In this “Ask Me Anything” (AMA) episode, Peter and Bob dive deep into cancer screening, including why it’s important, what you need to know about a test, and Peter’s approach with patients. They specifically discuss various screening methods, explain important terms like sensitivity and specificity, and how layering and stacking different tests in tandem can improve predictive values. They conclude with a discussion on one of the more exciting screening tools, diffusion-weighted MRI, and how it’s changing the cancer screening landscape.
If you’re not a subscriber and listening on a podcast player, you’ll only be able to hear a preview of the AMA. If you’re a subscriber, you can now listen to this full episode on your private RSS feed or on our website at the AMA #25 show notes page. If you are not a subscriber, you can learn more about the subscriber benefits here.
We discuss:
- The importance of cancer screening [1:15];
- Cancer screening terms: sensitivity, specificity, false positives, and false negatives [8:25];
- Cancer screening terms: positive and negative predictive value [17:00];
- Improving predictive value by layering tests, and the predictive values of mammograms [25:45];
- How smoking impacts the predictive value of cancer screening [30:45];
- Liquid biopsies for ruling out cancer and the blind spots of common cancer screening tests [33:00];
- The difference between cancer originating from inside versus outside the body [41:15];
- How diffusion-weighted MRI is changing cancer screening [45:15];
- Summary of Peter’s approach to cancer screening [53:45]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
The importance of cancer screening [1:15]
Some subscriber questions covered in this podcast:
- How do you think about cancer screening?
- Why and or when should I be screened?
- Which tests are worth getting?
- What do you think of liquid biopsies?
- How do you interpret sensitivity and specificity of tests? What do those actually mean?
- What are some screening tools for cancer you use in your practice?
- Can you discuss how you categorize cancers and how you screen for each?
- What’s the difference between cancers outside the body versus cancers inside the body?
Addressing the first question: How do you think about cancer screening?
Longevity has these two components—they’re not independent—but sometimes, it’s helpful to think about them in isolation:
- Lifespan—How do you live longer?
- Healthspan—How do you live better?
- Major diseases that rob a person of lifespan include cancer, atherosclerotic diseases, and the diseases of dementia and neurocognitive decline
- The latter two go more hand in hand with the reduction in health span
- By definition, when a person has Alzheimer’s disease, their quality of life i.e. their cognition) is also deteriorating–So they’re experiencing both the slide in quality of life and eventually length of life
- Similarly in people that have advanced atherosclerosis, a lot of times the reduction in the ability to carry out activities of daily living kind of moves more hand in hand with that
- In the case of cancer, health span decline is a little less the case
- Age is the greatest risk factor for cancer just as it is for the other two diseases
- But in some ways it’s a little bit easier to think of cancer in isolation from the health span stuff
- if you’re trying to imagine a world in which you can live longer… that means living in a world where we delay the onset of chronic disease and/or have better tools to live longer with chronic disease
- Peter much more favors the former option (i.e., delay) because we’ve basically spent most of the history of modern medicine working on the latter option with very, very limited success.
Screening
- One of the pillars of longevity is minimizing mortality from cancer
- So where does screening fit into this?
- Screening is one of three pieces
- First piece would be, how do you prevent cancer?
- The second thing would be, how do you screen for cancer and detect it early?
- And the third is, how do you treat it when you have it?
Focusing on the prevention piece…
- Why does Peter believe that screening is an important pillar?
- The simplest explanation for why screening matters is the evidence that suggests that a cancer that is caught earlier is easier to treat than a cancer that is caught later
- For instance, if you catch a breast cancer or a colon cancer when there are tens or hundreds of millions of cancer cells, your odds of treating that successfully are better than if you catch the same cancer years later, when there are billions of cells
- The evidence for that basically comes from examining how patients respond to the exact same drugs in the adjuvant setting versus in the metastatic setting
- The adjuvant setting is when a drug is given to a patient who has no visible cancer
- So if you believe that they have microscopic disease that remains, and you give them a drug like Herceptin for a HER2/neu positive breast cancer
- If you compare the outcomes of those patients to the outcomes of patients who are given the exact same drug for the exact same phenotype and genotype of the cancer, but in the metastatic setting, there’s no comparison in the outcomes
- Possible explanation for the difference in success rates:
- One explanation for that may be that the cancers that have been around longer have developed more mutations
- It is therefore Peter’s belief that the more we can do to screen for cancer and catch it earlier, the better we will be
Screening frequently comes with a price:
- We pay a financial price for that
- And we pay potentially an emotional price
- We have to now get into false positives and false negatives
Looking at five-year survival stats…
- Take breast cancer—If you catch it early and it’s a local cancer and it hasn’t metastasized, the five-year survival rates are 99%
- But for metastatic breast cancer, five-year survival is about 28%
Cancer screening terms: Sensitivity, specificity, false positives, and false negatives [8:25]
Sensitivity

Figure 1.
- Sensitivity is the probability that the test yields a positive result for someone who has the condition of interest
- A sensitive test is likely to detect a person who has COVID if they’re tested
A realistic example: Mammography
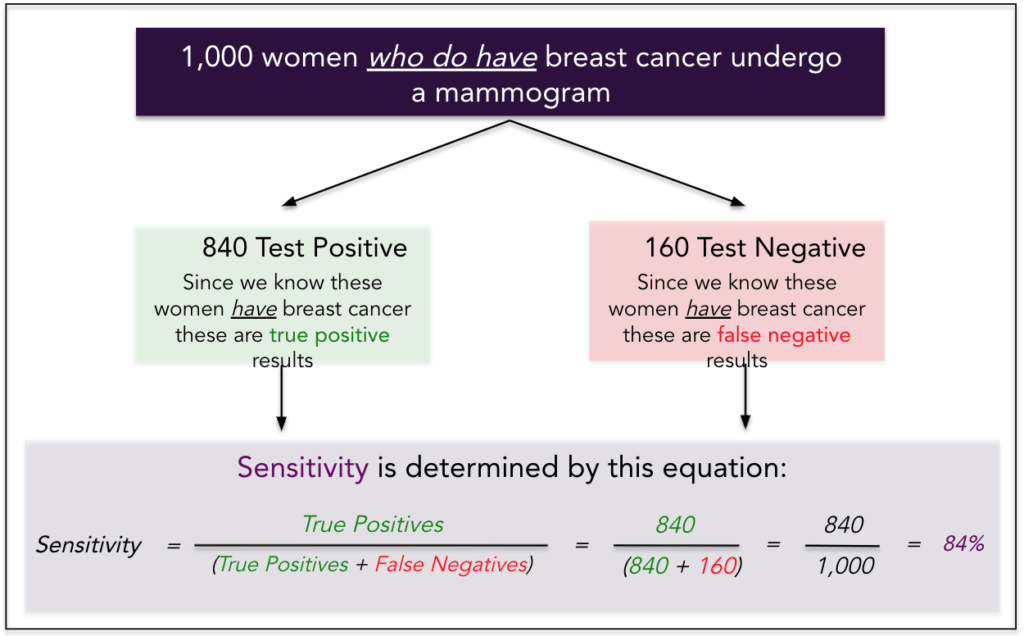
Figure 2.
- we are now talking about 1,000 women who have breast cancer
- if you were to run a mammogram on them, 840 of them would have a positive mammogram
- the radiologist would read that and say, “this woman has breast cancer.” So those are true positives.
- In this example, 160 of those women would have their mammogram read as negative
- And these would be false negatives
- Sensitivity is defined as the true positive rate over the total number of cases
- True positives plus the false negatives, which in this case yields 84%.
- a very, very, very sensitive test would always have caught the people who have the condition
- Best case scenario here is a 100% sensitive test that would detect 1,000 of those women, and none of them would be false negatives
With sensitivity, you have to understand that it’s basically backwards looking
- With specificity, by contrast, you truly know who has cancer, who doesn’t have cancer, when we get into specificity
- when you look at sensitivity, you already know what the result is when somebody, after they get screened and you know the results
- But in the case of sensitivity, if the test is negative, you know it’s wrong. You know it’s a false negative, just because we’re looking at a group of people where you already kind of have the answer in hand with sensitivity
- with specificity as you’ll see in a moment, it means that you actually have forward-looking data to know that a negative is truly a negative
Specificity
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.




