If you’re reading this, you probably know that I’m obsessed with longevity. But to really understand longevity, you must understand metabolic health, insulin resistance and, by extension, one of its end-results: type 2 diabetes (T2D). Though my medical practice does not focus on type 2 diabetes, I have taken care of several patients with T2D over the past few years. When I was in medical school I was taught many things about T2D, but one stands out most: T2D is incurable, I was told. Once you have it, you’ve always got it, and the best one can do is “manage” it as a chronic—but irreversible—condition.
But is this really true? Asked another way, is T2D reversible?
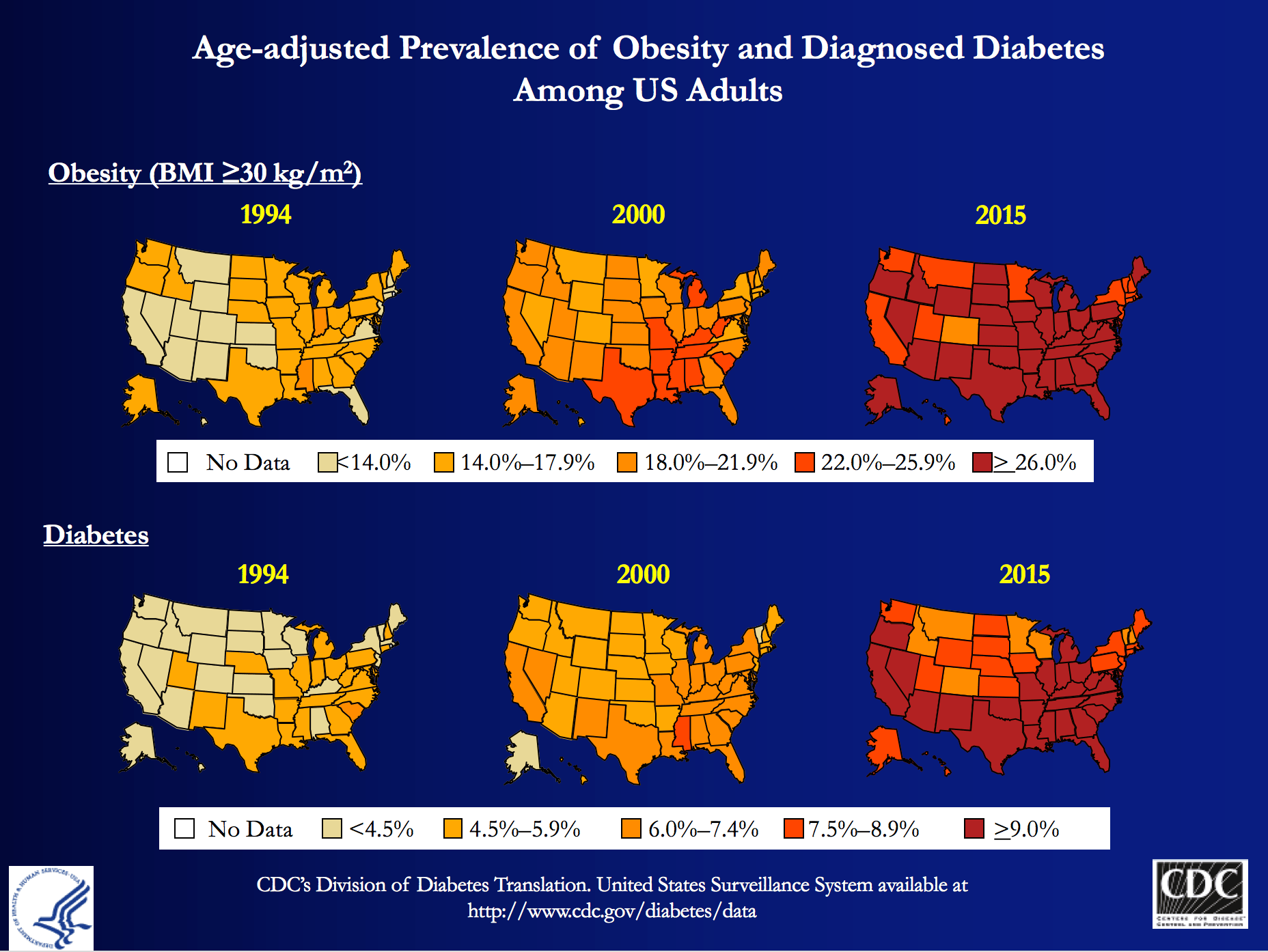
My obsession is partly due to my personal journey to better metabolic health, which I’ve documented elsewhere on this blog, and spoken about publicly. But those facts alone, don’t fully explain why I wanted to be involved with Virta Health (I’ll get to them shortly). T2D is a massive societal problem that has the potential to literally bankrupt countries: More than 29 million Americans have T2D and more than 80 million are pre-diabetic. And whether you view it through the lens of population health, or the lens of an individual patient, T2D is perhaps the biggest healthcare challenge of our generation.
At the population level, T2D costs Americans more than $300 billion per year: one of every three Medicare dollars is spent on T2D, and one of every six healthcare dollars is spent on T2D. At the individual level, patients and payers (employers and insurance companies) spend thousands of dollars (often more than $10,000) in annual expenses for medications and procedures with significant side effects, and much higher risk of developing cardiovascular disease, cancer, Alzheimer’s disease, blindness, amputation and kidney disease.
The traditional approach—which is clearly not working—is to “manage” this chronic condition with medications and the ever-ubiquitous “eat-less-avoid-fat-exercise-more” lifestyle interventions. At best, this approach only slows down the progression of the disease. Furthermore, many diabetes drugs have their own side-effects and diabetes management has a dismal diabetes reversal rate of about 1%. To date, the only clinically proven way to reverse T2D has been bariatric surgery, which is costly and not without risk. If one great thing has come from bariatric surgery, besides the obvious help to those have been successfully treated, it is that any physician or scientist paying attention to the results can’t help but notice that the reversal of T2D in these patients post-operatively seems uncoupled from their weight loss. In other words, adiposity, while correlated with T2D, is not likely the cause.
Every doctor has his (or her) “Patient 0”—the one who really got him (or her) thinking. I’d like to introduce you to mine, RB. When I met RB, he was a 37 year-old Mexican man with a family history of T2D who had a “high” glucose level on a screening blood test. His two-hour oral glucose tolerance test (OGTT) is below.

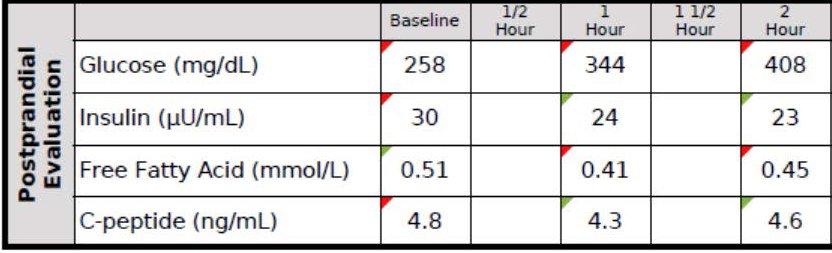
You don’t have to read these for a living to see this isn’t ideal. As you can see, his fasting glucose was 258 mg/dL and his fasting insulin, 30 uU/mL. When given 75 g of glucose, his glucose rose to 344 mg/dL at 60 minutes and 408 mg/dL at 120 minutes, all the while his insulin level fell from 30 to 24 to 23. These numbers alone confirm the diagnosis of T2D. But if we needed more evidence, his HbA1C was 9.7%, corresponding to an average blood glucose of 232 mg/dL (today the diagnosis of T2D is defined by HbA1C >= 6.5%, but I much prefer to use OGTT).
Ordinarily, for a patient with this degree of disease and beta-cell fatigue, I would have opted for at least two drugs, metformin (cheap) and a DPP4 inhibitor (not cheap) and most doctors would have gone straight to insulin, as well. However, due to the patient’s financial circumstances, we opted to only use metformin and dietary modification. The patient worked very long hours in construction and, frankly, was pretty much exercising all day, so there was no way adding more exercise to his day was going to work. If we were going to fix him, it had to be through nutrition. I spoke with one of my mentors, Dr. Naji Torbay, a remarkable endocrinologist who has the largest diabetes reversal program in Dubai and Lebanon, about this case. Even he thought it would be tough, but he’d reversed cases like this, so we gave it a shot.
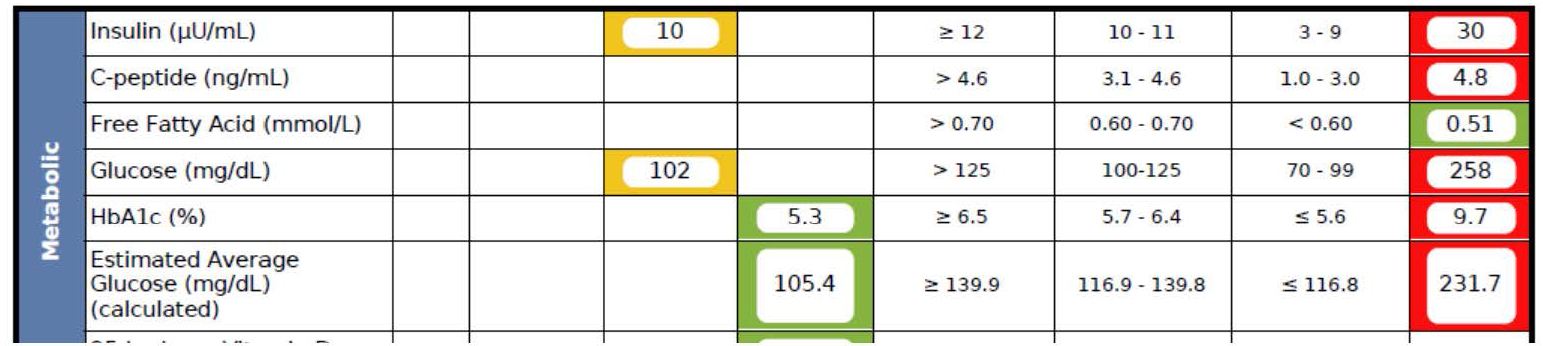
What happened over the next 5 months surprised me, as even I did not anticipate the alacrity of RB’s reversal. Below is a snap shot of RB’s labs from March 1, 2016 about 5 months after the OGTT, above. On the right side you can see the results from September 28, 2015, including the HbA1C of 9.7%, the fasting glucose of 258 mg/dL, and the fasting insulin of 30 uU/mL (HOMA-IR calculated at 19.1).
As you can see, the HbA1C fell to 5.3%—that’s even below the threshold of pre-diabetes—and the fasting glucose and insulin fell to 102 and 10, respectively (HOMA-IR calculated at 2.5).
RB doesn’t have diabetes any more. RB will avoid the amputations that destroyed the lives of his family. RB will not die prematurely from heart disease in his 50s. RB got a new lease on life.

If you think I’m telling you this story to impress you, you’re mistaken. Countless doctors (though not enough) know how to do what I did with RB—it’s actually simple biochemistry, and if a former surgeon like me can learn it, certainly anyone can, as long as one has the ability to frequently and safely manage medications and guide necessary behavior change. But sadly, most people like RB don’t have this option, and even if I and countless other doctors devoted the rest of our lives to helping everyone like RB out there, we could not put a dent in this problem, which is where Virta Health comes in.
Disclosure: I am an advisor to Virta Health and I have invested in the company, because I believe their approach is the best one to solve this problem—not the other way around.
Is it possible to deliver systematic diabetes reversal results (like the case above) safely, sustainably, and at scale among average diabetics?
Of course, even with the correct biochemical/nutritional approach, there are number of challenges to make T2D reversal possible at scale:
- Eliminating diabetes medications safely requires day-to-day (not monthly) careful adjustments by a physician. This is not how physicians work and would not be cost-efficient.
- Anything nutrition related requires a very high degree of individualization based on health status, lifestyle preferences and other life circumstances. For the 1% DIY’ers (who probably disproportionally read blogs like this one) any extreme approach can work, but at a population level, it won’t be enough.
- Both the patient and physician would need near real-time biomarker (e.g., CGM) data to adjust meds and the overall intervention. [By the way, I get asked all the time—mostly on Twitter—what CGM is…for those about to ask, here you go.]
- All behavior change and lifestyle interventions have failed at scale because only a small fraction of the population is able to DIY through complex decisions in today’s environment and life circumstances. This would require a near real time “personal coach” who can address any situation (e.g., family struggle, travel, new job, holidays).
It appears that we may be a step closer to somebody solving this challenge. Today, the first results of a T2D reversal clinical trial were published in the Journal of Medical Internet Research that show a promising new way to look at T2D: it is reversible in a large percentage of average patients, safely and sustainably. The trial was conducted by Virta Health, an online diabetes reversal clinic, which uses technology and artificial intelligence to solve the above mentioned care delivery challenges. The entire intervention is managed by physicians and the nutritional approach is based on highly individualized carbohydrate restriction and nutritional ketosis (which I’ve written about extensively in the past and throughout this blog).
The trial took place in Lafayette, IN, in partnership with Indiana University Health. A total of 262 women and men with T2D enrolled in the Virta Clinic. Average age was 54 (Stdev: 8); BMI 40.8 (Stdev: 8.9) and two-thirds of the patients were female. The trial will continue for at least two years, and data from the first 70 days were published today.
After just ten weeks:
- 56% of the diabetics enrolled achieved an HbA1C below the diabetic range (6.5%), while eliminating hypoglycemic medications
- Almost 90% of insulin users had it either completely eliminated (close to 40%) or reduced
- Mean body mass reduction was just over 7%, which is quite significant, but also shows that diabetes can be reversed before massive weight loss (i.e., it’s not the obesity that causes type 2 diabetes, which is consistent with the gastric bypass literature)
- Patient completion rate was >90%, which is remarkably high in an outpatient-based intervention.
- Reported feelings of hunger decreased from the pre-trial level (this seems to be a strong indication that will-power driven caloric restriction was not a factor in weight loss)
- Importantly, there were no serious adverse events, no incidence of symptomatic hypoglycemia, and no incidents of ketoacidosis.
The trial is ongoing with one-year data expected to be published shortly.
Yes, this is only one clinical trial and 70 days is not very long, but these data force us to consider that there is another way to look at T2D: it is not a chronic condition that gets progressively worse. With the combination of the right science and technology, it can be reversed at scale and among average diabetics. Clearly we need to look at the long-term success, and see many more patients succeed safely, but this is more promising than anything I have ever seen. I’ve seen some of the preliminary 1+ year analysis and the results look very impressive. I look forward to sharing them as they become publicly available.
If you are interested, you can learn more about Virta and their diabetes reversal science here. I’m excited to be a very small part of this organization and I look forward to the day when every patient with T2D at least has the chance to try an approach that can potentially reverse their condition.