Robert (Bob) Gatenby is a radiologist who specializes in exploring theoretical and experimental models of evolutionary dynamics in cancer and cancer drug resistance. He has developed an adaptive therapy approach for treating cancer which has shown promise in improving survival times with less cumulative drug use. In this episode, Bob explains what brought him into medicine, his search for organizing principles from which to understand cancer, and the mathematical modeling of other complex systems that led him to model the dynamics of tumor cell changes in cancer. He discusses his pilot clinical trial treating metastatic prostate cancer, in which he used an evolutionary game theory model to analyze patient-specific tumor dynamics and determine the on/off cycling of treatment. He describes how altering chemotherapy to maximize the fitness ratio between drug-sensitive and drug-resistant cancer cells can increase patient survival and explains how treatment of metastatic cancer may be improved using adaptive therapy and strategic sequencing of different chemotherapy drugs.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Bob’s unlikely path to medicine and his disappointment with his medical school experience [1:45];
- Rethinking the approach to cancer: using first principles and applying mathematical models [12:15];
- Relating predator prey-models to cancer [26:30];
- Insights into cancer gathered from ecological models of pests and pesticides [32:15];
- Bob’s pilot clinical trial: the advantages of adaptive therapy compared to standard prostate cancer treatment [41:45];
- New avenues of cancer therapy: utilizing drug-sensitive cancer cells to control drug-resistant cancer cells [48:15];
- The vulnerability of small populations of cancer cells and the problem with a “single strike” treatment approach [56:00];
- Using a sequence of therapies to make cancer cells more susceptible to targeted treatment [1:05:00];
- How immunotherapy fits into the cancer treatment toolkit [1:15:30];
- Insights into why cancer spreads, where it metastasizes, and the source-sink trade off of cancer [1:20:15];
- Defining Eco- and Evo-indices and how they can be used to make better clinical decisions [1:29:45];
- Advantages of early screening for cancer [1:40:15];
- Bob’s goals for follow-ups after the success of his prostate cancer trial [1:42:15];
- Treatment options for cancer patients who have been told they have “failed therapy” [1:51:15];
- More.
Bob’s unlikely path to medicine and his disappointment with his medical school experience [1:45]
- Peter stumbled across Bob’s work preparing for another podcast
- The article in Wired about his new approach to treating cancer quickly captivated him
- Originally, Bob wanted to be a physicist
-
- After working with some great physicists, he came to the conclusion that he wasn’t smart enough
- It was the Vietnam war era and going to medical school was considered something that was really for humanity; he decided to do that
- He was at Princeton as an undergrad in the late sixties-early seventies
- Peter notes Richard Feynman did his PhD at Princeton too, and undergrad at MIT
- There was the shadow of Feynman there in the late sixties because he had just won his Nobel prize in ‘65
- Wheeler was still the department chair; he was one of the great physicists of his generation
- Bob’s TA won a Field Medal; it’s only awarded every 4 years
- He was surrounded by really smart people
- It was an intellectually exciting to be there at the time
- Dr. Witten was there; he was very involved in string theory
- Going into medicine seemed like the right thing to do in that era
- Many people, including him, had the desire to help people
Medical school and how doctors think
“I think that’s another part of your story that I can relate to…I realized very quickly that in biology, you couldn’t think your way out of every problem the way you could in math or physics or engineering.” – Peter Attia
- Bob discovers in his first semester in medical school, in histology that he cannot intuit his way through this class; he has to memorize everything
-
- This foreshadowed some other issues he had with his medical journey
- It brought him back to his previous 12 years of Catholic school, with catechism; this kind of rote memorization
- He found similarities between clinical medicine and catechism; when asked the scripted question, one is required to make the scripted answer
- He remembers one scripted question – why do cancers grow
-
- The scripted answer was, because cancer cells grow faster than normal cells
- And that’s totally wrong, on so many levels that it’s hard to believe
- Medical school was less scientific than he expected
- Almost like a trade school in the sense of learning from masters the way to do things
- The scripted answer was, because cancer cells grow faster than normal cells
- It’s very difficult to get physicians as a group, to stop talking dogma and simply think
-
- Memorizing becomes their way of thinking in medical school
- Bob finds that for things that have been done the same way for the last 5 decades, questioning it doesn’t go over well with physicians
- This is discussed in books such as The Doctor’s Plague and The Ghost Map
- The story of Ignac Semmelweis, a physician in the 1800’s who pioneered handwashing and antiseptic techniques
- Mid 19th century, the medical community was very, very conservative; and even moving them toward washing hands or using a septic technique took decades
Semmelweis died in an insane asylum for having been so rejected and cast out by the medical community
- Peter relates a story from his medical training, during his residency (6-7 years into his training)
- He’s looking for any excuse to apply mathematics to problem solving
- One of his critical care fellows in the ICU rotation (an anesthesiologist) had a PhD in math
- He was the first person who could really put all of the critical care equations into their truest form of physiologic differential equations
- He didn’t just explain the dogma but could really show you the theory
- Peter and he would stay up late, forgo sleep, and talk really deep about medicine
- Months later Peter became dumbfounded at how naively they would dose antibiotics, based on guessing decay times
- He thought there must be a more accurate way to do this
- There were equations that could accurately describe how the plasma concentration of gentamycin would decay; all that was needed was a few more data points
- In the course of a couple weeks, he built a model that would predict the exact right time to be checking nadir levels to re-dose
- When he attempted to implement this he was met with huge resistance and was actually threatened to be fired by one of the attendings
- This response does not surprise Bob
- When he attempted to implement this he was met with huge resistance and was actually threatened to be fired by one of the attendings
Rethinking the approach to cancer: using first principles and applying mathematical models [12:15]
What drew Bob to radiology, then radiation oncology?
- He liked the intellectual exercise, the puzzle of it
- He was a very shy, retiring kid; dealing with patients was very difficult; it was a lot easier to work with films
- It was really one of the few things about school that he liked
When did he start thinking about cancer differently?
- His first job was at the Fox Chase Cancer Center in Philadelphia
- His desire to help people was especially strong here because the disease is so awful
- He spent lots of time learning about cancer, reading textbooks, reading the journal Cancer Research, the flagship journal of the AACR
- He asked himself how different studies on cancer fit together
- He noticed there were no organizing principles; studies were simply making a series of observations and each was quite separate
- In the physics world, observations ultimately led to the development of organizing principles, a first principle
- Observations of planetary motion and data observed by Tycho Brahe, then Kepler developed a kind of geometric interaction, and ultimately Newton developed the first principles that could put this all together
- One can make the case with Einstein’s work around the photoelectric effect
- Most people think Einstein won the Nobel prize for relativity, but it was actually for the photoelectric effect
- He was not the first to observe it but the first to upt it all together
{end of show notes preview}
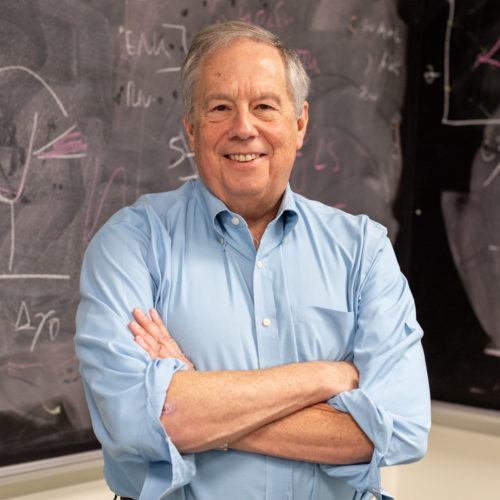
Robert Gatenby, M.D.
Robert (Bob) received a B.S.E. in Bioengineering and Mechanical Sciences from Princeton University and an M.D. from the University of Pennsylvania. He completed his residency in radiology at the University of Pennsylvania where he also served as chief resident. Bob remains an active clinical radiologist specializing in body imaging. While working at the Fox Chase Cancer Center after residency, Bob perceived that cancer biology and oncology were awash in data but lacked coherent frameworks of understanding to organize this information and integrate new results. Reaching back to his training in engineering and physical sciences, Bob recognized that cancer was a complex dynamic system (similar, for example, to weather) and that understanding the often nonlinear interactions that govern such systems requires mathematical models and computer simulations. As a result, most of Bob’s subsequent research has focused on exploring mathematical methods to understand the first principles and key parameters that govern cancer biology and treatment. In 2008, Bob joined the Moffitt Cancer Center as chair of radiology and convinced the leadership to add a group of mathematicians to the faculty and form the Integrated Mathematical Oncology (IMO) department. Now numbering 8 faculty mathematicians and over 20 post docs and grad students, the IMO has catalyzed formation of several disease-oriented teams of oncologists, surgeons, pathologists, radiologists, mathematicians, physicists, cancer biologists, imaging scientists and evolutionary biologists. These multidisciplinary groups are investigating virtually every aspect of cancer biology and therapy. In fact, IMO members are co-PIs of two ongoing clinical trials that use evolutionary dynamics and computational models to guide therapy. There is no other cancer center in the world that has so completely integrated mathematical modeling and computer simulations into basic science and clinical research.




This is a fascinating line of reasoning. It makes so much sense and has so much explanatory power. I sincerely hope the oncology world can begin to understand this ecological approach to treatment. I’m filing it away as something to consider if I or my immediate family ever need to face chemotherapy.