This week an article titled Primary Prevention of Cardiovascular Disease with a Mediterranean Diet was featured in the New England Journal of Medicine. The study received a considerable amount of attention, including an article in the NY Times.
Study design
The objective of this study, as its name suggests, was to study the impact of a Mediterranean Diet on the primary prevention of CVD. Primary prevention of X implies looking at patients (ideally those susceptible to X) who have not yet had X to see if your intervention prevents X. Such trials are more difficult (i.e., larger and more expensive) than secondary prevention trials because in secondary prevention trials you start with patients who have already had X and are therefore at much greater risk of having X again.
Let’s use a relevant example. A primary prevention trial for CVD would study subjects who have never had a heart attack or stroke, and look for which treatment (e.g., a drug like a statin) reduces the number of such events (sometimes called MACE – Major Adverse Cardiac Events). A secondary prevention trial would study subjects who have already suffered some MACE and look at interventions to prevent a recurrence.
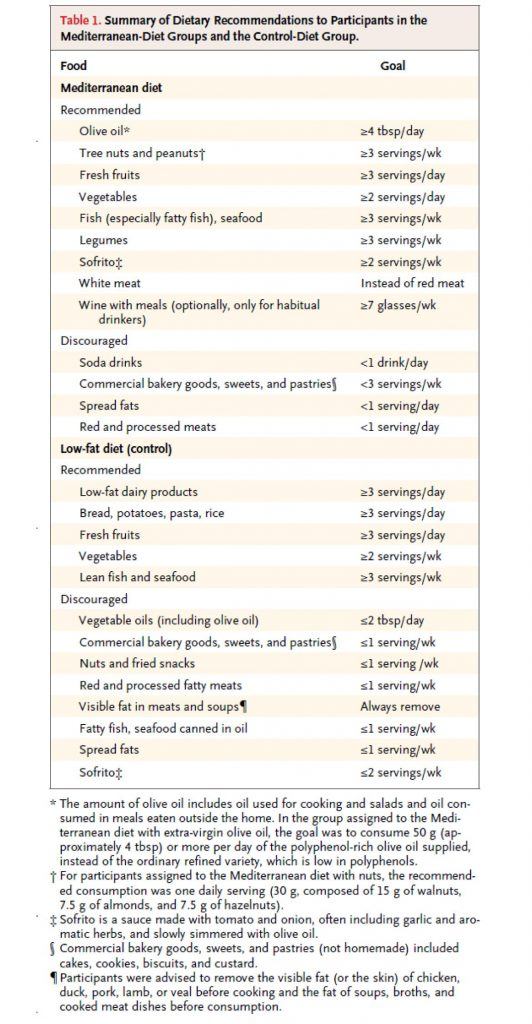
This study, a primary prevention trial, enrolled about 7,500 patients who were at high risk for CVD, but who had not suffered any MACE, and randomized them to one of three diets – two variants of a Mediterranean Diet, and a low fat diet. Table 1 shows the dietary targets. The two variants of the Mediterranean Diet were (i) one that emphasized extra virgin olive oil (EVOO) and (ii) another that emphasized nuts.
(As an aside, my 40th birthday is coming up soon and my wife suggested to my daughter that they make me a cake for my birthday. My daughter – who loves cake, of course – objected immediately by saying, “Mommy, we can’t do that…Daddy hates sugar!” A few minutes later she came back to my wife and said, “Mommy, wait, I have a great idea…we can make Daddy a nut cake!” Those of you who read this post may recall the last point I made. Suffice it to say, if I were in this study, I would have done really well on the nuts arm, though I think I eat closer to 5 or 6x the amount they were recommended per day.)
As you can see all three arms were discouraged from consuming bakery goods, sweets, pastries, red meat, processed meats, and spread fats. The authors report compliance data, but not biomarkers (if I wasn’t so short on time, I’d go back and read the other publications of this study which likely show biomarkers – e.g., insulin, glucose, HDL-C, and triglycerides – which are pretty good for confirming compliance, especially HDL-C).
So, macro point #1 is this:
Everyone in this study, almost by necessity, was consuming a very healthy diet relative to their baseline diet (if you believe most folks were on a “standard” diet, or worse yet, a poor diet, prior to enrollment, which I do). I’ll come back to this point later, but it’s worth remembering this as you read on.
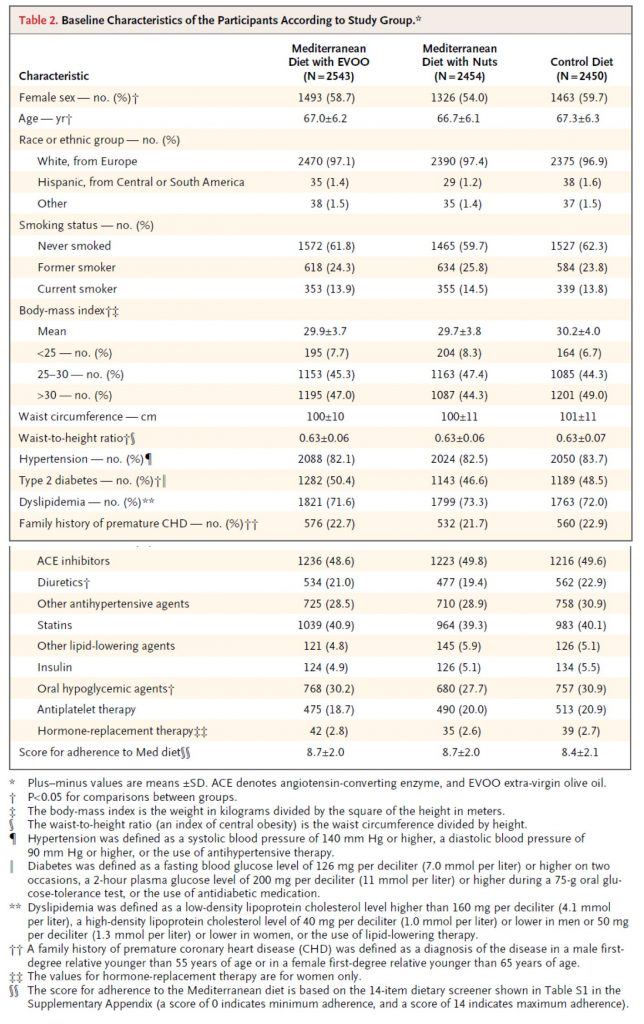
Table 2, below, shows you the baseline characteristics of the subjects in each arm. I must admit, before I saw the results of trial, but knew it was going on, I was a bit surprised at how audacious the investigators were. Primary prevention trials are really challenging! However, as soon as I read the inclusion criteria and saw this table I realized this wasn’t really a garden variety primary prevention trial, per se. Why do I say that? Less than 10% of the subjects were of normal weight. Less than 20% did not have high blood pressure. 50% had type 2 diabetes. Less than 30% had normal lipid profiles (presumably defined by LDL-C and HDL-C cutoffs). Over 40% were taking statins. You get the point. Virtually everyone enrolled in this study had metabolic syndrome.
This is not a criticism of the study, to be clear. It’s merely a statement of why this study, I believe (and hopefully will make a case for), showed a treatment effect in the setting of primary prevention with a dietary intervention. In fact, this is exactly what the authors sought in the enrollment. They specifically looked for high risk patients who had not yet suffered a MACE. In my humble opinion, this was a very good choice for two reasons:
- If they selected healthy subjects, they would have needed 5-10x the number of subjects, and
- This patient population is in desperate need of dietary intervention.
So, my only minor critique of this is the semantics of calling this a primary prevention trial. It would be more accurate to call it a primary prevention trial of patients with diagnosed metabolic syndrome.
One thing I always look for in dietary trials (and trust by now you’re also looking for) is something called performance bias, which is very common in dietary intervention trials. In fact, you’ll recall it was the main flaw of the meta-analysis I wrote about a while ago. The authors of this particular study (you can read about this in the methods section) did a good job avoiding this.
This brings me to macro point #2. This study would have been better if the “control” arm (in this study, the low fat arm), was actually a true control relative to the “standard” patient diet. For example, this might look like the following 3 arms: standard fare diet vs. low-fat diet vs. Mediterranean diet (pick one of the 2 from this study). The drawback of this approach is that patients in the “standard fare” would almost certainly have a performance bias working against them. The other two groups would have a sizable intervention effect, while this (true) control arm would be left on their own.
The final point I want to make is more of a so-called teaching point. Broadly speaking, there are two (and an emerging third) types of studies in human nutrition:
- Efficacy studies – studies that elucidate (under the strictest most controlled conditions ever used to study humans) the mechanism of action of food. In other words, these studies ask, “How does factor X or factor Y actually work at the mechanistic level in the body?”
- Effectiveness studies – studies that elucidate to what extent free-living people will adhere to a dietary change, and determine the long-term safety and effectiveness of that change. In other words, these studies ask, “Does this dietary intervention work over time, and what are the risks and benefits?”
- Econometric studies – studies that elucidate (under free-living conditions) how to change people’s behavior, by changing the defaults, the economic forces, and the cues. In other words, these studies ask, “How do we induce people to change behavior – to eat healthy — once the science provides definitive answers about what that behavior should be?”
Obviously, this study is in the second category, as virtually all “diet studies” are. I mention this for the reason that while it’s tempting to speculate on a mechanism of action in this study, there was not a single design element in this study to elucidate such things. So, at best, we are really looking at the difference between two dietary interventions.
What happened in this study?
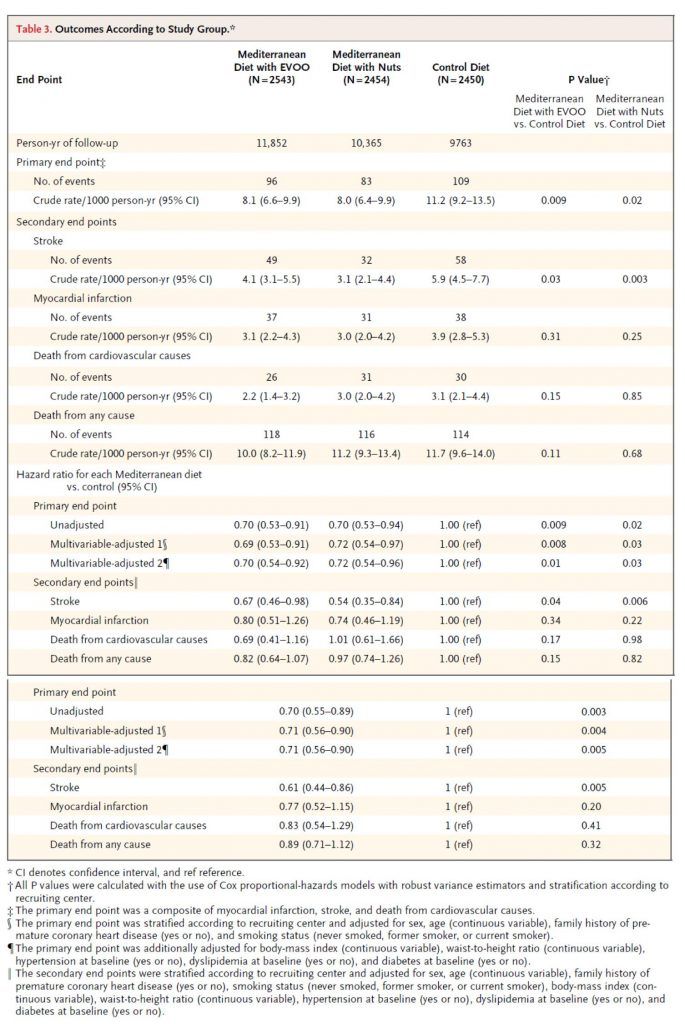
Table 3 shows the outcome of the study and commensurate hazard ratios. I won’t walk you through this table in its entirety, but I’ll show you how to read one row of each.
Consider the first row, the primary end point (recall: this was defined as a composite of myocardial infarction (MI, “heart attack”), stroke, and death from cardiovascular cause). The first row shows the number of crude events. Of course, to see this in an apples-to-apples fashion the number needs to be normalized to a common denominator, in this case events per 1,000 person-years. So, the row that’s particularly important is the one that shows 8.1, 8.0, and 11.2 per 1,000 person-years. (Note, one uses person-years to also normalize for and remove any impact of time in study.) Next to each number I’ve listed above are two numbers in parentheses. These are the 95% confidence intervals. So, even though the first is listed as 8.1, you can be “95% sure” the actual number is between 6.6 and 9.9.
How can you tell if this is “statistically significant?” Most of us don’t possess the ability to do this in our heads. So, the authors do it for us in the last two columns. The right-most column compares the control (low-fat) to the Med Diet (nuts), while the column to the left of that compares the control group to the Med Diet (EVOO). The number shown, called a p-value, is defined as the probability the difference you’re seeing is due to chance. The smaller the better, and generally a number below 0.05 is considered to earn the moniker “statistically significant.” (Not to be confused with “clinically significant,” which I’ll discuss below).
Before we go back to the other endpoints, let me comment quickly on the hazard ratio for this endpoint. A hazard ratio is essentially the probability of an event in the treatment group divided by the probability the same event occurs in the control group (hence, control groups have a hazard ratio of 1.0).
So, the hazard ratio of 0.70 means there was relative risk reduction of 30% for the Med Diet relative to the control diet. This should not be confused with absolute risk reduction, which I’ll get to shortly. For the sake of time and space, I will not go into the details of unadjusted and multivariate adjusted analyses.
But there was no difference in MI or death?
As you can see from Table 3, there was no statistically significant difference in death (CVD or otherwise) or MI across the three groups. It’s very tempting to make the following mistake:
“Hey, none of this matters, because you won’t live longer.”
Remember that pesky little statistical thing called power. This study was powered (at 80%) to detect a difference in the primary outcome, which it showed. In fact, the intention-to-treat was greater than 7,500 because the authors expected no more than a 20% relative risk reduction. But they saw a 30% difference, and the study was halted early.
So, we don’t actually know which of the following statements is correct:
- This dietary intervention does not result in a difference in MI or death; or
- It does, but this study was not large or long enough to detect it.
Very important distinction. I can’t emphasize this enough.
Back to absolute versus relative risk
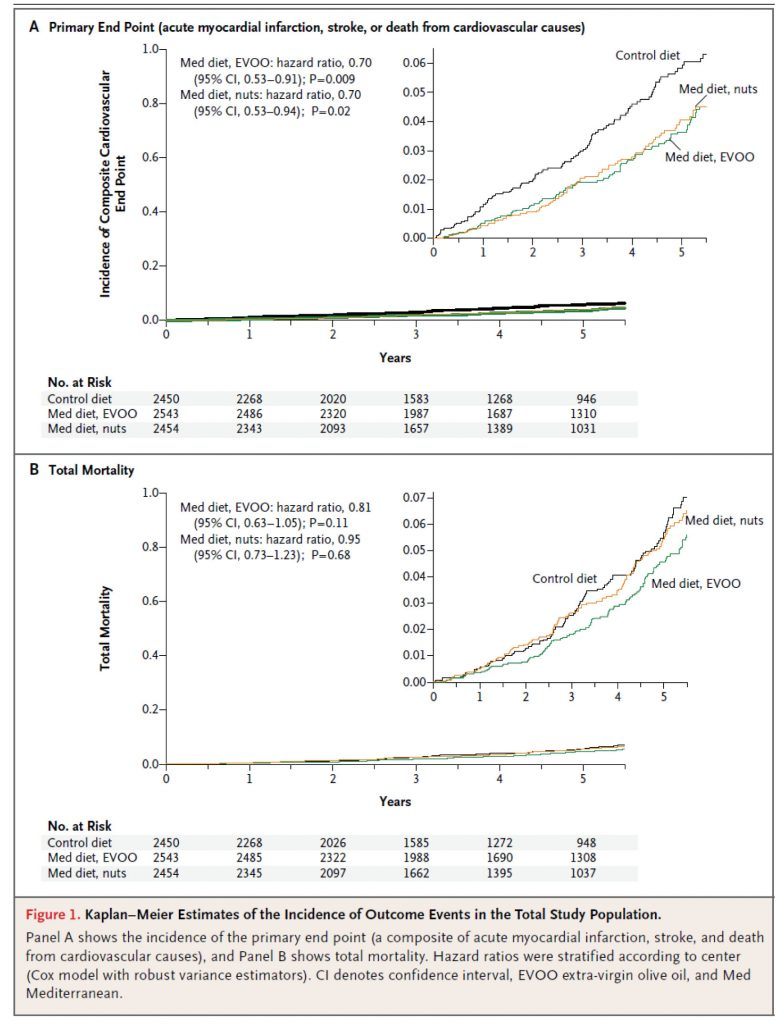
Figure 1, below, shows the Kaplan-Meier estimates for the primary end point (A) and total mortality (B). Each figure shows both the full y-axis (which always varies from 0 to 1) and, in the upper right corner, a zoomed view to show the difference. The fact that the zoom view is necessary tells you something about the absolute risk reduction. It’s small.
Here’s a quick calculator to determine the absolute risk reduction (ARR). When you plug the numbers in from this study (I’ll just do it for the low-fat vs. EVOO group), you’ll see the ARR is 0.3065%. The reciprocal of this number is 1/0.003065 = 326. This is called the number needed to treat (NNT). This means that 326 people would need to undergo this dietary intervention for about 4 or 5 years to prevent one “count” of the primary outcome.
Is this important? Or, to be more specific, is this “clinically significant” as I asked earlier? Well, it depends on the intervention. If this study were testing a drug with a 1% major toxicity rate, the answer would be emphatically, no. Obviously, we could not justify treating 326 people to save 1, if 3.26 people (on average) will experience a major toxicity!
Conversely, if this study were testing a drug with a 1% minor toxicity rate (e.g., headache) and a 0.001% major toxicity rate (e.g., kidney failure), the answer is not so clear. For perspective, most drugs fall into this second category (e.g., statins, aspirin).
I could go through the exact same argument using Quality-Adjusted Life Year (QALY) instead of toxicity. While this approach is not used in the United States (perhaps it should be), it is certainly the cornerstone of other healthcare systems, such as the NHS in the United Kingdom.
While it’s beyond the scope of what I wanted to write about today, the key to sorting through this grey zone is better defining patient susceptibility and outcomes in large clinical trials. For example, I would argue that the data on statins could be much better if the treatment target was LDL-P or apoB instead of LDL-C, especially in high risk patients with metabolic syndrome, at least half of whom have discordant LDL-P and LDL-C.
So, what to make of the modest ARR in this study? Well, question 1 should be: what is the toxicity of a Mediterranean Diet? Question 2 should be: what is the QALY impact of a Mediterranean Diet?
I can’t really answer either of these questions. The former is objective but has not been quantified to my knowledge. The latter is subjective, and each person needs to answer it for themselves.
My conclusions
Overall, I think this is a good study, and a better study than the study prompting it, the famous Lyon Heart Study. That said, I would have much preferred to see only one Mediterranean arm (in retrospect this is obvious, of course, given the lack of difference between them), in favor of a true control or another arm such as Very Low Carb.
It’s impossible to guess what the ARR would have been for the Med Diet if the control was a standard fare diet (complete with 138 gm per day of sugar!), rather than a much improved low fat diet. If I had to guess, I’d ballpark the ARR at 1-5%, for a NNT of 20 to 100 people, but this is nothing more than speculation. Remember, I think the Low Fat arm in this study experienced an enormous benefit over their baseline.
In the coming months and years, as NuSI begins funding remarkable clinical trials, we’ll have plenty more to discuss…
Photo by Carlos Santiago on Unsplash




I have proved to myself that it is possible to do a low-carb vegan lifestyle. Interesting serum chemistry results – the best total:HDL ratio I’ve ever achieved, best hsCRP ever, best trigs ever, and weight and BP continue to drop through the floor, nicely. It is possible to minimize cholesterol intake, saturated fat and carbohydrates. If it’s of any value, here is what I eat.
Breakfast:
-bowl of low carb organic low fat yogurt with 7 types of nuts and seeds (hazelnut, almond, brazil, walnut, pecan, sunflower, pumpkin seed)
-2 avocados
-15 lupin beans
-1 tablespoon of macadamia nut butter
-1 glass of water
(I stopped drinking coffee or tea entirely.)
Lunch (5-6 hours later):
-Israeli salad with fine-chopped tomatoes, cucumbers, green onions, radishes, green pepper.
drenched in tahini whipped 50:50 with lemon juice and spices.
-2 tofu sausages on the side, dipped in honey mustard aioli dressing (low carb).
-1 glass of water
Dinner (6 hours later):
-2 low carb fajitas made with seasoned tofu, sauteed broccoli, red onion, mushrooms, orange pepper, high protein greek yogurt (18 g per 175 cc), 4 drops of mexican hot sauce, toasted.
the seasoning consists of cumin, pepper, salt, smoked paprika, chili powder, garlic powder.
-1 glass of water
Snack (at night)
-nuts or olives or lupin beans or an avocado
I’ve stopped my statin, don’t worry about salt intake, but make a concerted effort to avoid acellular carbohydrates, as you can see from the above.
Peter – thanks for responding to my inquiries, I’m really trying to figure this out so I can give my patients the best care. I wonder if you can comment on significant discrepancies between our local lab and the Liposcience NMR results – I have had a couple of patients where the results are significant, but most recently a gentleman who had his lipid panel and his lipoprofile tested within 3 days of each other, but the total cholesterol was 247 at our lab and 197 at liposcience, and his LDL was 170 at our lab and 137 at liposcience; I had one other patient who had them drawn at the same time and the LDL was 30 points different – I am feeling very insecure about one test or the other if there is this kind of discrepancy (not the only times I’ve seen it, but in most of the other patients I have had a 3 month difference and thought their labs came down significantly with LC eating). Thanks – Jenn Lentz
Not my area of expertise.
Jenn Lutz, was he fasting in one lab and postprandial in another? More likely, you are comparing direct and calculated LDL – they will be very different, as calculated LDL is based on a number of assumptions, which for the typically American is usually incorrect. For example, a triglyceride count that is either too low or too high will throw off a Friedwald-calculated LDL quite grossly.
I had both NMR and VAP Profile, same day, with different results.
TG had delta of 30 pts
TC had delta of 20+
I don’t know what to make of it.
VAP Profile
TC 315
HDL 67
Tris 103
LDL 220
LP(a) 7.0
Sub-class:
LDL1-Pattern A 49.8
LDL2-Pattern A 67.5
LDL3-Pattern B 60.5
LDL4-Pattern B 0.0 (good?)
NMR Profile
TC 292
HDL 69
Tris 71 (way off from VAP PROFILE)
LDL-C 209
Small LDL-P 711 (good or bad?)
LP-IR Score: 10
LDL size 21.3 nm
Dan – thanks. No, he was fasting for each. I was figuring that the NMR would be more accurate just because it is measured as opposed to calculated, and so I am going with that number. I just was very surprised by the huge discrepancy. Thanks.
I recall Lyle Mcdonald mentioning that those pre-disposed to depression would have a difficult time psychologically with a low carb diet. I believe he related this to protein precursors to serotonin and dopamine and insulin but I’m not sure. Any thoughts?
Would need to see data to comment, though it seems that would be more an issue with protein restriction than carbohydrate restriction.
Peter, my company partners with the Mayo Clinic for employee health. I got a “personal” reminder today as I take medication for high blood pressure. There were 10 bullet points, and some of them were sensible (lose weight, exercise, reduce alcohol consumption). The ones that stuck out to me were items 3 & 4 (shown below).
3. Eat a healthy diet
Eating a diet that is rich in whole grains, fruits, vegetables and low-fat dairy products and skimps on saturated fat and cholesterol can lower your blood pressure by up to 14 mm Hg. This eating plan is known as the Dietary Approaches to Stop Hypertension (DASH) diet.
It isn’t easy to change your eating habits, but with these tips, you can adopt a healthy diet:
Keep a food diary. Writing down what you eat, even for just a week, can shed surprising light on your true eating habits. Monitor what you eat, how much, when and why.
Consider boosting potassium. Potassium can lessen the effects of sodium on blood pressure. The best source of potassium is food, such as fruits and vegetables, rather than supplements. Talk to your doctor about the potassium level that’s best for you.
Be a smart shopper. Make a shopping list before heading to the supermarket to avoid picking up junk food. Read food labels when you shop and stick to your healthy-eating plan when you’re dining out, too.
Cut yourself some slack. Although the DASH diet is a lifelong eating guide, it doesn’t mean you have to cut out all of the foods you love. It’s OK to treat yourself occasionally to foods you wouldn’t find on a DASH diet menu, such as a candy bar or mashed potatoes with gravy.
4. Reduce sodium in your diet
Even a small reduction in the sodium in your diet can reduce blood pressure by 2 to 8 mm Hg. The recommendations for reducing sodium are:
Limit sodium to 2,300 milligrams (mg) a day or less.
A lower sodium level — 1,500 mg a day or less — is appropriate for people 51 years of age or older, and individuals of any age who are African-American or who have high blood pressure, diabetes or chronic kidney disease.
To decrease sodium in your diet, consider these tips:
Track how much salt is in your diet. Keep a food diary to estimate how much sodium is in what you eat and drink each day.
Read food labels. If possible, choose low-sodium alternatives of the foods and beverages you normally buy.
Eat fewer processed foods. Potato chips, frozen dinners, bacon and processed lunch meats are high in sodium.
Don’t add salt. Just 1 level teaspoon of salt has 2,300 mg of sodium. Use herbs or spices, rather than salt, to add more flavor to your foods.
Ease into it. If you don’t feel like you can drastically reduce the sodium in your diet suddenly, cut back gradually. Your palate will adjust over time.
I think I remember you’ve commented on the DASH diet trials in the past, but I really doubt that eating low fat, whole grain diet would reduce your BP by 14mmHg.
Similarly, they flog Salt – apparently they haven’t read Gary Taubes article on the Political Science of Salt. I would the Mayo clinic would think for themselves and not just pass along the same old foolishness spouted by the Medical establishment.
Thanks,
Dave
Oh boy…
Hi Pete,
Thanks heaps for your really informative articles. I just have a quick question regarding your thoughts on my own diet that is fairly balanced in terms of macronutrients, but probably with a larger proportion of fats (particularly saturated fats from coconut oil, whole milk, eggs, grass-fed butter). I was wondering whether eating relatively high amounts of saturated fats with moderate-high amounts of carbs (~300g/day) is detrimental to my heart health and arteries. I am a pretty skinny distance runner (64kg, 175cm, 18 y.o) so eat quite a few starchy carbs (sweet potato, white rice, oats) around workouts, even though i’d like to experiment with ketosis when I move out of home. I occasionally eat processed meat as well that my family cooks, begrudgingly as to not receive criticism. If i’m to maintain this balanced diet that include more carbs than is necessary (I’m scared ketosis would decrease my weight too much) am I better off excluding saturated fats and rather emphasise monounsaturated fats? I feel confused as to the real dietary determinants of cardiovascular disease are.
Thanks again,
kind regards,
Jonny.
Jonny, I can’t really comment on your diet. If you do experiment with NK, though, be sure to do it “right” and give it enough time to allow your body to adapt. In my experience this takes anywhere from 2 weeks to 2 years, with a median of about 3 months.
Hi Peter,
I really appreciate your blog and your quest to help us all think more critically about nutritional information. NK has been a blessing for me and I am trying to flesh out my understanding of it by reading many of these studies. Perhaps I am even getting to the point where I am biased in picking out the studies that support HFLC, so I’ve tried to diversify my reading, hence the questions I have on this study. (Sidenote: I have also been trying to figure out if there is any good evidence to support the whole 1:1 ratio of omega 3s to omega 6s. I saw this on your upcoming posts and look forward to your thoughts as I’m not having much luck reaching a solid conclusion other than to be sure to include DHA and EPA supplements.) Anyway, I recently came across this NIH study on Alzheimer’s and a diet high in omega-3s vs omega-6s (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3029147/pdf/nihms262591.pdf) and was thinking that diets high in omega-6s are likely also high in glucose, so why did the authors single out red meat and dairy so much? Any thoughts on the validity of this conclusion? They say they created a diet profile for each participant but only discuss the Med diet in much detail and classify the other diet as high in red meat, butter, and high-fat dairy. So… both diets are high in fat, omega 3s are obviously good and protective against AD (though apparently also needs to be low in omega 6s as well) but a diet high in omega 6s (and low in omega 3s) may possibly lead to AD?
Caitlin
At some point the “scientific” community needs to stop publishing this type of absolute nonsense. This was not an experiment. There was no intervention. I have neither the time, nor emotional energy to explain how scientifically corrupt this work is, other than to point you in the direction of my previous post on the supposed harm of red meat. Please give it a read. The higher consumption of meat and fat is almost surely a proxy for what is really driving the risk of AD.
It’s shortcomings are more obvious to me now and it frustrates me. I think that studies like this are some of the most harmful to the NK argument, not because they have validity but because they have authority. People trust their doctors (and big institutions like Harvard and NIH) not because they are ignorant but because they understand the limits of their own time, training, and knowledge. Even though diet seems like the root of so many medical problems, it’s going to be challenging to turn the tides on our national health crisis without getting these authorities (for better or worse) on board. For me personally, NK is an obvious choice rooted in sound science. But, for example, when I talked to my doctor about it, she seemed a bit skeptical but gave me the green light based on my youth, healthy weight, and high HDL (I also had low B-12 levels from following a so-called healthy, low fat diet.) I think she’s a very sharp doc and would not discard sound evidence, but I feel a bit silly trying to “teach” someone who is really supposed to be the authority on my health. I couldn’t help thinking what she might have said to another patient though. I hope that you and NuSi can fill this authoritative void. Best wishes, Caitlin
Thanks, Caitlin. You’re clearly a quick study on the issues we’re up against. I sometimes wish I knew none of this and lived in ignorant bliss. Kind of like the Matrix…
The knowledge is both a blessing and a burden for sure. If only we could take all that money we spend on treating preventable metabolic diseases and use it on schools and education, what a different world this would be! Keep thinking about all the good your work brings (and can bring on the future) and also how much cooler Neo is than the ignorant dystopians… 🙂
That’s true. I guess we need to feel more Neo-like. I just wish I looked like Neo, at least!
Thanks so much for your article… I’m looking at this journal article and am new to statistics, so it’s helped immensely. However, could you explain what you mean here?
“Remember that pesky little statistical thing called power. This study was powered (at 80%) to detect a difference in the primary outcome, which it showed. In fact, the intention-to-treat was greater than 7,500 because the authors expected no more than a 20% relative risk reduction. But they saw a 30% difference, and the study was halted early.”
There’s a lot there, so I’m not sure of your question. You can find great examples of statistical power on line. Hopefully that helps. I’ve also defined it in previous posts.
I’m not a scientist or a doctor. In fact, I’m a stay-at-home mother. Nutrition and food is something of a layperson’s obsession for me, and fresh food shopping and cooking from scratch daily take up an inordinate amount of my time. I have long had the nagging question in my mind about the effects of preservatives and additives in food. I think that, individually, the preservatives in food may not be harmful, per se. But, taken together in the quantities that most people/families consume processed food (precisely for the lack of inordinate time!), I wonder how these chemicals affect hormones and other functions in the body and their knock-on influence on obesity. The example of BPA leaps to mind. How much is too much when it comes to these chemical additives and what degrees of harm do they provoke? How does the body process this stuff? How are the liver, kidneys, brain, pancreas, and immune system affected? A can lined with BPA plastic filled with sodium- and preservative-laden green beans is not the healthy option it appears to be. Multiply this intake by the number of meals in a day, week, month, or year and we may see shocking amounts of “invisible” chemicals. By extension, pesticides and other chemicals in the food system and how they affect the body and obesity should be investigated. GMO food? Fast food could be a complete study on its own. There seems to be less and less food in food. Perhaps the food itself is not the only problem. The coincidence of our “modern” diet and the obesity trend should not be overlooked. We seem to have very little control over what is sold to us in supermarkets and in restaurants and it seems that every component of a meal at home comes from a jar, can, or box –which means lots of additives. What do you think of this? (Forgive me if you covered this topic elsewhere in your blog, I’m new to this one. Just point me in the right direction.)
Dr. Attia,
I’m interested in the recommendation in many (relatively) northern countries like Canada to take supplemental vitamin D. I wondered how humans in northern climates received vitamin D prior to supplements being available.
Looking at foods naturally high in vitamin D it’s apparent that fatty meats and fish contain huge amounts. This makes sense as it’s a fat soluble vitamin.
Is it fair to hypothesize that part of the widespread Hypovitaminosis D is partly due to the current fat paranoia that we seem to have? By my math, even a diet with 30-40% of calories from fat, including fish, is likely to provide plenty of vitamin D, whereas the a diet following the LEARN recommendations would not.
I think we’re still working on developing a better understanding of where optimal vit D levels should be and by extension how much, if at all, folks should supplement. May be an inverted U effect–in fact, almost assuredly is–the question is where the curve lies.
I agree with your statement, I have read one more blog that also clearly indicate that Mediterranean diet preventing cancer.
You mention “So, I choose to still consume bacon, because I believe, on average, and in most populations, bacon consumption is merely a marker for bad eating habits.”
Surely you are not worried about the high fat there, so far we agree. I wondered if you go out of your way to find nitrite- and nitrate-free bacon.
If not, is it because the amounts are small enough not to worry or is it because you don’t believe that nitrite and nitrate are as evil as advertised (that is, that the studies that “proved” this are weak)?
I’m still waiting for one nitrate study to convince me they are harmful in the quantities most people consume them.
Hello.
My wife Sarah is following this diet. She says she feels a lot better already, and she has been following it for only 30 days. She loves the Mediterranean diet food and she actually enjoys being on this diet.
She decided to start following it after reading ebook “Mediterranean diet weight loss results” on Amazon.
Here is her meal plan:
On Mondays she eats Greek yogurt with strawberries and oats for breakfast.
For lunch, she usually has whole grain sandwich with vegetables.
And when it comes to dinner, she often makes tuna salad; dressed in olive oil (she loves it). It’s really delicious.
For a dessert she is allowed to take a piece of fruit.
I would like to bring your attention to the endogenous PPAR-alpha agonist- OEA (Oleoylethanolamide) which is implicated in weight loss in obese rats & other experimental animals. (PPAR-Alpha is the target receptor to treat hypercholesterolemia). RiduZone (www.riduzone.com) is the only FDA acknowledged supplement in the market which supplements OEA adequately & results in healthy weight loss.
Thanks!
If you’re wife is anything like mine, she would have told your daughter “Honey, your Daddy is already a nutcake!”.