In this “Ask Me Anything” (AMA) episode, the conversation focuses on cancer screening, a topic often shrouded in confusion yet crucial to understand given that early identification of a cancer is an essential part of survival strategy. Peter examines the arguments both for and against cancer screening, including addressing why some trials may show no benefit to screening. He then delves into the various screening modalities available for different cancers, highlights the pros and cons associated with each, and explains how to interpret the results. Additionally, Peter provides guidance for navigating outside of the relatively narrow and confined screening guidelines for various types of screening tests.
If you’re not a subscriber and listening on a podcast player, you’ll only be able to hear a preview of the AMA. If you’re a subscriber, you can now listen to this full episode on your private RSS feed or on our website at the AMA #56 show notes page. If you are not a subscriber, you can learn more about the subscriber benefits here.
We discuss:
- Why understanding cancer screening is crucial [2:45];
- The prevalence of cancer diagnosis and mortality rates [4:30];
- Why cancer screening and early detection is such an important part of the strategy to survive a cancer diagnosis [11:00];
- The data on how cancer screening impacts survivability of cancer [16:30];
- Inconsistencies between cancer screening trials regarding benefits to survival rates [25:45];
- What are some of the reasons why clinical trials don’t always improve cancer-specific mortality? [30:15];
- What are the arguments against population-level cancer screening? [42:00];
- Cancer screening outside the recommended guidelines: risks and benefits, interpreting results, and other considerations [46:00];
- Understanding sensitivity and specificity when reviewing screening results [52:30];
- Risks and complications associated with colonoscopies [55:45];
- Cancer screening modalities: options for cancer screening both within standard recommendations and beyond [58:30];
- The strengths and limitations of various types of cancer screening [1:02:15];
- Understanding positive and negative predictive value using sensitivity, specificity, and pretest probability [1:11:45];
- Factors that influence an individual’s pretest probability of cancer [1:13:45];
- How to interpret cancer screening results [1:18:15];
- The importance of having an advocate when considering out-of-guideline cancer screening tests [1:23:30];
- How stacking multiple cancer screening modalities can decrease the risk of false positives [1:29:30];
- Advice and guidance for making decisions related to cancer screening [1:31:15]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Why understanding cancer screening is crucial [2:45]
Today’s AMA is going to focus all around cancer screening
- Is it important?
- Is it beneficial?
- Sometimes articles in the news claim cancer screening is beneficial
- Others talking about how studies came out in cancer screenings not beneficial
- This creates a lot of confusion for people around this topic
Today’s AMA will go through:
- Cancer screening in general
- the cases for and against cancer screening
- why some trials may show benefit while others don’t
- What modalities do people have
- the different options for cancer screening, including the pros and cons of each of them
- also what should people think about when they get cancer screening, whether it’s within traditional guidelines or what we’re seeing more so now is if people are paying out of pocket outside of traditional guidelines
The prevalence of cancer diagnosis and mortality rates [4:30]
Cancer incidence and mortality rates
- A rough, but not totally accurate, way to say this is that a person in the US has a lifetime incidence of cancer about one in three and about half the time it’s going to be fatal
- Said another way, one in three chance of getting cancer in your lifetime, and one in six chance of dying from cancer
- However, this is an underestimate
- What are the most recent numbers?
- Men have a lifetime incidence of just under 41% and indeed about half of those are fatal, i.e., a 20.2% lifetime risk of dying from cancer
- For women, the numbers are slightly better, 39.1% lifetime risk of cancer diagnosis with just under half of those being fatal, so a 17.7% of dying from cancer
- A more relevant way to look at this:
- Cancer is the second leading cause of death in the United States and globally (ASCVD is #1)
- And it’s probably more maybe insightful to compare this through decades of life
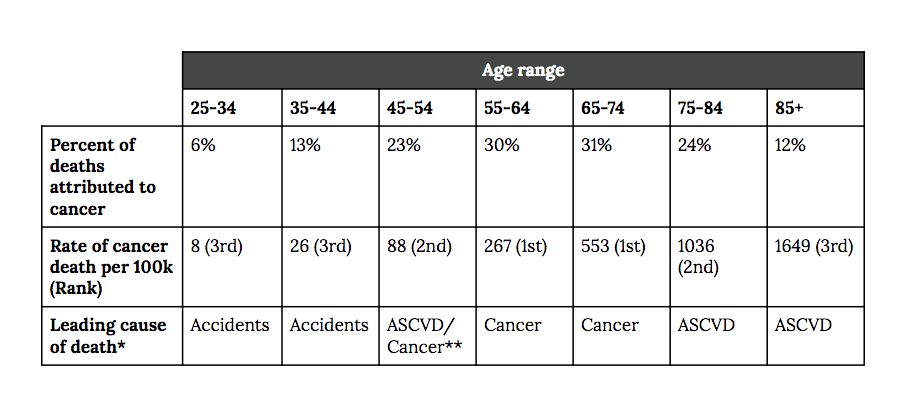
Figure 1. Source: CDC report on causes of death in 2021, omitting deaths attributable to COVID-19 where applicable.
- This table is organized by decades—we’re looking at people aged 25 to 34, 35 to 44, et cetera, all the way up to 85+
- And we’re looking at three things
- 1) What percentage of deaths in that decade are attributed to cancer?
- 2) Then we’re looking at the actual rate of cancer death.
- And this is always done in deaths per 100,000
- So what is the number of deaths per 100,000 and what is the rank of cancer relative to other types of death within that decade?
- 3) And for the cases where cancer is not number one, what is number one?
Let’s start at the lowest end of the spectrum: This is lowest in terms of lowest mortality because the number you really want to anchor to is what’s the absolute death rate, and that’s going to be in how many cases per 100,000
- In that first decade, 25 to 34, cancer accounts for 8 deaths per 100,000 individuals
- Not many people fortunately are dying that young… it represents 6% of total deaths ranking third
- There are two things that rank significantly higher and not surprisingly, the number one cause of death in that demographic is accidental death (typically overdose)
- You go up to the next category, 35 to 44, the percent of deaths attributed to cancer goes up from 6 to 13% and the rate of death goes up threefold
- Goes to 26 deaths per 100,000
- It is still the third leading cause of death, trailing accidental death (overdose, typically)
- We go into the next decade, 45 to 54, cancer now accounts for 23% of all deaths in someone Peter’s age
- The rate of cancer deaths again jumps sharply from 26 to now 88 per 100,000, and it technically ranks second (asterisk here because here is where cancer and ASCVD are constantly switching with each other)
- It ranks first or second here, and it’s either ASCVD or cancer that are in the number one spot
- Then accidents tends to fall to number three
- So you go one decade up, 55 to 64, the percentage of deaths attributed to cancer is 30% of deaths
- By the way, this is almost the maximum share of cancer deaths you’ll see
- It now rises to the number one cause of death in that age group, and it now accounts for 267 deaths per 100,000
- Go up another decade, 65-74, and it basically is the same story
- It’s 31% of deaths attributed
- It is the leading cause of death, and it now has doubled to 553 deaths per 100,000
- Now you’ve made it to the age of 75, and what happens?
- Well, it turns out that other diseases are exploding, and so cancer now falls to second
- ASCVD takes over, but cancer still accounts for a quarter of deaths, but the absolute rate continues to rise
- It doubles again to 1,036 deaths per 100,000 people
- Again, ASCVD is number one
- And when you go out past 85…
- ASCVD holds onto its number one spot
- And cancer takes the number three spot
- It tends to fall (now 12%), although it’s absolute numbers go up to 1,649 deaths per 100,000
- So here, neurodegenerative disease tends to come up and take that place of cancer.
Why go through all of those stats?
- Well, the point to make here is there’s really no decade of life in which cancer is not at least top three causes of death
- And by extension, anybody listening to this is probably thinking of cancer
- It would be almost impossible to listen to this and not know someone who has either battled cancer or who has outright died of cancer
Why cancer screening and early detection is such an important part of the strategy to survive a cancer diagnosis [11:00]
Let’s take a step back and compare cancer to ASCVD
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.



