Alton Barron is an orthopedic surgeon specializing in the shoulder, elbow, and hand. In this episode, Alton breaks down the anatomy of the upper extremities and discusses the most common injuries associated with this area of the body. He explains in detail how he examines the shoulder, elbow, and hand to find the source of the pain and lays out the non-surgical and surgical treatment options as well as the factors that determine whether surgery is appropriate. Additionally, Alton describes the surgical procedures that, when done appropriately, can lead to tremendous reduction of pain and improvement in function.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
(See “Selected Links” section at the bottom of show notes for a list of all YouTube video clips created from this discussion)
We discuss:
- Alton’s path to orthopedic surgery [3:45];
- Evolution of orthopedics and recent advances [8:45];
- Anatomy of the upper extremities [13:30];
- Rotator cuff injuries, shoulder joint dislocation, and more [21:15];
- Peter’s shoulder problems [31:30];
- The structure of the biceps and common injuries [35:30];
- Labrum tears in the shoulder and natural loss of cartilage with usage and time [38:15];
- Shoulder evaluation with MRI vs. physical exam, diagnosing pain, and when to have surgery [41:30];
- How anatomical variation can predispose one to injury and how screening may help [50:30];
- Pain generators in the shoulder, and the important nuance of the physical exam [56:00];
- Frozen shoulder [1:05:15];
- Shoulder pain that originates in the neck [1:11:15];
- Surgical treatments for a labral tear, and factors that determine whether surgery is appropriate [1:16:00];
- Repairing the rotator cuff [1:29:15];
- Are platelet-rich plasma (PRP) injections or stem cells beneficial for healing tears? [1:38:15];
- Repair of an AC joint separation [1:45:15];
- Total shoulder replacement [1:55:45];
- The elbow: anatomy, pain points, common injuries, treatments, and more [2:05:30];
- How Tommy John surgery revolutionized Major League Baseball [2:17:15];
- History of hand surgery and the most significant advancements [2:22:15];
- The hand: anatomy, common injuries, and surgeries of the hand and wrist [2:29:30];
- Carpal tunnel syndrome [2:40:00];
- Other common injuries of the hand and forearm [2:47:15];
- Grip strength [2:55:15];
- Arthritis in the hands [2:59:30];
- Trigger finger [3:07:45];
- Nerve pain, numbness, and weakness in the upper limbs [3:14:00];
- The Musician Treatment Foundation [3:22:00];
- Gratitude and rucking [3:34:15]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Alton’s path to orthopedic surgery [3:45]
- Peter did general surgery, but outside of trauma, he knows very little about orthopedics
- This it probably true for a lot of doctors
- How much more is that true for patients?
- Orthopedics is a broad field and pretty specialized at the same time
- Alton agrees, in medical school we only do a subset of rotations
- He knows nothing about urology, brain surgery
- It depends on the luck of the draw, on what we get exposed to
- Then we narrow ourselves down like a funnel in terms of knowledge
- There has been a knowledge explosion for the past 2 decades in terms of research and new science
- There are subsets of orthopedics and then there are subsets of shoulder surgery that involves just research versus just clinical practice
- Alton’s well informed patients ask him about things, and hopefully he knows a lot of it, but he doesn’t know all of it
- Some of them are very good at looking at true scientific articles and approach him with new articles
- He is learning every week from his patients about shoulder surgery
When you went to med school, did you think you wanted to be an orthopedic surgeon?
- He didn’t know
- Alton had a very circuitous path
- He was an engineer at UT in Austin
- Mechanical and biomedical
- His dad was an engineer so he went that way
- At the end, he wasn’t sure about going into industry
- On a whim he went to dental school for a year
- He had 2 uncles that were dentists
- He didn’t like that at all, but he loved the science
- He was exposed to the anatomy of the entire body
- His anatomy instructor at dental school was a MD, PhD and when he confided in her that he was leaving, she suggested he try medical school
- He came back to Austin, TX and painted houses for a year, then applied to medical school
- In med school he loved invasive cardiology
- All the aspects of the physiology and the electricity going on in our bodies
- Then he was exposed to orthopedics and knew he liked it
- It felt so natural putting things together, like a jigsaw puzzle
- It felt all in perfect line with his engineering background
At the time when you went through orthopedics, was it common for people to also do a fellowship after 5 years of residency?
- It was
- He went to Tulane, this was pre-Katrina
- It was a big program
- They had 8 residents per year
- At the time, about 4 going to general practice
- Fellowships were not ubiquitous then
- Now they’re almost mandatory because you need to have a special interest because the groups you’d apply to work for want you to have some subspeciality
- Peter agrees, this is the case in medicine
- Even if you did general surgery and didn’t do a fellowship, you’d be hard pressed to go into the community and do everything
- You’d probably focus on one part of the body
Where did you do your fellowship?
- Upper extremity
- He did a shoulder fellowship at Columbia in New York
- Then he did a hand fellowship at Roosevelt Hospital in New York
- 2 separate fellowships
- Most people didn’t do that at the time, but he just really like both very much
- He dabbled with spine during residency
- The reason he wanted to do upper extremity is because there’s nothing cookie cutter about it
- There were very few cutting jigs, very few linear things
- There’s so much variability in the upper limb, both anatomy and the specific pathology
- It was more creative for him
Evolution of orthopedics and recent advances [8:45]
What year did you finish your training?
- He started practice in ‘96
When did minimally invasive orthopedic surgery become common for joints?
- Peter recalls, there was a day when the shoulder surgery he had would have been done with a big open incision
- Knee arthroscopy was the first big arthroscopic realm to develop
- Dick Asbury was hugely innovative in that space
- Shoulder arthroscopy was primitive by the time Alton was in residency
- They had the basic equipment to get into the shoulder, but they couldn’t do much
- By the time he finished his shoulder fellowship, they were doing open shoulder arthroplasty
- He was at one of the meccas of shoulder surgery, so everything advanced was being done there at the level it could be done
- But it was open shoulder arthroplasty
- The incisions were smaller but it was still open
- They did open instability repairs, open labral repairs
- They didn’t appreciate the slap tear
- They knew it existed, but they didn’t know the impact
- There were certainly no arthroscopic repairs of the labrum (see the figure below) except these early devices where you’d get in there, see it, and you’d just drill a little hole and mallet in this big broad tack
- That was just so primitive, and they would fall out
- They had a high failure rate, but that was the state of the art at that time
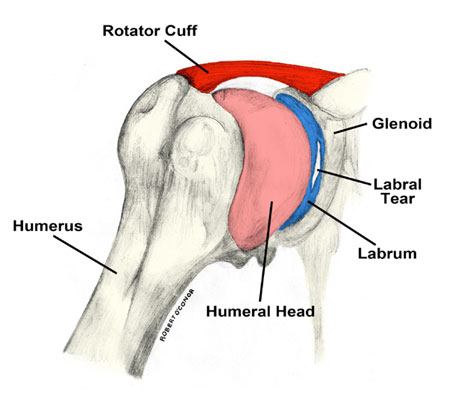
Figure 1. Shoulder anatomy and labrum. Image credit: Hospital for Special Surgery
Was any of this being done in clinical trials?
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Alton Barron, M.D.
Alton Barron earned his undergraduate degree in Engineering with honors from the University of Texas at Austin. He earned his medical degree from Tulane University, where he also completed his orthopedic surgery residency. He was awarded fellowships in shoulder surgery at Columbia-Presbyterian Hospital and hand surgery at Roosevelt Hospital.
Dr. Barron is a board certified, fellowship-trained shoulder, elbow, and hand surgeon based in New York City since 1996. He specializes in both routine and complex problems of the upper limb, including all sports injuries, severe arthritis requiring shoulder and elbow arthroplasty, nonunions and malunions of bones, and severe nerve injuries requiring tendon transfers and microsurgery. He is a Clinical Associate Professor of Orthopedic Surgery at NYU Langone Medical Center, and a Senior Attending Physician at the Roosevelt Hand to Shoulder Center at OrthoManhattan. He is Medical Director of Pinnacle Surgery Center in Austin and has clinical practices in both Austin and Manhattan. He is affiliate faculty in the department of Department of Surgery and Perioperative Care at The University of Texas at Austin Dell Medical School.
Dr. Barron has been teaching and conducting research for his entire career and has numerous peer-reviewed journal publications, book chapters, and national presentations. He is a member of multiple professional societies, including the American Academy of Orthopedic Surgeons, American Shoulder and Elbow Surgeons, American Society for Surgery of the Hand, and New York Society for Surgery of the Hand, for which he served as Treasurer (2007-08) and President (2011-2012). Dr. Barron was a Fordham University Team Physician from 2002-2014 and has been a treating doctor for the New York Philharmonic Orchestra and Metropolitan Opera for the past 17 years. He is a consultant for the New Jersey Devils NHL team. He previously held academic teaching positions in Orthopedic Surgery at Columbia College of Physicians and Surgeons from 1998-2014, and the Mt. Sinai Icahn School of Medicine from 2014-2015. He was a Senior Attending Physician in the Department of Orthopedic Surgery at St. Luke’s-Roosevelt Hospital Center from 1999-2015, and a Senior Attending Hand/Upper Extremity Surgeon at the CV Starr Hand Surgery Center at Roosevelt Hospital, the oldest teaching hand service in the country, from 1996 through 2015. He is co-author, with Carrie Barron MD, of The Creativity Cure: How To Build Happiness with Your Own Two Hands published by Scribner in 2012, and has been Chairman of the Board of Trustees at Post University since 2012.
In 2017, Dr. Barron founded the Musician Treatment Foundation. This nonprofit is the first of its kind, in scope and breadth, and is dedicated to the healthcare needs of professional musicians. The MTF mission is to: 1) Provide direct orthopedic shoulder, elbow, and hand surgical and nonsurgical care for the uninsured and underinsured musicians of Austin, New York, and beyond. 2) Educate musicians (both amateur and professional) on preventive medicine techniques that will minimize or avoid musician-specific injuries. 3) Conduct research and gather outcomes data into the unique diagnostic and treatment issues facing all musicians and to disseminate this knowledge throughout the world. 5) Create the first cloud-based platform to allow state of the art remote preoperative, postoperative, and non-operative continuity of care, and to provide real-time consultation and treatment recommendations and referrals worldwide. 6) Build the first physician-surgeon network in the world dedicated to providing the care for needful, injured and ailing musicians. [altonbarron.com]
Follow Alton here:
- Instagram: @draltonbarron
- Facebook: Dr. Alton Barron
- Twitter: @altonbarronmd
Follow Musician Treatment Foundation here:
- Instagram: @mtfusa
- Facebook: Musician Treatment Foundation
- Twitter: @mtfusa



