In this “Ask Me Anything” (AMA) episode, Peter dives deep into the topic of atherosclerotic cardiovascular disease (ASCVD)—the number one killer in the developed world. Peter argues for the importance of paying attention to and understanding ASCVD given its ubiquity and inevitability. He goes into great detail about the development of atherosclerosis and how it can take hold at a very early age, the role of cholesterol, and the causal factors of ASCVD that determine prevention strategies. Additionally, he discusses the important metrics and biomarkers found in blood work, as well as diagnostic tests such as coronary artery calcium scores (CAC) and CT angiograms which help to determine the level of arterial damage present. Finally, Peter lays out the keys to understanding and interpreting calcium scores before wrapping up the conversation with his key takeaways regarding prevention.
If you’re not a subscriber and listening on a podcast player, you’ll only be able to hear a preview of the AMA. If you’re a subscriber, you can now listen to this full episode on your private RSS feed or on our website at the AMA #34 show notes page. If you are not a subscriber, you can learn more about the subscriber benefits here.
We discuss:
- The importance of understanding atherosclerosis early in life [2:15];
- Defining atherosclerotic cardiovascular disease (ASCVD), its causes, and the role of cholesterol [9:00];
- The process of developing ASCVD, part 1 [15:00];
- The process of developing ASCVD, part 2 [24:00];
- The process of developing ASCVD, part 3 [32:45];
- How early in life ASCVD can start to develop [40:30];
- Case studies of atherosclerosis and figures showing real pathology [43:00];
- Coronary artery lesions present in autopsies of different age groups [49:15];
- The causal factors of ASCVD that determine prevention strategies [52:15];
- Labs to identify biomarkers of ASCVD [59:00];
- Diagnostic tests to determine the level of arterial damage present—CAC, CTA, CIMT, and more [1:00:30]
- Calcium scores: keys to understanding and interpreting a CAC score and/or CTA results [1:05:15];
- Is there a risk from cholesterol levels being too low? [1:13:00];
- Key takeaways regarding prevention [1:15:45];
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
The importance of understanding atherosclerosis early in life [2:15]
Atherosclerosis is ubiquitous
- It’s the only disease that is inevitable, and it limits human longevity
- Cancer and dementia, also diseases of old age are not inevitable the way atherosclerosis is
“Not everybody dies from atherosclerosis, but… everybody dies with it”— Peter Attia
- You want to understand this because the impact is huge and the tools we have are also huge
- Extending lifespan comes down to delaying the onset of chronic disease, and atherosclerosis is the most common chronic disease
2 main paths to atherosclerosis
Risk factors
- Smoking, a behavioral risk factor (we’ll put this aside for the moment)
- 1 – Hypertension
- 2 – High blood and lipid abnormalities (we’ll focus on this one)
- This leads to atherosclerotic cardiovascular disease (ASCVD)
Studies of pathology show ASCVD begins at a young age
What is the most common presentation for a 1st heart attack?
- Sudden death
- A 1st heart attack in over 50% of people is fatal; today this number is a little less but still staggering
What is the age distribution of people who have their 1st major adverse cardiac event?
- Adverse cardiac events are a heart attack or a stroke (or death)
- Figure 1 shows the incidence of cardiovascular events for both males and females in the US
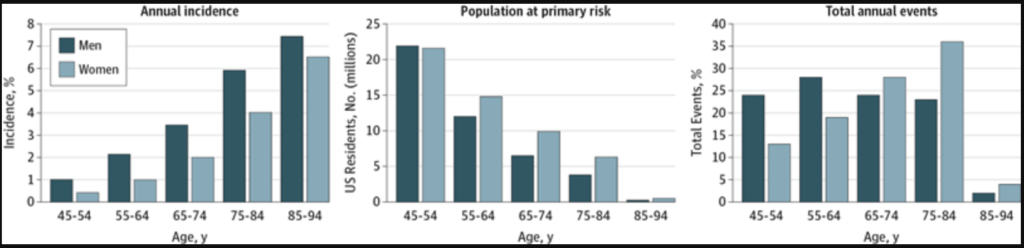
Figure 1. Incidence of cardiovascular events by age and sex. Credit JAMA Cardiology 2016
- The graph on the right shows total annual events
- The 1st 2 sets of bars show the number of events for people under 65
- Men are shown in the darker bars comprising slightly below 25% and slightly above 25% of all cardiac events
- The implication is that 50% of men who are going to have a cardiac event in their life will have it before the age of 65
- For women, a third of women will have their 1st cardiac event before the age of 65
- The total annual events is not the whole story; it’s important to understand how long it takes for this disease to take hold
- Early prevention is key
- Almost 25% of these events are in men younger than 54
- When you think of someone who is 45, 50, this disease didn’t start 2 years before
When you see these stats laid out, it creates a shift in your mind around why you should care about this
Defining atherosclerotic cardiovascular disease (ASCVD), its causes, and the role of cholesterol [9:00]
ASCVD is disease state characterized by the deposition or the buildup of cholesterol (sterols) in the artery wall
- It begins with a fatty streak that later consolidates into plaques that can ultimately lead to a reduction in blood flow
- Reduction in blood flow is called ischemia
- Ischemia results in tissue damage to the heart and this is what results in a heart attack
- A heart attack can be fatal depending on the amount of cardiac tissue that is damaged from loss of oxygenation
Causes of ASCVD
- You don’t have to be obese or have high blood pressure
“It’s really a question of the cholesterol in your blood. That’s really what defines the disease.”— Peter Attia
- Atherosclerosis is defined by the presence of cholesterol in the artery wall
- This is not necessarily related to the measurement of cholesterol in circulation
- Patients with cholesterol in their arteries do not necessarily have to have co-aggravating factors such as: high blood pressure, diabetes, obesity, family history, smoking
- All these things that exacerbate ASCVD
Cholesterol explained
- Cholesterol is an organic molecule, a type of lipid
- It is not soluble in water
- It is a hydrophobic molecule
- Picture pouring oil into water and you would immediately see what it means to have a hydrophobic substance in contact with something that is hydrophilic (water)
- They repel each other
Cholesterol is about one of the most important molecules in the body
- You would die without it
- Rare genetic conditions that impair the ability to make cholesterol are fatal
- Cholesterol is used for 2 main things:
- 1 – The cell membrane of every cell in the body contains cholesterol
- Cholesterol contributes to the fluidity of the cell membrane, important for membrane channels that allow things in and out of the cell
- 2 – Synthesis of many hormones begins with cholesterol, including: cortisol, estrogen, testosterone
- It is also essential for the creation of bile acids, necessary to digest food
Where does cholesterol come from?
- Most people think of cholesterol as something that comes from eating certain foods
- This is true, eggs contain cholesterol
- But the cholesterol in your bloodstream has little to do with the cholesterol in foods you eat
- The reason is, the cholesterol we eat in esterified, it has a chemical bond that swings between an intermediary oxygen and another side chain
- This cholesterol is too large for the receptors in our gut to absorb
- Most of the cholesterol we eat is excreted
Most of the cholesterol we will discuss [in our bloodstream] is made in our body and transported between cells through lipoproteins
The process of developing ASCVD, part 1 [15:00]
Anatomy of blood vessels
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.



