Steven Dell is an ophthalmologist, current Medical Director of Dell Laser Consultants, and a leader in refractive eye surgery with over 20 patents to his name. In this episode, Steven explains the anatomy and functional mechanics of the eye and how they relate to common variations in vision. He discusses changes in vision that occur with aging, the fundamentals of different types of vision loss, and provides an in-depth look into the various treatments and procedures available for corrective eye surgery. Additionally, Steven explains how one might protect the eyes and prevent vision loss—a topic particularly important for children in light of the epidemic of myopia.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Why Steven chose ophthalmology, and the crossovers to other medical disciplines [3:45];
- Anatomy of the eye, common types of vision loss, and age-related vision changes [14:15];
- Eye drops that can potentially improve vision [27:30];
- The explanation for different eye colors [33:15];
- Physiology of the eye and its connections to the brain [34:45];
- Understanding human vision through an evolutionary lens [41:00];
- Enhancing vision beyond 20/20 [47:00];
- Astigmatism: definition, cause, and high prevalence [51:30];
- Nearsightedness (myopia): causes, epidemic in children, and prevention strategies [54:15];
- Cataracts: impact of aging and how they can be repaired [1:05:00];
- Lens implants that can correct and improve vision [1:19:30];
- Effects of eye trauma [1:26:45];
- Corneal abrasion from ‘dry eye’: causes, treatment, and prevention strategies [1:29:00];
- Sunglasses for eye protection [1:35:00];
- Solutions to correct nearsightedness [1:42:00];
- Laser eye surgery—photorefractive keratectomy (PRK) [1:45:45];
- Laser eye surgery—LASIK [2:02:00];
- Laser eye surgery—small incision lenticule extraction (SMILE) [2:11:45];
- Glaucoma: definition, causes, symptoms, and care [2:13:45];
- Tips for preserving eye health [2:20:00];
- Screen time and eye health [2:24:15];
- Contact lenses: good hygiene and considerations [2:27:45];
- A bonus benefit from repairing cataracts [2:29:00];
- Questions about corrective eye surgery [2:31:30];
- How an eye exam can be a window into metabolic illness [2:33:45]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Why Steven chose ophthalmology, and the crossovers to other medical disciplines [3:45]
- The eye is a topic that everybody has questions on, Peter included
- From medical school, Peter remembers there is an optic nerve, a cranial nerve, and the second cranial nerve (this is the optic nerve)
- He remembers something called fovea, and he knows there’s a blind spot, but he’s forgotten why
- Peter remarks, “It’s safe to say my knowledge of this topic right now is probably at par with everybody’s right?”
- Steven understands, “Well, that’s not rare, frankly, because the eye is so literally compartmentalized. We just don’t interact that much with other specialties, so it’s not rare for people who are in other specialties to be very ignorant of the eyeball, and that’s fine because I think it’ll help us keep the level of discussion at an approachable level for everyone.”
- Peter asks if there has ever been discussion suggesting that ophthalmologists don’t need to do the four-year MD degree
- How much of what was learned in medical school became relevant in residency?
- Steven says there was quite a lot
- There’s nothing specifically magical about the eyeball
- It’s got neurological tissue in the back, actual brain tissue in the back
- It’s got a vascular supply
- There are a lot of crossovers to other medical disciplines
- All of the cellular processes are the same
- He operates adjacent to the eye
- He thinks it’s important for ophthalmologists to have a general sense of medical knowledge, particularly because so many systemic diseases manifest as eye problems
- Now there is a discipline of medical training or of visual training, basically optometry— which deals with the eye, but not all of the surgical stuff
- He works in a collaborative fashion with optometrists
- Those are the folks who are fitting glasses
- They’re screening for eye disease
- They’re handling preoperative and postoperative care in many cases
- They’re treating some diseases that are specific to the eye, such as glaucoma
Ophthalmology training
- Peter asks about ophthalmology residency— does everyone spend time operating?
- Is there a nonsurgical discipline to this?
- Does the training bifurcate?
- Steven explains, “There are nonsurgical ophthalmologists, but I think they all start out as surgeons to become an ophthalmologist. You’re really training to become an eye surgeon.”
- But there are, for example, neuro-ophthalmologists, which are really more neurologists than eye surgeons; they don’t do eye surgery
- There are some ophthalmologists who don’t do eye surgery
- Peter recalls one of his lasting memories from residency was stealing suture from the ophthalmology OR at Hopkins
- As the number of the suture gets larger the suture itself gets smaller
- An O suture is thick, like a piece of rope
- The scale progresses from 1-0, 2-0, 3-0, etc
- By a 4-0 suture, it’s actually quite thin
- Steven replies they use an 11-0 suture
- Cardiac surgery uses a 7-0
- Occasionally there’s some guys that would sew the distal end of a coronary artery with an 8-0 and at that level, it’s already very thin; just the slightest tug too much, and it breaks
- Peter recalls about ophthalmology, “you guys wrote 11-0, and so I used to steal 11-0 constantly every night I was on call and practice suturing with 11-0. The thinking being, if you can tie in 11-0 with your hands and not tear it, that 7-0, which normally is like a piece of hair is going to feel like a piece of rope. I used it to help me develop a good feel for fine suture”
- The tools in ophthalmology are tiny and Steven can remember the operating room where he did his training was near orthopedic surgery
“You hear this Black and Decker stuff going on over there, and our little tiny tools are very, it’s just totally different” – Steven Dell
- Everything he does operationally is under a microscope
- They use a binocular microscope
- So he’s looking through both eyes, and this is either mounted from the ceiling and is controlled by his feet
- The X, Y, and Z, and the zoom focus are controlled by a foot pedal
- And that either comes from the ceiling or it’s on a really large stand
- He’s sitting and looking straight ahead, so the image is here, but he operating down below
- It’s interesting because sometimes his wife will kid him, I’ll come home from a day of surgery exhausted, but she says something like, “well, I don’t really get it. You’re just sitting in a chair, making these little tiny movements, and there’s soft music playing. It all seems very, very sedate.”
- It’s incredibly stressful and exhausting
- Ophthalmologists have a problem where they tend to hyperextend
- They tend to bring their head forward, to come up to the oculars and that creates a whole other set of problems
- There are ergonomic challenges for sure, and he remembers early on in his career, he was coached very carefully on how to sit, how to have his spine arranged
- One doesn’t want to crane their neck forward
- He has to make sure his shoulders are down
- Steven notes, “It’s interesting because when you train surgeons, and you look at them, they’re all raising their shoulders up, and they’re terrified that they’re going to do something wrong. They’re in a very, very compromised and stressful position, and then they tend to lift their hands up.”
- The surgical movements are these little tiny movements, so very small positional changes can have a huge impact on the outcome of the surgery
- Peter understands this problem, he has 2 friends from residency who required multiple neck surgeries
- One of them could no longer operate after his surgery; he trained as a cardiac surgeon and now does cardiac critical care
- It’s still a great career, but after 10 years of training as a cardiac surgeon, to not be able to operate…
- One of them could no longer operate after his surgery; he trained as a cardiac surgeon and now does cardiac critical care
- Peter asks if Steven knew he wanted to do ophthalmology when he began medical school
- No, but he knew he wanted to do something surgical, something with his hands
- He remember a Eureka moment where the first time he looked through a slit lamp (which is basically a microscope to look into the eye) he was hooked
- This was during an ophthalmology rotation in a weeks where they did a little ophthalmology and a little ear, nose, and throat
- It was then that he knew ophthalmology was what he wanted to do
- He had some exposure to ophthalmology prior because the father of one of his friends was an ophthalmologist
- Peter asks if ophthalmologists do a general surgery internship
- Some do; Steven did what is referred to as a transitional residence internship, where one does a little bit of everything: general surgery, internal medicine
- It was very helpful
- The general surgery part was rough, but it was nice to have exposure to a little bit of everything
- It was a 4-year residency, including the internship
- Peter asks what was the “bread and butter”?
- For example, in general surgery in the 1960’s and 1970’s, it would’ve been Billroth procedures and things like that, where the most common thing one was doing was cutting out half of the stomach because of peptic ulcer disease and things like that
- By the time he got to residency, he never did one of those because H2 blockers and PPIs basically eliminated the need to surgically remove part of the stomach for gastric or peptic ulcers
- Peter wants to know, at the time of his training, where did 80% of the volume come from? What type of cases?
- It was cataract surgery and then retinal disease
- It’s still cataracts
- The scourge of essentially diabetes causes these very, very complex retinal problems
Anatomy of the eye, common types of vision loss, and age-related vision changes [14:15]
- When Steven explains the eye to a kid, he compared it to a camera with film in the back; that’s the retina
- Then the kid looks at his parents and asks, “What’s a camera? Film, what’s that?”
- The eye is built like a camera where in the very front is the cornea
- The cornea is the covering on the front of a watch; that’s the thing that a contact lens would sit on
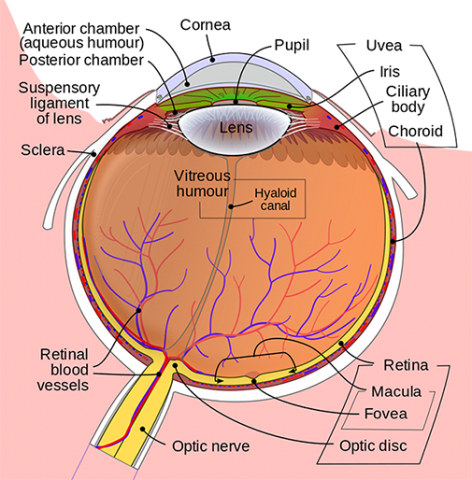
Figure 1. Anatomy of the eye. Image credit: Kellogg Eye Center
- The next thing is the pupil, which is the hole in the iris
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Steven Dell, M.D.
Steven Dell is a board certified ophthalmologist in Austin and the Medical Director of Dell Laser Consultants. He is an internationally recognized leader in refractive eye surgery specializing in: LASIK laser eye surgery, cataract surgery and refractive lens exchange. He is the chief Medical Editor of the medical journal Cataract and Refractive Surgery Today. He is the Chair-emeritus and President-emeritus of The American-European Congress of Ophthalmic Surgery. He is a principal investigator for a variety of FDA clinical trials in the field of eye surgery. He has invented several surgical instruments and devices, and holds over 20 US and international patents in eye surgery including the: Dell Astigmatism Marker™, Dell Fixation Ring™, Dell PlumeSafe Ophthalmic Evacuation System™, and Dell PlumeSafe Handpiece™. He is also the author of numerous textbook chapters and peer-reviewed journal articles. [Dell Laser Consultants]



