Kari Nadeau is a physician scientist with expertise in treating food allergies. In this episode, Kari first explains the fascinating workings of the immune system, exploring how it adeptly defends against bacteria and viruses but how the same system can lead to food allergies. She proceeds to explore the complexities of food allergies, detailing their typical developmental patterns, underscoring the significance of preventative approaches like early exposure, and highlighting the potentially life-threatening nature of severe food allergies. Kari illuminates the latest advancements in immunotherapies that not only mitigate allergy severity but also hold the potential to completely cure the patient. Additionally, Kari shares her concerns about the increasing levels of air pollution, elucidating its adverse effects on health while providing valuable suggestions for reducing exposure.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER

We discuss:
- Kari’s motivation to study food allergies [4:00];
- Overview of the immune system and the family of immunoglobulins [9:00];
- How our immune system fights a virus, bacteria, or fungi, and some exceptions to the rule [13:00];
- Why our immune system is generally better at fighting viruses than bacterial infections [18:45];
- Differentiating a food sensitivity from a food allergy, and a discussion about celiac disease [25:30];
- How food allergies develop, why they can be lethal, and factors contributing to the uptrend in food allergies [35:45];
- The role of environmental factors in the onset of food allergies and strategies for prevention [50:15];
- How immunotherapy helps to overcome, and even cure, food allergies [1:04:15];
- Can immunotherapy work for environmental allergens like pollen? [1:24:00];
- Air pollution: impact on health and tips for reducing your risk [1:25:30];
- What happened to Kari’s early patient who died despite using an epinephrine device? [1:37:15];
- Resources for those wanting to learn more or find clinical trials related to food allergies [1:40:45]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Kari’s motivation to study food allergies [4:00]
- It’s been 8 years since Peter and Kari were together in person
- He always appreciated the amount of time she used to make for him when he would wander into her lab at Stanford, just to pick her brain
- He always thought her work was exciting and knows that it ties into so much about what people are interested in around food allergies, even to some extent food sensitivities
- It’s also very interesting to discuss air pollution
- This is probably something that isn’t getting enough attention with respect to health
- Peter feels woefully deficient in his understanding though he tries to pay attention to his PM2.5 but he’s not sure what to do with that information sometimes
- Kari has now left Stanford and is at Harvard
What Kari’s Ph.D. dissertation focused on
- She was really excited to do her Ph.D. in biochemistry
- She learned a lot about toxicology and biochemistry
- She did her Ph.D. in parasitology working on an enzyme in a parasite called the trypanosome, which causes African sleeping sickness and another disease called Chagas disease
“I loved my work there because we were able to go to the very minute levels of understanding of a chemical entity to be able to create a drug to target that entity to help people with that disease.”‒ Kari Nadeau
- She did her Ph.D. at Harvard under Chris Walsh; it was a great Ph.D., she loved it
- Then she did other work in immunology and animal models
- She is also a pediatrician by training
What led you to study the field of food allergies?
- She did her M.D. training at Harvard and then trained in pediatrics at Children’s Boston as well as Stanford
- With that, she had the opportunity to become a fellow in a feel that she loved: allergy, asthma, and immunology
- She had done a lot of immunology work when she did her Ph.D. in parasites because parasites are killed by immune cells
- Especially this little molecule called IgE: it tends to kill parasites but it’s not so great for allergies
- This yin and yang of this molecule [IgE] in biology as an immunologist was really interesting
- Fast-forward, she was a fellow on the wards about to see a patient that she was being asked to consult on for a milk allergy
- He was in the ICU after having drunk a glass of milk and having a bad reaction
- By the time she arrived, he had died, and his parents were being asked to give consent for him to be a liver donor
- She took care of the person that received the liver who also had a milk allergy
- That gave her pause and really initiated her efforts in food allergy to understand the role of IgE (the role of the immune system) and how food allergies get started in the first place
Kari wanted to know: “How in the world did a child with food allergy who died then give his same food allergy to the recipient of his liver?”
- All of these things started to catalyze her curiosity, and she felt very blessed and lucky at the time to be able to be in a lab
- She feels that we’re obligated to be able to use that training to best help mankind and to best help those questions that parents ask us
- At the bedside of this particular young child that died, unfortunately due to a milk allergy, she’ll never forget his father trembling, asking why the EpiPen didn’t work?
- “What can we do to help children in the future never have to die again?”
- Kari promised that father that she would do the absolute best to prevent further deaths in children and adults with food allergy as well as help really make sure that we educate about the use of injectable epinephrine devices and how to best use them to prevent deaths to food allergy
- That’s her why, and ever since then she’s always wanted to really help out in this field
Overview of the immune system and the family of immunoglobulins [9:00]
You mentioned one of the immunoglobulins (IgE), talk about the family of immunoglobulins: what are they there for? How do we acquire them? How do they normally function?
- We have certain proteins in our blood that help protect us and that’s what they’re meant to do and that’s great
- And they exist in different concentrations
- Just like in a milkshake, you have different proteins that exist in different concentrations and they’re all there for nourishment purposes, sometimes for taste too
- The proteins in our blood that constitute immunoglobulins are really helpful
- For example, we learned a lot about how important immunoglobulins were to protect against COVID
- Everyone wanted to know their “titers” and what that means is immunoglobulin
- For example, we learned a lot about how important immunoglobulins were to protect against COVID
- IgG is the main class of immunoglobulin, and those are very protective
- They are proteins found in high amounts in our plasma
- [the figure below summarizes the different classes of immunoglobulins, aka antibodies]
- The minute someone is under a drug like a steroid (or other drugs that affect your immune system), the amount of immunoglobulin in the blood decreases
- It’s important to have good concentrations (not too high), and immunoglobulins in general help protect us against infections and they also help protect us against allergies
- There’s another complimentary suite of immunoglobulins that don’t just stay in our blood, they get into our organs
- Because you want to protect all of the surfaces around your organs (in addition to your blood)
- For example IgA class (we call that the secretory class)
- That’s helpful in our saliva, in our gut
- In women who are pregnant, they secrete it after pregnancy in their breast milk
- When people are missing IgA, they have allergies
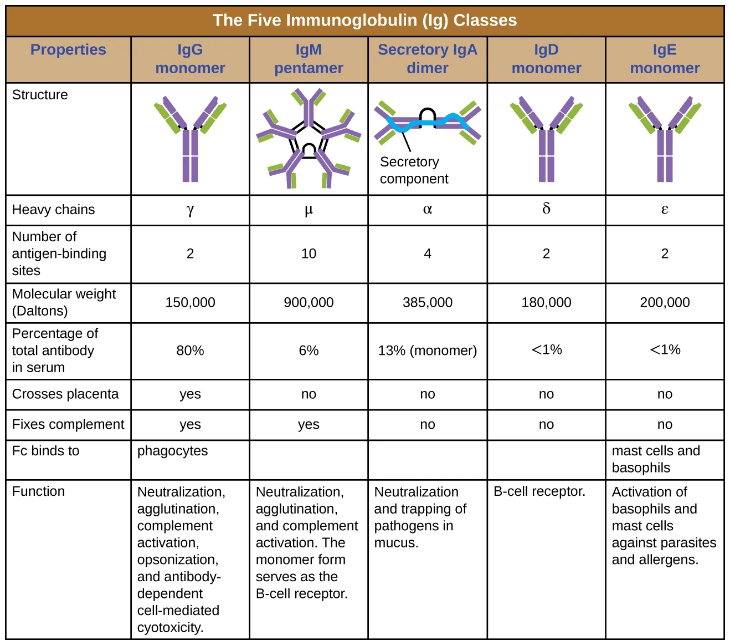
Figure 1. Classes of immunoglobulins (aka antibodies). Image credit: OpenStax Microbiology
- The other immunoglobulin class that Kari will talk about is IgM (the “Marines” of the immunoglobulins)
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Kari Nadeau, M.D., Ph.D.
Kari Nadeau earned her B.S. in Biology from Haverford College and her M.D./Ph.D. from Harvard Medical School. She completed a pediatric internship and residency at Boston Children’s Hospital and a residency and fellowship in allergy, asthma, and immunology at Stanford-UCSF. After this, she joined the faculty at Stanford Medical School. Currently, Dr. Nadeau is the Chair of the Department of Environmental Health at Harvard School of Public Health and John Rock Professor of Climate and Population Studies. She practices Allergy, Asthma, Immunology in children and adults.
For more than 30 years, Dr. Nadeau has devoted herself to understanding how environmental and genetic factors affect the risk of developing allergies and asthma, especially wildfire-induced air pollution. She has published over 400+ papers, many in the field of climate change and health. Her laboratory has been studying air pollution and wildfire effects on children and adults, including wildland firefighters. She oversees a team working on air pollution and wildfire research along with a multidisciplinary group of community leaders, firefighters, engineers, scientists, lawyers, and policy makers. Dr. Nadeau was appointed as a member of the U.S. Federal Wildfire Commission in 2022. She is also a member of the National Academy of Medicine and the U.S. EPA Children’s Health Protection Committee.
Dr. Nadeau co-founded Before Brands, IgGenix, alladapt immunotherapeutics, and COUR Pharmaceuticals. At Stanford, she started the Sustainability Health Seed Grant initiative as well as the Climate Change and Health Equity Task Force and Fellowship program. [Harvard]



