In this special episode of The Drive, Peter provides a comprehensive overview of the various endocrine systems: the thyroid system, the adrenal system, and the sex hormone system (for both men and women). He walks through the basic biology and the feedback cycles that regulate the production of these hormones and discusses the various options for the treatment of hormone deficiencies. In addition, Peter delves into hormone replacement therapy (HRT), providing nuanced insights into its appropriate usage and the clinical approach he adopts when working with patients.
Peter supplements these explanations with whiteboard illustrations. For a more complete understanding, we highly recommend watching these videos over just listening. The videos can be found on our YouTube channel or on the show notes page.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER

We discuss:
- The thyroid system [2:15];
- The adrenal system [15:45];
- The female sex hormone system [27:00];
- The male sex hormone system [40:00]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
View the clips from each section:
The thyroid system:

The adrenal system:
The female sex hormone stystem:

The male sex hormone system:

Show notes preview below:
The thyroid system [2:15]
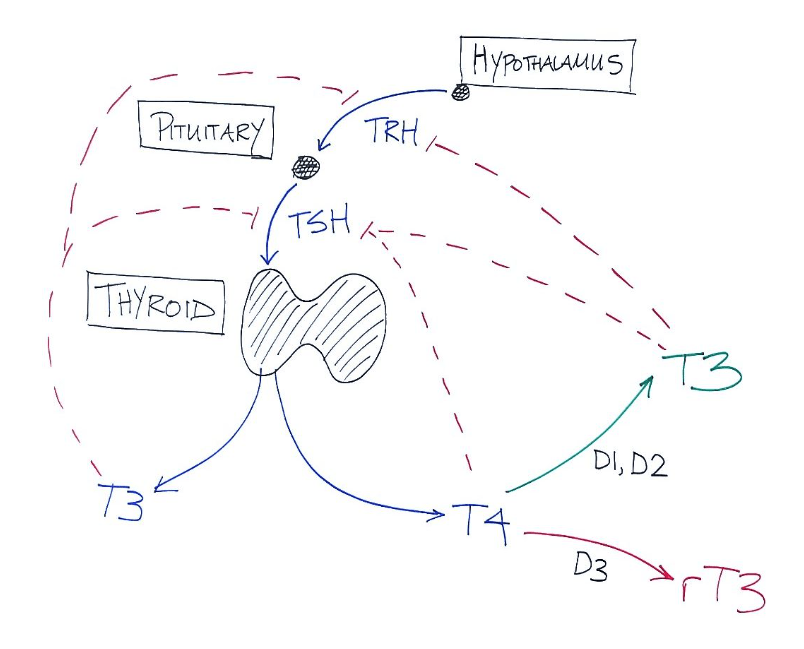
Figure 1. Hormones that stimulate the thyroid, hormones produced by the thyroid and their inhibitory effects.
- The thyroid gland sits in front of your larynx
- You can actually feel it
- It’s shaped like a shield
- The thyroid is regulated directly via a hormone called TSH
- TSH is produced by the anterior portion of the pituitary gland
- TSH tells the thyroid gland to make T4 and T3
- The pituitary gland is regulated upstream by the hypothalamus, which stimulates it via a hormone called TRH (we’ll come back to this)
- The thyroid gland makes mostly T4 and a little bit of T3
- The numbers 3 and 4 refer to the number of iodines in the molecule
- T4 has 4 iodines
- T3 has 3 iodines
- The difference has to do with their biologic activity
All of the thyroid-promoting functions are controlled by the active version, which is T3
- T3 keeps you warm, aids in metabolism, controls things like the brittleness of your nails, your hair, bowel function, all sorts of things
- T4 is the inactive version of the hormone
Most of what comes out of the thyroid is T4, inactive
- It’s not entirely clear what the ratio is between these, but it’s directionally about 4:1 or 5:1 [T4:T3]
- Peter imagines that virtually everything the thyroid is producing is T4
T4 needs to be converted into an active hormone in the body, and that’s where the enzymes called deiodinases come in
- Deiodinases remove one of the iodines from T4 to create T3 (T3 is the active hormone)
- The story gets a little bit more complicated because there are different types of deiodinases, but the three most relevant are D1, D2, and D3
- D1 and D2 are quite similar in that they both convert T4 into T3; what’s different is where they do it
- D1 is extracellular, it’s on the cell membrane facing outward
- D2 is on the membrane of the endoplasmic reticulum and it’s facing internal to the cytosol
- Put that aside for a moment and just keep in mind that D1 and D2 both convert T4 into the active hormone T3, and T3 is the one that has all of the positive effects of thyroid hormone
- D3 is different in that D3 takes T4 and makes something called reverse T3
- Reverse T3 is very similar to T3 except for a very important difference, which is it doesn’t activate the receptor that T3 activates
- It occupies the receptor without activating it
- In effect, you can think of reverse T3 as anti-T3; it basically blocks the effects of T3
- It sounds like a very bad idea to have reverse T3 floating around, and unfortunately in the modern world it often is
- Reverse T3 usually is a sign of inflammation, illness or things of that nature
- The reason it probably exists is to cope with shortage of nutrients
- When nutrients are scarce, when you need to slow down metabolism, one of the first things that the body does is it increases the production of reverse T3 to block the effects of T3
One of the things Peter used to notice when fasting
- When fasting for a week at a time, he would check his blood pre and post
- He was surprised at how much his thyroid function deteriorated during that period of time
- How much much his free T3 and reverse T3 changed
- The ratio of free T3: reverse T3 might go from 0.25 (normal) to 0.05 or less in a 5-7 day fast
- About half of that was due to the reduction in T3, and the majority was due to the increase in reverse T3
The body is going to regulate these three enzymes in response to various physiologic circumstances, and that’s effectively at the cellular level how the body is controlling thyroid function
Evaluating thyroid function
- This creates a bit of a problem when you want to evaluate a patient for their thyroid status because the traditional way to think about a patient’s thyroid status is just to look at their TSH
- On the surface this makes sense because if everything is working perfectly, the TSH should give you the answer
- If the TSH is very high, there must not be much T3 around because it would be inhibiting TSH [refer to figure above]
- If TSH is very, very low, you would be getting a lot of inhibition from these things [on the figure above], and you would be in a hyperthyroid state
- But the reality of it is you can sometimes have a normal TSH and still have the symptoms of hypothyroidism
- For example, you have very high amounts of reverse T3 and very low amounts of T3, in other words, if your T4 is being preferentially shunted into reverse T3 instead of T3, you might feel like you have the symptoms of hypothyroidism
- You could be cold, your metabolism might be slow, you’d have difficulty sleeping
- If it were really extreme, your nails might even get brittle, you’d be constipated
- These sorts of unfortunately nonspecific symptoms which make it difficult to make such a diagnosis at times
- For example, you have very high amounts of reverse T3 and very low amounts of T3, in other words, if your T4 is being preferentially shunted into reverse T3 instead of T3, you might feel like you have the symptoms of hypothyroidism
Where does this matter when it comes to how we treat hypothyroidism?
To be clear, hypothyroidism is far more common than hyperthyroidism
- Peter is not going to talk about hyperthyroidism, he’s going to talk about hypo
- The standard treatment for hypothyroidism is to give T4
- We give a synthetic version of this hormone, the inactive thyroid hormone, and we do that with the knowledge that most patients will convert that T4 into T3 (via D1 and D2)
- The T3 will go on to have all the biologic effects, and it will also suppress TRH and TSH, and the body will come back into line
- For example, if a patient shows up and they have the classic symptoms of hypothyroidism and their TSH is elevated (for example, at 6-7), you might give them 75 mg of T4
- And you might expect to come back and see that TSH at 2-3 and them feeling better
- Many times it works out that way, but unfortunately it doesn’t always work out that way
- Sometimes you give a patient T4 and they start to feel worse, and sometimes their TSH actually improves
- And the reason it improves is T4 does have some inhibition of TSH (not as much as T3, but some)
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.



