Ted Schaeffer is an internationally recognized urologist who specializes in prostate cancer. In this episode, Ted delves deep into the realm of prostate health, starting with strategies for vigilance and effective management of the issues that can arise with aging, including urinary symptoms, prostatitis, pelvic pain, and prostate inflammation. Ted sheds light on the popular drug finasteride, renowned for its dual purpose in prostate shrinkage and hair loss prevention, as well as the contentious topic of post-finasteride syndrome. Ted then shifts to the topic of cancer, explaining how androgens, genetics, and non-genetic factors contribute to the pathogenesis of prostate cancer. He provides valuable insights into cancer screening, examining blood-based screening tools like PSA and the use of MRI in facilitating biopsies and their interpretation. Finally, he explores the various treatment options for prostate cancer, including surgical interventions, androgen deprivation therapy, and more.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Changes to the prostate with age and problems that can develop [3:45];
- Behavioral modifications to help manage nocturnal urinary frequency and other lower urinary tract symptoms [8:30];
- Pharmacologic tools for treating nocturnal urinary frequency and lower urinary tract symptoms [16:30];
- Surgical tools for treating symptoms of the lower urinary tract [26:15];
- HoLEP surgery for reducing prostate size [32:30];
- Prostate size: correlation with cancer, and considerations for small prostates with persistent symptoms [40:30];
- Prostatitis due to infection: symptoms, pathogenesis, and treatment [46:45];
- Prostatitis caused by other factors besides infection [58:45];
- How to minimize risk of urosepsis in patients with Alzheimer’s disease [1:05:00];
- Prostate cancer: 5-alpha reductase inhibitors, how androgens factor into pathogenesis, and more [1:10:00];
- Post-finasteride syndrome [1:18:15];
- The relationship between testosterone and DHT and the development of prostate cancer over a man’s lifetime [1:26:30];
- How genetic analysis of a tumor can indicate the aggressiveness of cancer [1:35:15];
- Pathogenesis and genetic risk factors of prostate cancer, and the use of PSA to screen for cancer [1:37:45];
- Non-genetic risk factors for prostate cancer [1:45:45];
- Deep dive into PSA as a screening tool: what is PSA, definition of terms, and how to interpret results [1:56:30];
- MRI as a secondary screening tool and the prostate biopsy options [2:13:15];
- Ted’s ongoing randomized trial comparing different methods of prostate biopsy [2:24:00];
- Determining when a biopsy is necessary, interpreting results, explaining Gleason score, and more [2:27:00];
- Implications of a Gleason score of 7 or higher [2:46:45];
- Metastasis of prostate cancer to different body locations, treatment options, staging, and considerations for patients’ quality of life and survival [2:53:30];
- How prostate cancer surgery has improved [3:09:30];
- Questions to ask your neurologist if you are considering prostatectomy for cancer [3:21:45]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Changes to the prostate with age and problems that can develop [3:45]
What the prostate gland is and what it does
- Let’s start at the beginning
- It’s worth assuming that a lot of people didn’t hear the first podcast, and those that did probably don’t remember much
- A lot has changed in four years [since the previous podcast with Ted]
- The prostate is an exocrine gland, and it’s part of the reproductive system
- It sits just below the bladder in men (shown below)
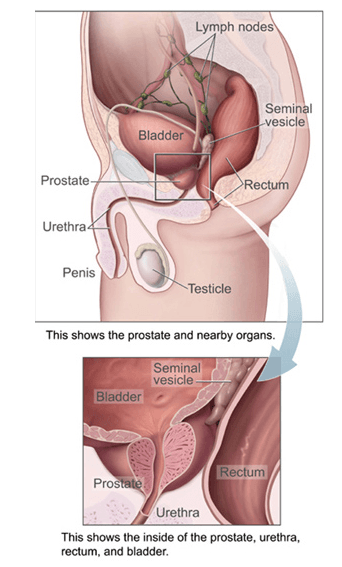
Figure 1. The prostate and nearby organs. Image credit: Wikipedia
- The prostate is a dimorphic organ, it does not exist in women
- It develops in utero in response to fetal androgens
- It produces 50-60% of the components of semen
- It’s used in reproduction in all mammals
When you think about things that start to go wrong in the prostate, most men might think of prostatitis
- Inflammation, infection, benign enlargement that leads to obstruction and the neoplasm
- The prostate is an organ that sits in line with the urinary tract
- The urinary tract in men has a dual purpose
- 1 – It’s used for reproduction
- 2 – It’s used to eliminate all the urine
- Because of that shared functionality, you can develop problems in one or the other of those two disease systems and they result in symptomatic issues
- A lot of problems that men will experience are related to the prostate
- Even at a young age, but particularly as they age
- It’s absolutely true that in younger men you can develop infections in the urinary tract, and they can be problematic and difficult to solve if they involve the prostate
- If you develop an infection (classic bacterial or potentially viral or other kinds of causes) you can get inflammation in the prostate, which can result in long-term pain
- That’s one of the things Ted sees when young men come in with prostatitis
- The prostate evolves and changes as we get older, different issues arise
- They can result and impact your urinary function, because it’s a shared system of elimination of semen and of urine
Prevalence of prostate problems
- As we get older, 50-60% of men at age 50 and older will have issues with lower urinary tract dysfunction, and those almost always directly relate to the prostate in some way or another
- By age 60, it’s 75-80% of men will have lower urinary tract symptoms
Lower urinary tract symptoms
- These include: weak stream, hesitation or slowness in getting your urinary stream started, urgency to go to the bathroom, increased frequency to go to the bathroom
- Symptoms are related to two things:
- 1 – Functional obstruction of the urethra (that’s the tube we urinate through, the tube that comes out of the tip of the penis)
- The first part of that tube passes right through the middle of the prostate
- So as the prostate enlarges, it can compress that channel, and that can result in a weak stream; it can result in dribbling and straining
- Above the prostate is the bladder, and the bladder is a bag (a storage device) that is muscular
- As the diameter of the urethra narrows with increasing [prostate] size, that muscle will have to work harder
- Compliance will go down
- And when the compliance of the bladder goes down, the capacity can go down and the increased urgency to go to the bathroom will go up (because it’s less stretchy)
- 2 – As we get older, parts of the prostate will grow
- Oftentimes, that growth of the prostate results in narrowing of the channel
- That can commonly lead to thickening of the bladder wall, and then that results in a whole constellation of urinary symptoms, which can be managed
- Many, many men have them
- That can commonly lead to thickening of the bladder wall, and then that results in a whole constellation of urinary symptoms, which can be managed
Behavioral modifications to help manage nocturnal urinary frequency and other lower urinary tract symptoms [8:30]
The first steps in the medical management of lower urinary symptoms
- This is an area where the surgeon (urologists) does both the medical management and the surgical management
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Ted Schaeffer, M.D., Ph.D.
Edward (Ted) Schaeffer graduated from the University of Chicago in 2001 with his M.D. and Ph.D. He completed his internship in general surgery followed by a residency in urology at Johns Hopkins. He is a board certified urologist with an active practice specializing in prostate cancer.
Dr. Schaeffer is Chair of the Department of Urology at Feinberg School of Medicine and Program Director of the Genitourinary Oncology Program at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. His globally recognized prostate cancer research focuses on at-risk populations, diagnosis, treatment outcomes, and the molecular biology of lethal prostate cancer. [Northwestern Medicine]
Twitter: #EdwardSchaeffer
Website: TedSchaefferMD.com



