” form (a long chain of joined glucose molecules) called glycogen.
Whenever our bodies cannot access sufficient cellular oxygen, our metabolism shifts to a less efficient form of energy acquisition called anaerobic catabolism. During these periods of activity, we cannot oxidize fat or glycogen (i.e., use oxygen to harness the full chemical potential of fat or carbohydrate molecules). I will be writing in much more detail about these ideas in the next month or so, so don’t worry if these ideas seem a bit foreign right now. Just know that sometimes our bodies can convert fat or glucose to energy (efficiently), and sometimes we can only convert glucose to energy (inefficiently).
Because of my ketosis, and the metabolic flexibility that accompanies it, I only “require” that my body turn to glucose for energy under the most “stressful” forms of exercise – like I was doing a lot of during this workout. But keep in mind, my muscles CANNOT export one gram of the glucose they store, so any glucose in my bloodstream is either ingested (which I didn’t do) or coming from my liver, which CAN export glucose.
Furthermore, the stress of a workout like this results in my adrenal glands releasing a set of chemicals called catecholamines, which cause my liver to export even more of its stored glucose via a process called hepatic glucose output (HGO).
[As an aside, one of the major defects in type-2 diabetes is the inability of insulin to suppress HGO. In other words, even when not under the catecholamine stress that “should” lead to HGO, their livers constantly export glucose, which contributes to elevated blood glucose levels. The very popular drug, metformin, used often in type-2 diabetes, blocks this process.]
While I did experience a pretty large rise in lactate (almost 3x), my ketones still went up a bit. This could imply a few things:
- Elevated lactate levels do not directly inhibit beta-hydroxybutyrate (B-OHB)
- Mild elevations in glucose do not directly inhibit B-OHB
- Mild elevations in glucose do not directly inhibit B-OHB, if insulin is being suppressed (as is the case during vigorous exercise)
- B-OHB was suppressed, but we are only appreciating the net effect, which was a small increase (i.e., because of my MCT oil and activity, B-OHB levels were rising dramatically, but the rise was blunted by some other factor, such as HGO, insulin, and/or lactate)
More questions than answers from this workout, so on to the next workout.
Cycling
Despite this being a tough ride at several points, on average it was less stressful than the other two workouts and I spent the greater fraction of time in my aerobic to tempo (zone 2 to zone 3) zones.
A ride like this, however, is a great example of the advantages of improved metabolic flexibility that accompanies nutritional ketosis. My average heart rate during this 6 hour ride was 141. Prior to becoming ketotic, at a HR of 141 my respiratory quotient (RQ) was about 0.98, which meant I was almost 100% dependent on glycogen (glucose) for energy. Today, at a HR of 141 (with the same power output), my RQ is about 0.7 to 0.75, which means at the same HR and same power output as prior to ketosis, I now rely on glycogen for only about 10% of my energy needs, and the remaining 90% comes from access to my internal fat stores.
This is an important point. I will devote future posts to this topic in more detail, but I wanted to use this opportunity to mention it.
So what happened physiologically on this ride?
- My glucose levels fell, probably because I was slowly accessing glycogen stores for peak efforts (once my HR reaches 162 I become 50% dependent on glycogen) throughout the ride (e.g., peak climbing efforts, hard sections on flats), but my liver was not “called on” to dump out a massive amount of glucose in response to a catecholamine surge (and if it was, at some point during the ride, that amount of glucose had been used up by the time I was finished).
- B-OHB levels increased by about 2.5x – to 4.4. mM, which is pretty high for me. My highest recorded B-OHB level was 5.1 mM (also after a long ride). This confirms what my RQ data indicate — my body almost entirely relies on fat oxidation for energy for activity at this intensity. In the process, B-OHB is generated in large quantities, both for my brain and also my skeletal muscles (e.g., leg muscles). In reality, cardiac myocytes (heart muscle cells) also “like” B-OHB more than glucose and probably also access it when it is abundant.
- Lactate levels by the end of the ride were effectively unchanged though. Based on “feel,” I suspect I hit peak lactate levels of 8 to 10 mM on this ride during peak efforts, but I had ample time to clear it.
A few observations:
- I consumed 67 gm of carbohydrate on this ride (of which 50 gm was Generation UCAN’s super starch), yet this did not appear to negatively impact my ability to generate ketones. Technically, we can’t be sure this is the case, since I would have needed a “control” to know this (e.g., my metabolic and genetic twin doing and eating everything the same as I did, but without the consumption of super starch and/or without the bike ride). It’s possible that super starch did slightly inhibit ketosis and that my B-OHB level would have been, say, 5.0 mM instead of 4.4 mM. Metabolic studies of super starch show that it has a minimal impact on insulin secretion and blood glucose levels, hence the name “super” starch.
- Whatever impact peak levels of lactate production and hepatic glucose output had during the ride, they seem blunted by the end of the ride (and the ride did finish with a modestly difficult 1.4 mile climb at 6-7% grade, which I rode at a HR of about 150).
Since neither lactate levels nor glucose levels (nor insulin levels by extension) were elevated, I can’t really draw any conclusion about whether one factor, more than any other, suppressed production of B-OHB, so on to the next workout.
High intensity training
This sort of workout spans the creatine-phosphate (CP) system and the anaerobic energy system, and probably involves the aerobic energy system the least. I’ll write a lot about these later, but for now just know the CP system is good for very short bursts of energy (say 10-20 seconds) and recall the previous discussion of aerobic and anaerobic catabolism. In other words, this is the type of workout where my nutritional state of ketosis offers the least advantage.
- This workout saw the greatest increase in glucose level, about 70%. It is important to recall that during this workout I ingested water with a small amount of branched chain amino acids (BCAA’s – valine, leucine, isoleucine) and super starch, about 4 gm and 10 gm, respectively. I do not believe either accounted for the sharp rise in blood glucose and, again, I believe hepatic glucose output in response to a strong catecholamine surge attributed to this increase.
- Lactate levels also rose, though probably less so than during a peak swim effort. This suggests more of the effort in this workout was fueled by the CP system (versus the anaerobic system, which probably played a larger role in the swim workout).
- This was the only workout that saw a fall in B-OHB levels, which now offers some insight into what might be impacting B-OHB production.
Contrasting this workout with the swim workout draws a pleasant contrast: both saw a similar rise in lactate, but one saw twice the rise in blood glucose. In the former, B-OHB was unchanged (actually rose slightly), while in the latter, B-OHB fell by over a third.
This suggests – but certainly does not prove – that it is not lactate per se that inhibits ketone (B-OHB) production, but rather glucose and/or insulin. It is possible the BCAA played a role, and if I was thinking straight, I would not have consumed anything during this workout to remove variables. But I have a very hard time believing 3 or 4 gm of BCAA could suppress B-OHB. When you see hoof prints in the sand, you should probably think of horses before you think of zebras.
Conversely, there is some evidence that lactate promotes re-esterification of fatty acids into triglycerides within adipose cells. What does that mean in English? High levels of lactate take free fatty acids and help promote putting them back into storage form. This would prevent free fatty acids from making their way to the liver where they could be turned into ketones (e.g., B-OHB). In other words, we may be missing this effect because of my sampling error – I only sampled twice per workout, rather than multiple times throughout the workout.
So what did I learn, overall?
I think it’s safe to say I did not definitively answer any questions, which is not surprising given the number of confounding factors, lack of controls, and sample size of one. However, I think I did learn a few things.
Lesson 1
The metabolic advantages of nutritional ketosis seemed most apparent during my bike ride, evidenced by my ability to access internal fat stores across a much broader range of physiologic stress than a non-ketotic individual. (More on this in Lesson 4.)
Lesson 2
The swim and high intensity dry-land workouts suggested that my state of nutritional ketosis did not completely impair my ability to store or export hepatic glucose. This is a very important point! Why? Because, it runs counter to the “conventional wisdom” of low-carb (or ketotic) nutrition with respect to physical performance. We are “told” that without carbohydrates we can’t synthesize glycogen (i.e., we can’t store glucose). However, those who promote this idea fail to realize that glycerol (the backbone of triglycerides) is turned into glycogen, along with amino acids, not to mention the 20 to 40 gm of carbohydrates I consume each day (since my brain doesn’t need them). We know muscles still store glycogen in ketosis, as this has been well studied and documented via muscle biopsies by Phinney, Volek, and others. But, my little self-experiment actually adds a layer to this. Because muscle can’t export glucose (muscle lacks the enzyme glucose-1-phosphatase), we know that the increase in my blood glucose was accounted for by HGO – my liver exporting its glycogen. In other words, ketosis does not appear to completely impair hepatic glycogen formation or export. Again, we’d need controls to try to assess how much, if any, hepatic glycogen formation and/or export is inhibited. It’s hard to make the argument that being in ketosis is allowing me to swim and do high intensity training with greater aptitude, and as I’ve commented in the past, I feel I’m about 5-10% “off” where I was prior to ketosis for these specific activities, but at the same time, I could be doing more to optimize around them (e.g., spend less time on my bike which invariably detracts from them, supplement with creatine which may support shorter, more explosive movements), which I am not.
Lesson 3
Consuming “massive” amounts of super starch (50 gm on the ride), did not seem to adversely affect my ketotic state. My total carbohydrate intake for that day, including what I consumed for the other 18 hours of the day, was probably close to 90 gm (50 gm of super starch plus 40 gm of carbs from the other food I ate). This suggests one or two possibilities:
- Because of the molecular structure of super starch (I’ll be discussing this in the future, so please hold questions) and the concomitant metabolic profile that follows from this structure, it may not inhibit ketosis like other carbohydrate, and/or
- During periods of profound physical stress insulin secretion is being sufficiently inhibited that higher-than-normal amounts of carbohydrate can be tolerated without negatively impacting ketone production.
This is pretty straightforward to test, even in myself. I just haven’t done so yet.
Lesson 4
While it’s probably the case that my liver has less glycogen (i.e., stored glucose) at any point in time, relative to what would be present if I were eating a high-carb diet, it’s not clear this matters, at least for some types of workouts. Why? Take the following example:
- Someone my size can probably store about 100 gm of hepatic (liver) glycogen and about 300 gm of muscle glycogen at “full” capacity. This represents about 1600 calories worth of glucose – the most I can store at any one time.
- Before I was ketotic, my RQ at 60% max VO2 (about 2,500 mL of O2 per min consumption) was nearly 1.00, so at that level of power output (a pace I can hold for hours from a cardiovascular fitness standpoint) I required 95% of my energy to come from glycogen. So, how long do my glycogen stores last? 2,500 mL of O2 per minute translates to about 750 calories per hour, so I would be good for about 2 hours and 15 minutes on my glycogen stores.
- Contrast this with my ketotic state. Let’s assume my glycogen stores are now only half what they were before. Muscle biopsy data suggests this is probably an overly conservative estimate, but let us assume this to be the case. Now I only store 50 mg of hepatic glycogen and 150 gm of muscle glycogen, about 800 calories worth of glucose.
- In ketosis, my RQ at 60% max VO2 is 0.77 (at last check), telling me I am getting only 22% of my energy from glucose and the remaining 78% from fat. So, how long do my depleted glycogen stores last? Nearly 5 hours. Why? Because I barely access glucose at the SAME level of oxygen consumption and the same power output.
I know what you’re thinking…why is this an advantage? Just consume more glucose as you ride! It’s not that simple, but you’ll have to wait until my upcoming post, “What does exercise have to do with being in the ICU” to find out.
Going back to the black sheep example I open Part I of this post with, we know that at least one person in nutritional ketosis seems to make enough liver and muscle glycogen to support even the most demanding of his energetic needs.
Photo by Troy Oldham on Unsplash






Peter,
I’m a 40 years old runner. And im on ketogenic diet for a month now.
The problem is my heart beat is too much increased during my workouts.
Since i started this diet, i’ve notice a increased heart beat, at beggining making me stop the trainning. So, i give some time to complete the ketoadaptation. Since im in ketosys almost three weeks now, i wonder why this dont get better. Im checking my ketonas level and usually in the morning is 1.0-1.2 mmol, and in the evening as higher as 2.0-2.5.
Usually my heart beats doing interval trainning like 5×1.000m stays in the 168-175 range, and now 200-230.
And besides the higher heart beat i dont feel any symptoms.
Even in the long run where usually my heart beats stays in the 145-155 range, now goes up to 200. This is normal in the keto state???
Hard for me to troubleshoot, but makes me wonder if you’re deficient in sodium (i.e., unless you’re deliberately supplementing sodium, you will be), which in turn leads to depletion of potassium, and possibly magnesium. If sodium supplementation didn’t fix this, you should see your doctor.
Thanks for an amazing post.
I cannot get my B-OHB level to increase during exercise.
I fast 16-18 and and normally work out fasted, I have a great amount of B-OHB (2-5) measured with ketosticks when measuring in the morning.
After reading your blog i decided to supplement with BCAA 10g during fasted exercise, and experienced a drop in B-OHB levels immediately after training and several hours later. Tried dropping BCAA to 4-6g instead, but experiencing the same.
Maybe i misunderstood a part, but as far as I understand, even though BCAA increases glucose this happens in a way that should not kick me out of ketosis right, since they contain no carbs, and the amount is very small, so it has nothing to do with the amount of protein.
I Just ordered some MCT oil, and thinking about replace BCAA with MCT post workout.
1. Not all exercise increases BHB (assuming one is starting in ketosis); depends on energy demands. Steady aerobic activity at ~60-70% VO2 max appears “best” for this effect.
2. BCAA are consumed (read: should be consumed) in tiny doses, that it should little impact on ketosis.
Good day, Emil! I hope it’s alright if I give you my take on this.
BCAAs pre-workout inhibit the muscle catabolism that would occur during completely fasted training and promote muscle protein synthesis. Of course, you’re still going to have to consume a source of “whole protein” after working out for MPS to eventually fully occur. The BCAAs just “flip the switch” more or less, but don’t provide the raw material for new muscle to be built.
The reason that BCAAs suppress your BHB levels is because of the insulin response they cause; this is of course largely dose-dependent, but I would assume the insulin response is more acute rather than long-lasting. Still, I don’t think ketosticks offer nearly enough granularity that you could gather precise data about this.
During anaerobic exercise your blood glucose rises due to your liver releasing glucose into your bloodstream and your BHB levels will fall because of the glucose and/or insulin This is why you might note lower BHB levels after a workout . Consuming MCT oil would certainly right away raise BHB, but here’s the thing: just because your BHB might be low does not mean you’re automatically in a state of low-energy, because remember your blood glucose is still going to be elevated for a while. For this reason I don’t think it’s needed to take MCT oil post-workout in the way that someone that is hypoglycemic should eat a bagel. Make sense? Personally, I’d just eat something and go on with your day and soon enough your BHB will go back up as your blood glucose normalizes. Some people consume MCT oil before exercise in an attempt to increase their performance, but this is not something I’m familiar with. Although, on the subject of BCAAs and MCT oil, your decision to take one shouldn’t per se affect whether you take the other since they’re so different in their effect.
Also, if you’ve read the blog post by Peter from last year where he discusses his diet, you’ll note his observation that when he would consume his daily food intake in one sitting it would often knock him out of ketosis for a while (due to the insulin from the carb and protein load). You have to ask yourself, “should eating one meal a day be avoided for just that reason?” In my opinion that wouldn’t necessarily make sense.
In essence, what I’m trying to get across is I don’t think the goal should be to have as high BHB levels as possible at every moment of the day, but rather taking note of your energy levels and how good you feel to guide you.
Well said, TS.
Good Day TS,
Of course it is alright, – I am just glad there are so many knowledgeable people on this site, all interested in helping out and cracking the code for optimum health and performance.
Sorry for the long post now, but it is hard not to make it in to a good discussion when the possibility is there to learn something.
I tried to read most of the articles on this site, and read “Low Carbohydrate Perfomance” and several other sites regarding the subject, but it is easy to get confused with all the different studies, and a large flow of information sometimes with contradicting pieces. – I recently read a blog post regarding BCAA in fasted workouts and why it could be detrimental. Would love your take on that, the link is here: https://bit.ly/1d6YVNt
You might be right that Ketosticks don’t offer precise enough results to rest the case, I will have to wait for my Ketometer to show up in the mail (We don’t have these in Europe it seems) – If we assume that they are a just a tidy bit correct, it took about 24 hours until the ketone production was in the 1.5-3 range again after consuming BCAA on 2 different occasions.
I read the first of Peters posts regarding what he eats, and even though I fast 16-18 hours, I manage to get 2 large meals, and until now none of them seem to have kicked me out of ketosis, even with up to 100g of protein in one sitting – the carbs though are never beyond 10 grams in one sitting though.
I have always tried to maintain the optimum Ketose range for as long as possible to reap the benefits, but your post gave me something to think about, and moved my focus from maintaining a moderate/high BHB level, to instead notice how I feel and perform. And I guess as long as the carb restriction is still taking place, I receive all the benefits of the diet/lifestyle right?
I think what confuses me sometimes in my quest for the perfect path to eating, and life, is that there is a difference in most NATURAL in regards to human evolution and health, and the most OPTIMAL situation regarding, strength, performance and health, and maybe these paths aren’t always the same?
Since a caveman would never have access to BCAA, MCT oil or would have to supplement his daily grok food with 2g’s of sodium, even though he would most likely always be in ketosis?
I guess the human body and the evolution is not for creating super humans, able to gain muscle, lose fat and perform like a beast in every possible situation. Instead built for the ability to keep the species alive and re-produce ourselves?
Thanks again for your reply.
Greetings from Denmark
Dear Peter,
I found out that I had insulin resistance almost 5 years ago (I also have PCOS and I May have thalassemia (which could not be concluded) , now although i had managed to shed weight and it may seem that my body is functioning normally, I have some concerns about the education around insulin resistance. I have only just started re-visiting and re-educating myself on this & I must say finding your blog, TED TAlk and NuSI site have been an absolute godsend!
there is so much you have opened my eyes to, and although sometimes I need to read an article about 5 times to understand it, I feel I know more and so much better equipped to fight this and have started my blog to track my own findings…
I have two main areas of concern.
1. The prescription of diaformin/Metformin (which I have been on for 5 years now – and whom the endocrinologist says I must be on for the rest of my life (Which both concerns and frustrates me) whats your take on treating insulin resistance with diaformin/metformin? I really dont believe in it and want to wean my body off it but i am fearful of putting on weight as my body has become use to the help of this drug increasing my sensitivity to insulin, have I destroyed my metabolic system by being on this for so long?
2. The types of excersise one should do if they are insulin resistant. Now i’m not sure if i’m interpreting this right but it seems as though High intensity work outs actually increase glucose in the body thus being less beneficial to someone with insulin resitance . Thus is it better to do low intensity workouts in order to keep glucose production at bay (in the beginning of my diagnosis I was only walking first this in the morning before eating and thats all the exercise i was doing) and i managed to drop so much weight.
Now however , I have gained weight (but still at normal weight range) but i am going to the gym almost everyday, lifting weights but also doing high intensity workouts, however I don’t seem to be budging in weight)
Could there be a relation between the intensity of exercise and glucose production ? and which is best for someone with insulin resistance?
I understand you are a very busy human so ANY guidance would be greatly appreciated.
Also if you are reading this I just wanted to thank you for giving hope that there is a greater science out there, one that explains the WHY and the HOW and doesnt mask the proxys but treats the underlying issues!
THANK YOU!
Dear Peter:
Amazing blog. Thanks very much.
I’m puzzled by something.
1. You and others have asserted, and it’s certainly widely believed, that those on calorie-restricted low-carb diets initially lose “water weight.” I believe the logic is that the body first makes up its energy deficit by consuming the glycogen in the liver and muscles, and that this glycogen (say 500g) is bound to a lot of water (say another 1500g).
2. But, you’ve also written (and cited studies) showing that glycogen is still stored in the muscles even under ketosis, presumably from glycogen produced by the liver from whatever carbs are consumed and whatever else it can scavenge. Presumably with even a few hours of calorie surplus, glycogen stores would begin to be recharged.
I’m not sure I understand how both of these mechanisms can be reconciled. In sum, how can there both be “water loss” and replenishment of glycogen on very low carb diets? Is it that glycogen stores are only replenished under ketosis when and if the body has a calorie surplus? Does that calorie surplus have to persist over days and weeks? For instance, is it that “Biggest Loser” contestants will never replenish glycogen until they stop running huge calorie deficits; they always have empty tanks? If so, can a cyclist never both have a full glycogen tank and be trying to lose a few pounds (my situation)?
The water loss is mostly plasma water loss. Glycogen loss occurs, but it probably rebounds to about 2/3 “normal” levels. The latter is a tiny amount of weight. The former can be more significant.
Hi Peter,
I have enjoyed reading your blog and I am trying to figure out the best nutritional protocol for keto running/training. I’m an ultra endurance athlete and typically run 5 – 6 days per week. In addition, I also do core and body weight exercises.
As a new keto adapted runner, I was wondering if you could share advice on what to eat both pre-workout and during workouts. I’m a little confused on when I should run with no pre-workout meal and when I should consume calories during a workout.
If I understand correctly, it looks like you would recommend something similar to this protocol for a long run ….
“About 90 minutes prior to the ride I consumed 4 eggs fluffed with heavy cream, cream cheese, coffee with heavy cream, and my usual 40 mL of MCT oil.”
During workout consume ….. single serve cream cheese, UCAN & nuts.
How about for intervals/track repeats? Utilize the protocol that you used for your swimming intervals?
“During this workout I consumed nothing and prior to the workout I consumed my usual 40 mL of MCT oil.”
How about tempo runs?
What is the optimal strategy on using BCAA’s? Do you recommend using UCAN pre-workout for high intensity runs (e.g., intervals, tempo) or just during long runs?. Thanks in advance for taking the time to answer my questions.
Dean
Dean, too complicated for quick response. I do most of my workouts fasted and only consume BioSteel’s BCAA (HPSD) in-workout, since I do nothing over 3 hours these days.
Dr. Attia, thank you for the work you have done. I have been experimenting with myself pre and post workouts. I have been following a strict carbohydrate reduction (less than 50 grams a day) paleo lifestyle for a while now. When testing my blood glucose (for fun) before high intensity (kettlebell swings, push ups, overhead lunges, burpees etc) short duration workouts following a fasted state of 16-17 hrs my blood glucose will range 75-85 mg/dL. Post workout my blood glucose has spiked to 150-168 mg/dl. What are your thoughts? My first question is does that seem “normal”. My other questions is: will consuming food (hefty serving of mixed green, avocado, green/kalamata olives, lots of EVOO, few table spoons of heavy cream, protein under 35 grams etc. ) 10-15 minutes post workout with an elevated blood glucose level have negative effects on a ketoic state?
Discussed in this post or previous…hepatic glucose output.
Doctor,
First off, I find myself returning to this post often because of the evaluation of the data. I’d like to see more like this.
Second, I stumbled across this article.
https://www.popularmechanics.com/science/health/life-extension/debunking-the-3-biggest-exercise-myths#slide-2
which states “For example, when your body burns fat or carbohydrates to fuel muscles, one of the byproducts is H2O.” combined with your description of Krebs Cycle in a previous post, makes me wonder; have you experienced, or seen any impacts, on dehydration now that you are in Ketosis?
I’ve always been pretty resistant to dehydration, relative to a “normal” person, so I have not really noticed a change one way or the other. I’ve heard theoretical arguments, but seen no data.
Hey Peter,
I am wondering if it is possible that hepatic glucose output can hinder one’s ability to get into, or stay in nutritional ketosis? Are HGO and Ketosis fighting one another?
I have been eating very low carb/high fat for about a year. Early on I had no trouble getting into and staying in nutritional ketosis, but lately it seems that even with very low carb intake I cannot seem to get there. One of the things that I did notice is that my morning glucose numbers were higher than the prior night before I went to bed. I have also been less physically active lately, and I am sure that has something to do with it as well.
Thank you for all of the great work that you do
Short answer, yes.
Dr. Attia,
Apologies for resurrecting this post from years ago! I’ve used ketogenic diets in the past with good success, but this is the first time I’m doing it in conjunction with serious training. I’m on about 3.5 weeks now, down 13lbs, and producing solid ketones according to the dipsticks. All good, right? I can’t train like I used to. As soon as I start running or cycling, my legs start burning as if they were filled with lactic acid. My run pace is now several minutes per mile longer than it used to be, and my heart rate is absolutely pegged, regardless of pace/effort. Spent an 8 mile run yesterday at an average 178bpm, and slower than molasses.
To me, it feels like my body just can’t access adequate energy on demand during exercise, but I feel fine any other time. Any thoughts? Thanks for your input.
Sean
Under extreme exertion it takes much longer than 3 or 4 weeks to adapt. Took me 12 weeks for first big improvement, then about 18 months to exceed where I was at outset for top-end anaerobic power.
Just read this article:
https://www.grindtv.com/outdoor/excursions/post/sami-inkinen-to-row-ocean-with-fat-for-fuel/
This should be an interesting journey!
Dr. Attia:
I am trying to get a base line on all of this information. Is it appropriate to say a 58 year old woman who would like to lose weight and maintain a workout that involves weight lifting and aerobic style exercise (five-six times a week for 30 minutes) could do a low to very low carb diet without fear of ketosis problems? I am a healthy “normal” female who is extremely efficient when it comes to storing and keeping my stored fat :(. I would like to say my metaboism is sluggish but I don’t know that for sure. I have no health issues. Any insight on this would greatly be appreciated.
Hey, great website you have here man.
I’m an athlete that comeptes in brazilian jiu jitsu, and currently am doing rock climbing about 5 times a week, and I am on a consistant 30 grams of carbs a day. I always have great energy (although I do take MP Assault prior to exercise, which has a few grams of carbs and other things).
what I wanted to ask (and maybe recommend) to you is something called “miracle berry”. It’s a berry that has a specific protein that attaches itself to your tongue’s sweet receptors, and activates them when an acid makes contact. So basically, you chew and such on the berry for about 60 seconds, and for the next 1-2 hours, anything sour you eat tastes sweet.
I have been drinking pure lemon juice + water that tastes like a very sweet lemonade. I also make LOADS of drinks with lemon in them that taste completely like desserts.
I’m soon to be trying making an icecream with lots of lemon juice, which should also taste like 100% sweet icecream.
I’m surprised more lchf/keto sites don’t talk about this berry? Have you heard of it? And if you have, why is it not more talked about?
Here’s a wiki on the fruit in question:
https://en.wikipedia.org/wiki/Synsepalum_dulcificum
P.S. I know lemon juice has some carbs, but it’s low enough that I can accomodate it into my diet without falling off keto (I’ll just cut back on some other source for the day I eat the berry).
Peter, I’m passionate about nutrition and exercise, and I really like to understand the science behind everything, and your blog is in-depth and didactic, you’re doing an awesome job here.
I started keto a while ago, and I’m taking some green tea extract to help with the fat burn, along with albuterol.
I now know that catecholamines, which the extract has a lot of, stimulate glycogen release through the liver.
Do you think I”m doing more harm than good by taking the extract? I’m using ketostix to get a rough estimate of where I’m at (I”ve found the metallic taste in my mouth to be a better indicator of ketosis, though), and all of the markers seem normal, so I”m still ketotic, but I’m looking to optimise fat mobilisation.
Thanks for your time! Also, what’s your opinion on sugar alcohols?
Nevermind, I read the bottle again and it’s high in CATECHINS, made me wonder why green tea would have epinephrine, haha.
Hey Peter, I’m also going to raise a year-old post, but this is also my first time reading it.
Apologies in advance for all the detail. The crux of my question is the impact of exercise and keto-adaptation, especially in the early stages, and especially relating to heart rate.
I am five weeks in. Started at 80kg and am down to 74kg – target is 68kg (which would be 5% body fat). My fasting glucose mean is about 85 (testing at home) and fasting ketones have been up to 1.0-1.5 on average (for past week). Carbs are 20-25g per day, mostly foundation veggies. And eating about 100/120g protein, and 100-140g fat. No cheating so far with food, altho I have had two IPA’s in those five weeks …
I did get a few “flu” symptoms that I am countering with 2000mg of sodium (stock cube) in addition to salt in food, and two 99mg potassium tablets, as well Primal vitamins and drinking 40-60oz water. “Flu” has largely cleared up. The one thing that’s persisting is a weirdly high heart rate.
As context, when in good cycling shape (I’m a Leadville 100/Cape Epic rider), I have a resting HR of about 50, and a field-tested LT HR of 162 at 320W at about 74kg. As of a week prior to the shifting to Atkins induction, my LT power had dropped to 290W with LT HR @ 165bpm at 80kg, and resting HR of 54. I don’t ride anywhere near as much these days as a relatively-new parent.
As of yesterday morning, my resting HR was 75-80bpm – and I can really feel it, and it woke me up Sunday night. When riding on my spin bike at 220W average, I am up at 165bpm – again, I can really feel it. The same was true on a 50km tempo ride this weekend – av HR of 169 @ 214W (but RPE was probably a 7 at the most). That compares to 155bpm @ 203W for the same ride two weeks ago.
I drank about 80oz of water yesterday and it seemed to help my HR and brought it down for a while, so I am wondering if this is simply a case of not enough fluid, or whether its related to minerals?
Have you ever had ketosis kick your resting and exercise HR so noticeably up like this?
Hi Peter,
Just to add to Adrian’s comment above. Mine was a similar story (albeit with less impressive wattage). Now I’ve been in ketosis for over 10 months and although the “during the exercise” HR numbers have come down to their historical levels – my resting HR is still about 15bpm above what it used to be prior to getting started on the ketogenic diet.
Thanks for your time!
Dear Peter,
Thank you for such an amazing website.
My mum has always been overweight even when she was in an almost starved state (living on water and some rice). Now I have a lot of trouble convincing her that her foods are too high in carbs (many Korean foods are low in fat, protein and high in simple carbs such as potatoes, flour, rice etc).
Recently she’s been having a lot of issues such as high cholesterol levels, knee problems due to her weight but she thinks they are the result of consuming too much red meat. On an average week she consumes probably one small portion of red meat or none so I honestly do NOT for a second believe that red meat is causing her any problems. Her low-fat high fructose yogurt, fruit juices, sugary muesli bars, wheat biscuits are behind all of this.
It can be very frustrating to see someone you love follow such terrible guidelines learnt in their childhood (at school) and risk their health but I am making slow progress all thanks to your highly detailed blog. My parents still think I’m a little crazy but they are slowly making changes.
I just wanted to thank you since I’ve been following your blog for a year now and have never left you a comment. Just knowing that someone actually puts their time and money into sharing critical information (all nicely laid-out) for others for free is an inspiration in itself.
Thanks again!
Thank you, Marina. Very kind of you to say this.
Hi Peter,
I’m a giant fan of your personally and professionally. You’re definitely a pioneer in the field and someone I look up to. You’re one of the big reasons I got into ketosis in the first place. I’ve studied a lot of your work and also some of Phinney’s work. I am currently a professional soccer player nearing the end of my prime and have started experimenting with ketosis to see if it can take me to another level physically during my matches.
I have heard you speak of insulin being the driving factor of ketosis, but it is a popular belief that lack of liver glycogen is the driver of ketosis. And here, you say that your higher glucose levels are a result of emptying of liver glycogen (therefore, confirming the former of the two above theories of insulin and not liver glycogen being the determinant factor). My question is how do we know this glucose increase isn’t a result of muscle/internal catabolism to achieve this higher glucose level instead of hepatic glucose.
Would love to hear back from you. Thanks again for trail-blazing my friend.
Kyle K.
Kyle, I think both play a role, actually. Even in complete starvation (or hypocaloric KD), the body’s stores of glycogen remain about 50% full (largely due to GNG from glycerol in the case of starvation, and probably a combo of this and protein in the case of KD).
I favor the HGO argument for the simple reason, that even in starvation, if you administer glucagon to a person, glucose levels rise (implying the glucose is coming from the liver).
Great. Thank you so much Dr. Attia,
I know Volek/Phinney have proved that muscle glycogen stays around 50% full, but I haven’t seen anything conclusive around hepatic glycogen levels. I have been doing a little experimenting on myself lately through my training. I also think about the reasoning of our evolutionary mechanisms when looking to answer these questions with no conclusive answer our there. I just can’t rap my head around the idea that the liver would burn fats if it still had some glycogen. I do think lactate and the Cori cycle can definitely play a role in higher blood sugar levels during exercise. I do see what you are saying about glucagon, but wouldn’t the body be able to produce glucose from degradation of muscle and GNG from the resulting amino acids to accommodate to glucagon? So the same mechanism our body would use if on a HCLF after glycogen had been depleted.. I’d rather this wasn’t the case, but just trying to wrap my head around it.
Tough to justify liver biopsies, but the glucagon experiments imply hepatic glucose output (since muscles can’t release glycogen into general circulation).
Peter,
I have been diagnosed with Metabolic syndrome and have gone on 1000MG Metformin, and a ultra low carb diet. My Triglycerides are close to 700 and my diet is fairly clean. Obviously, this is genetic as I cannot loose a pound even if I ride 120 Miles a week. Interesting write up on athletic performance in ketosis. I always assumed you had to consume carbs to have enough energy for duration training. What your saying is your liver has the ability and store to convert glucose while maintaining ketosis and you don’t give up much in the way of energy stores.
Amazing!
What supplements should one be on if you are endurance training in nutritional ketosis?
Does your body need less endurance training to loose weight in ketosis?
I don’t know the answer to your question. It probably varies by person, though.
Dr. Attia,
I’ve scanned back thru several posts looking for a reference to a BG point which stops fat burning and if there is one I have missed finding it and apologize. I was told a fat burner would bonk cycling or running if their BG got over 100 mg/dL. This was later amended to be 100-120 mg/dL (crossover zone). Is this in fact true, to your knowledge? I was told fat burning quit and I was only burning glucose. Being a person in dietary ketosis (~30 grams of carbs per day, never more than 40 ever in the last 2 years) I don’t believe this and believe that this information was written not with the possibility that a ketogenic diet being used at all times even while training for a sport. I feel like with most other studies, People on long term true LCHF diets are not included in the performance studies.
I feel this is probably more complex than just a simple YMMV where a person crosses over, but can you let me know if my informer is wrong or right and maybe point me to a source of further reading.
Thanks for the blogs, looking forward to more, especially the ICU one I didn’t run across yet.
Not sure it’s that “simple.” That’s only one part of it. Look at the fat flux post or a detailed explanation of lipolysis.