Jeremy Loenneke has a Ph.D. in exercise physiology, a Master’s in nutrition and exercise, and is currently the director of the Kevser Ermin Applied Physiology Laboratory at the University of Mississippi, where he focuses his research on skeletal muscle adaptations to exercise in combination with blood flow restriction (BFR). In this episode, Jeremy explains the science of BFR and the mechanisms by which BFR training can produce hypertrophy using low loads. Here, he reviews anatomy and terminology of muscle structure and discusses the evidence that increasing muscular strength may not be dependent on increasing muscle size. Additionally, Jeremy goes into depth on how one might take advantage of BFR training, including practical applications for athletes and average people, as well as the situations for which BFR training would be most advantageous.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Jeremy’s interest in exercise and weightlifting and his scientific training [3:30];
- The microstructure and physiology of muscle [8:00];
- Definitions of fast-twitch and slow-twitch muscle fibers [12:45];
- Comparison of strength vs. hypertrophy [21:30];
- Blood flow restriction training and the origins of the Kaatsu system [28:30];
- The details and metrics related to exercise under blood flow restriction [44:45];
- Considerations when training with blood flow restriction: loading, pace, rest, and risks [53:00];
- Blood flow restriction studies and the relationship between muscle size and muscle strength [1:04:15];
- Evidence that increasing muscular strength is not dependent on increasing the size of the muscle [1:16:30];
- Practical applications of blood flow restriction training for athletes and average people [1:27:30];
- Situations in which blood flow restriction training is most advantageous [1:35:30];
- The mechanisms by which blood flow restriction training can produce so much hypertrophy at such low loads [1:39:45];
- Applications of “passive” blood flow restriction training [1:47:15];
- What experiments would Jeremy do if he had unlimited resources? [1:51:45];
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Pre-show notes
- Jeremy is the Director of an applied physiology laboratory and his research focuses on skeletal muscle adaptations to exercise in combination with blood flow restriction
- Peter first tried blood flow restriction a little over 10 years ago, in a swimming pool
- Blood flow restriction is a general term that applies to occluding some portion of the arterial inflow to a muscle
- Under these conditions, it becomes harder for the muscle to contract
- This allows an individual to exercise with a lower weight than they would normally use
- The most common term associated with this from a brand perspective is Kaatsu, which is Japanese for training with a restriction
- Peter remarks that one of the most interesting things that comes out of this discussion, “is that blood flow restriction offers a very cool way to study the relationship between muscle size and muscle strength”
- This episode will explain the physiology of the sarcomere, the microanatomy of muscle fibers, the difference between type two and type one fibers
- It will explain what an actin filament is and what a myosin filament is
Jeremy’s interest in exercise and weightlifting and his scientific training [3:30]
Jeremy’s interest in exercise
-
- He was into wrestling from age 5 through high school
- He didn’t lift weights then or do any conditioning, but his coaches continually told him to get in the gym to get stronger
- He started listening toward the end of high school
- One of his friends was into bodybuilding and powerlifting; Jeremy started training with him
- It helped a little with wrestling
- He began reading muscle magazines and focused on exercise science early on in undergrad
- He wanted to know how to make a muscle bigger, how to make it stronger
Jeremy’s scientific training
- At first he wanted to work with athletes, but upon trying it, he didn’t like it and turned to research
- He had a mindset that everybody was going to train and train hard and he found a mismatch between his expectations the athletes he worked with
- He landed at the University of Illinois and that’s where he met Lane and a couple of other people
- That’s where he really came came across blood flow restriction and focus his time on this; this was around 2007-2008
- He got into human research
- He did his PhD at the University of Oklahoma
- His dissertation focused on different methods of applying blood flow restriction?
- He evaluated the acute response of different exercise loads of 20%, 30%, under different pressures
- His dissertation focused on different methods of applying blood flow restriction?
- He took a job at Ole Miss, The University of Mississippi
The microstructure and physiology of muscle [8:00]
The anatomy of a muscle
- Muscles are made of tubular fibers called myofibrils, shown in the figure below
- The smallest unit is a sarcomere
- This is the repeating unit between 2 Z-lines (aka Z discs)
- Myofibrils are composed of repeating units of sarcomeres
- Sarcomeres are made up of alternating thin and thick filaments
- The thin filaments are made of actin, shown in green below
- The thick filaments are made of myosin, shown in purple below
- Actin and myosin are both proteins
- Exercise results in the production of more actin and myosin
- Muscle will get bigger when more actin and myosin is made than is broken down
- Actin and myosin interact to cause muscle contraction; this happens during exercise
- Contraction results in signaling for muscle adaptation
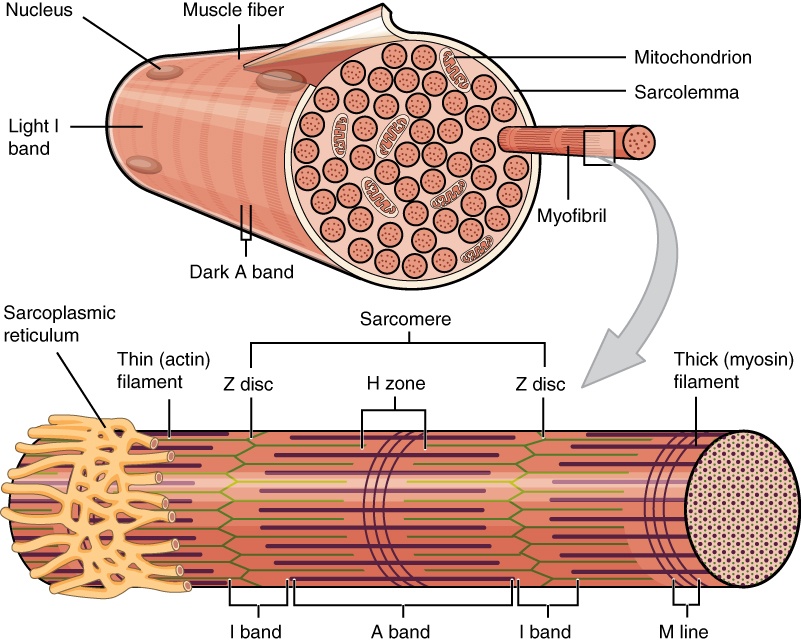
Figure 1. Anatomy of a skeletal muscle fiber. Image credit: OpenStax Anatomy and Physiology.
*Here’s a review of muscle anatomy: Skeletal Muscle Structure | GreatPacificMedia (October 4, 2009) (youtube.com) | [8:00]
There are 2 broad types of muscle, endurance based and force based
- Muscle fibers fall into 1 of 3 categories
- Type I: slow twitch speed, small force, highest resistance to fatigue
- Also called SO for slow oxidative fibers
- They generate energy by oxidative phosphorylation using mitochondria to perform aerobic respiration
- Used for endurance exercise
- Type IIA: fast twitch speed, medium force, some resistance to fatigue but less than type I
- Also called FOG for fast oxidative/glycolytic; or or FO fast oxidative
- They generate energy using aerobic respiration but may switch to anaerobic respiration (which produces lactate)
- Type IIX: fast twitch speed largest twitch force, low resistance to fatigue (fatigue easily)
- Also called FG for fast glycolytic
- They generate energy using anaerobic respiration
- Used for high resistance exercise such a lifting heavy weights
- In reality, muscle exists on a continuum between high endurance and high force capabilities
- Exercise can shift muscle to a different type
- Generally, exercise shifts the overall muscle fiber to become slower, more oxidative, and more efficient
- The sarcomere is composed of fibers bordered by Z-lines, labeled as a Z disc in the previous figure
What happens during muscle contraction
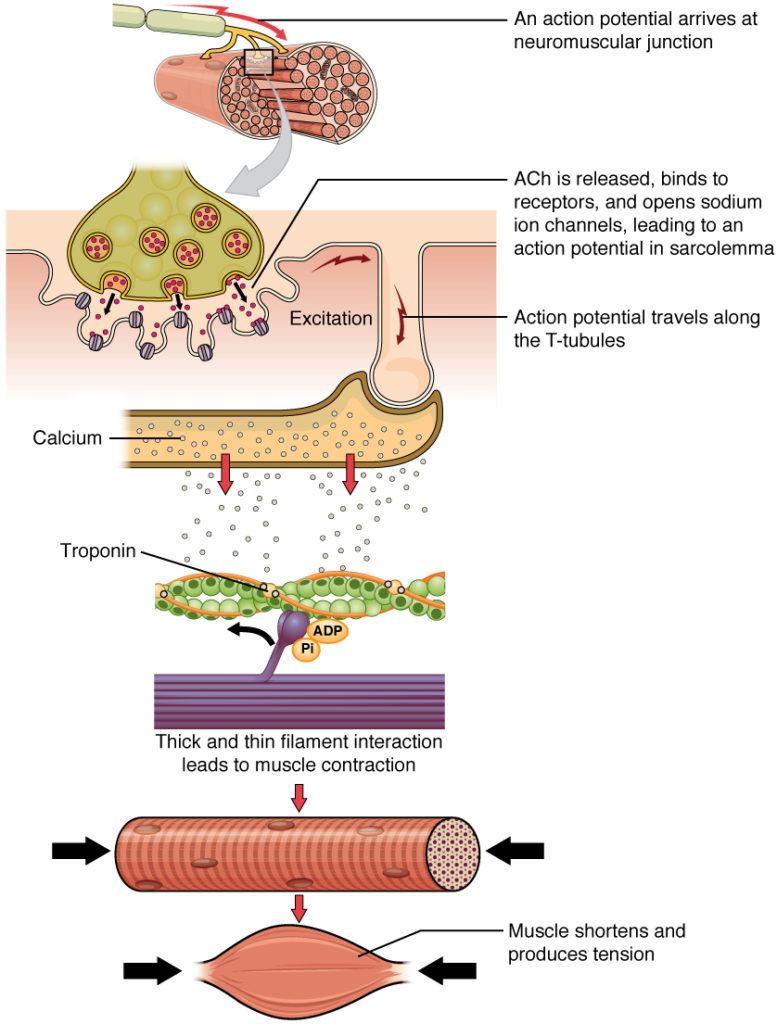
Figure 2. Signaling by a nerve initiates muscle contraction. Image Credit: OpenStax Anatomy and Physiology
- When one decides to exercise, a signal goes from the nerve to the muscle; see the previous figure
- There is a release of calcium
- This calcium will expose binding sites
- During muscle contraction, filaments slide past each other; shown in the next figure
- Myosin (in purple) interacts with actin (in green) to cause this movement
- Myosin has 2 heads; it will bind both actin and ATP
- ATP is required to break the bond between myosin and actin
- ATP is hydrolyzed to recock the myosin head then reattach to actin; this requires more calcium
- As long as calcium is president, or as long as signals for movement are being sent, the actin and myosin in sarcomeres will keep interacting producing muscle contraction
- The actin and myosin don’t all interact at the same time; they each interact at different times to produce fluid motion
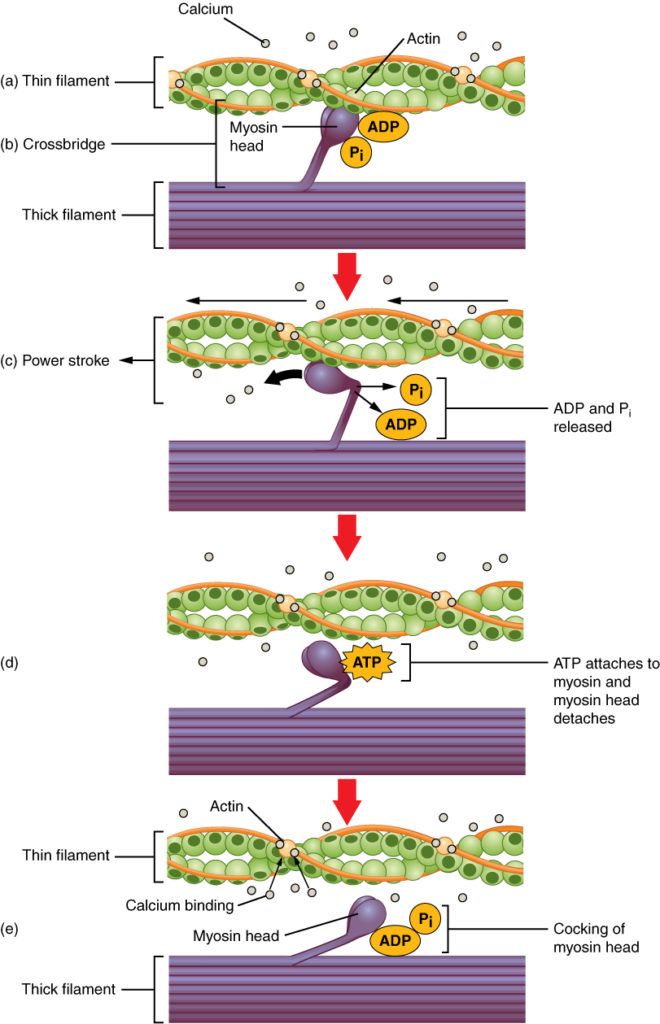
Figure 3. Sliding filament model of muscle contraction. Image credit: OpenStax Anatomy and Physiology
- Peter notes that ATP is required to release the actin-myosin complex, and this explains rigor mortis
- A dead person cannot make ATP; they don’t have the ability to release the actin myosin filaments
- This is why a body gets stiff
- A dead person cannot make ATP; they don’t have the ability to release the actin myosin filaments
- There is a continuum of muscle fibers; the terms fast twitch and slow twitch are used
- The faster twitch muscle has a higher contractile force, but it fatigues quickly
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Jeremy Loenneke, Ph.D.
Dr. Jeremy Loenneke graduated with a PhD in Exercise Physiology from the University of Oklahoma under the mentorship of Dr. Michael Bemben. Dr. Loenneke had previously earned a Master’s degree in Nutrition and Exercise Science from Southeast Missouri State University under the mentorship of Dr. Joe Pujol. As an Associate Professor of Exercise Science at the University of Mississippi, his research focuses on skeletal muscle adaptations to exercise in combination with blood flow restriction. His recent work has answered several important methodological and safety questions with respect to applying blood flow restriction. Dr. Loenneke is the director of the Kevser Ermin Applied Physiology Laboratory. He is a Fellow of the American College of Sports Medicine and a member of the American Physiological Society. He also serves as a peer reviewer for several journals including Sports Medicine, AGE, Medicine and Science in Sports and Exercise, and the Journal of Applied Physiology. [The University of Mississippi faculty profile and department of Health, Exercise Science, and Recreation Management]



