Stuart McGill is a distinguished professor emeritus at the University of Waterloo and the chief scientific officer at Backfitpro where he specializes in evaluating complex cases of lower back pain from across the globe. In this episode, Stuart engages in a deep exploration of lower back pain, starting with the anatomy of the lower back, the workings of the spine, the pathophysiology of back pain, and areas of vulnerability. He challenges the concept of nonspecific back pain, emphasizing the importance of finding a causal relationship between injury and pain. Stuart highlights compelling case studies of the successful treatment of complex cases of lower back pain, reinforcing his conviction that nobody needs to suffer endlessly. He also covers the importance of strength and stability, shares his favorite exercises to prescribe to patients, and provides invaluable advice for maintaining a healthy spine.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Peter’s experience with debilitating back pain [3:30];
- Anatomy of the back: spine, discs, facet joints, and common pain points [14:45];
- Lower back injuries and pain: acute vs. chronic, impact of disc damage, microfractures, and more [24:45];
- Why the majority of back injuries happen around the L4, L5, and S1 joints [31:00];
- How the spine responds to forces like bending and loading, and how it adapts do different athletic activities [36:15];
- The pathology of bulging discs [43:15];
- The pathophysiology of Peter’s back pain, injuries from excessive loading, immune response to back injuries, muscle relaxers, and more [46:00];
- The three most important exercises Stuart prescribes, how he assesses patients, and the importance of tailored exercises based on individual needs and body types [56:15];
- The significance of strength and stability in preventing injuries and preserving longevity [1:08:15];
- Stuart’s take on squats and deadlifting: potential risks, alternatives, and importance of correct movement patterns [1:19:30];
- Helping patients with psychological trauma from lower back pain by empowering them with the understanding of the mechanical aspects of their pain [1:30:00];
- Empowering patients through education and understanding of their pain through Stuart’s clinic and work through BackFitPro [1:39:00];
- When surgical interventions may be appropriate, and “virtual surgery” as an alternative [1:46:45];
- Weakness, nerve pain, and stenosis: treatments, surgical considerations, and more [1:55:30];
- Tarlov cysts: treatment and surgical considerations [2:00:15];
- The evolution of patient assessments and the limitations of MRI [2:02:15];
- Pain relief related to stiffness and muscle bulk through training [2:07:00];
- Advice for the young person on how to keep a healthy spine [2:14:15];
- Resources for individuals dealing with lower back pain [2:25:30]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Peter’s experience with debilitating back pain [3:30]
Stuart read Peter’s book [Outlive] and changed his behavior
- A few years ago, Stuart’s family doctor (who is one of his former students) did his blood work, and found he was just on the edge of needing Crestor or Lipitor
- His physician suggested, “Let’s run the experiment,”
- Stuart loves to work hard physically and finish it off with a beer, which 6 days out of 7, he’s denying himself of that
- Long story short, the experiment paid off, and he’s sleeping a little better and is a little more mentally sharp
- Peter thinks maybe he doesn’t have to be quite as restrictive
- He doesn’t necessarily believe in denying all the pleasures of life
Why the topic of biomechanics for a healthy back is of great interest to Peter
- The very abridged version of the story is Peter grew up doing all sorts of really aggressive things and really took to powerlifting when he was about 14
- He found himself reasonably strong for a little scrawny kid
- Between about the ages of 14-19, he really pushed
- He couldn’t bench press to save his life, but seemed pretty strong in a squat and deadlift
- He ignored any claims his parents made that maybe he was doing a little too much
- Truthfully, Peter had no formal instruction
- He was just watching the other grown men in the gym who were insanely powerful and trying to replicate what they were doing
- Peter had no sense of what he was doing
- Fast-forward to age 21, and he’s rowing crew, and for the first time in his life he experienced lower back pain
- This really rocked his world, because he always thought that people who got lower back pain were people who did nothing
- He never thought that someone who was as active as he was could get it
- For about 2 weeks, the back pain completely disabled him
- He could barely get around
- As a college student, he didn’t really have any resources and didn’t know what to do
- This was in the summer, so he didn’t have classes, but he had to stop rowing
- Otherwise he was able to work
- The back pain went away and he thought everything was fine
- He never thought about it again until the summer 3 years later, when he was 24 years old
- He was in San Diego riding his bike up the steepest hill, a patch of mountain called Mount Soledad
- There’s a section of this thing where you make a sharp right turn, and at that moment it’s about a 25 degree pitch
- Peter experienced this very sudden pain in his lower back and like a typical idiot, just kept on pushing and climbing to the top and finished the ride
- But then went on to experience the exact same thing: for two weeks he was debilitated and couldn’t do a thing other than lay around and walk, but then it got better and he just forgot all about it
- Fast-forward to the big one
- This occurred in Peter’s 3rd year of medical school
- He’s now 27 years old, and the remarkable consistency of this is not lost on him
- It is every 3 years by the summer, the summer of ‘94, ‘97 and 2000
- He’s riding his bike from class to the gym, he gets to the gym, hops off his bike to lock it up, and all of a sudden he feels that same familiar, horrible pain in his back
- But this time it’s a little worse than the previous 2 bouts
- It was so bad that he did something he’d never done before: he decided not to go into the gym
- He just slowly got back on the bike and limped his way back to his apartment and wasn’t able to do anything other than just lay in bed
- It was so bad that he did something he’d never done before: he decided not to go into the gym
- He assumed he’d be fine the next morning and he woke up the next morning and actually couldn’t get out of bed
- Luckily, Peter and his roommate each had separate phone lines, so Peter was able to call him from his room
- So began a really painful journey over the next couple of weeks where the only place he could find relief was bent at 90-degrees forward, where he would basically stand and bend over the nurses station
- By this point, he was doing clinical rotations and as every good, gunning medical student knows, there was no way he was going to miss a day
- He would drag himself to the hospital each day and somehow manage to get through
- The nurses and residents took pity on him, and they were injecting him full of Toradol
- This went on for a month
- It got so bad that eventually the pain progressed from just being debilitating in his lower back to a nerve pain that felt like his foot was being skinned
- It was interesting in that the pain in his lower back started to subside as it was replaced by the feeling of his left foot being skinned from the bottom
- This story gets worse and worse before getting better, but needless to say, Peter has a graduate degree in back pain
- There is a happy ending to this story, which is after this bout (which took a year to resolve), he made it a mission to figure out what was going on
- Fortunately, any time he’s had back pain since then, it has been a very, very short-lived experience
Peter plants one last seed that we can come back to before we jump into this
- If a reasonable person were to look at an MRI of Peter’s spine today at age 50, you would say, “How does he walk? This person must be in so much pain he doesn’t know his name.”
- But for the most part, Peter is not in pain at all
- Occasionally, he gets a little tight in his lower back, but he doesn’t have radicular pain
- He’s not limited in anything he does
This suggests that the correlation between the image of his back on an MRI and his symptoms is pretty light
- Peter adds, “The fact that you’re smiling so much as I tell you this story tells me not that you’re taking pleasure in my pain, but rather the familiarity of my story.”
- Exactly, Stuart has been doing pattern recognition
There’s only one thing that would account for the repeated acute episodes
- Stuart recognizes that in the interim between each episode, Peter was quite fine
- Then it shifted to a ridiculous pain and now he’s at the stage of life where it’s more an occasional grumpiness when he crosses what we call the “tipping point”
- Stuart asks, “Did the pain go to your foot, Peter?… Big toes or little toes?”
- Yes, it was burning pain that was like the bottom of the foot was being skinned
- There’s one detail Peter should have shared that might explain this: when he finally had surgery, it turned out that he had a free fragment that was about 5 cm long from the L5 S1 disc
- That free fragment had broken off
- Stuart was going to guess this
- He was going to ask which foot
- The 5th route goes to your big toe
- The unbearable pain Peter was having presumably was because that free fragment was parked on the S1 nerve root
- Even though it ended up taking 2 surgeries to get that out, and those surgeries ended up causing more damage that needed more repair (that turned into a journey of 1000 cuts)
- He was on the road to recovery
- The radicular pain seemed to be directly a result of the S1 nerve root
- Stuart is smiling because Peter told him exactly what the pain mechanism was
- He knew it was a disc switch an open fissured disc bulge
- It would be on the side of his foot, right or left
- Stuart asks, “What foot was it?”
- It was the left
Stuart explains, “You had a posterior left-sided, biased open, fissured disc bulge that would open and close as a function of the flexion postures bending down to lock your bicycle.”
- Before we get into the mechanisms, let’s walk through the anatomy of the back
Anatomy of the back: spine, discs, facet joints, and common pain points [14:45]
- Peter remarks, “You could almost argue it’s a miracle we don’t get more injured even though the frequency with which we do is intense.”
- Stuart would almost argue the opposite
- There was a TV show where they asked various experts around the world, “If you got to re-engineer your particular area… How would you re-engineer it and make it better?”
- Stuart was the spine guy, and they had a cardiac person, an endocrine person
- Every expert said they couldn’t, it was perfect
- Every system in your body comes with a trade-off, and there are rules that manage that trade-off
The spine
- This spine is a series of vertebrae forming a flexible rod
- This allows us to dance and move and procreate, tie our shoes, and do all of these wonderful things
- But at some point now, say are picking your child out of the crib, you reach across the crib, gather your child, pull them in
- If you had a flexible rod (consider a series of stacked oranges) it would fall apart
- You need a flexible rod that you can then stiffen to bear load
- You cannot push rope, but you can push stone, or in this case an I-beam to bear load
All of these things [a flexible rod that can stiffen to bear load] are necessary to have a functional spine
The structure of the discs [intervertebral discs]
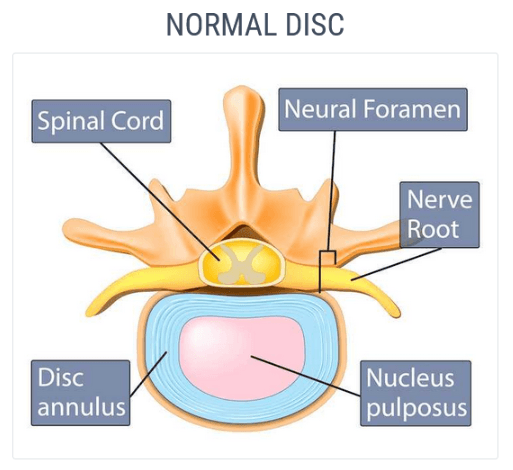
Figure 1. Anatomy of a normal intervertebral disc. Image credit: Miami Neuroscience Center
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.
Stuart McGill, Ph.D.
Stuart McGill earned a Bachelor of Physical Education from the University of Toronto. He earned a Masters in Science at the University of Ottawa to earn a Masters in Science, then a Ph.D. at the University of Waterloo. Dr. McGill stayed at the University of Waterloo as a professor of Kinesiology and Health Sciences for 32 years. He is now a distinguished professor emeritus.
His laboratory and experimental research clinic investigated issues related to the causal mechanisms of back pain, how to rehabilitate back-pained people and enhance injury resilience and performance. During his academic career he authored over 240 peer-reviewed scientific journal papers, received many international awards, and mentored over 40 graduate students.
His work continues at Backfitpro Inc. where he is the chief scientific officer. He sees elite athletes and people with difficult back cases. He has also authored several books on the mechanics of pain, fitness, and performance as it pertains to the back including: Ultimate Back Fitness and Performance, Low Back Disorders, Back Mechanic, and Gift of Injury. [backfitpro.com]



