Check out more content with neurologist, Richard Isaacson, M.D.:
Peter is joined by writer, director, actress, and founder of HFC, Lauren Miller Rogen, and previous podcast guest and director of the Alzheimer’s Prevention Clinic at Weill Cornell Medicine and New York-Presbyterian, Dr. Richard Isaacson. In this episode, Lauren tells the heartbreaking story of watching members of her family succumb to Alzheimer’s disease (AD) which motivated her to proactively address her own risk with Richard’s guidance. Richard discusses the various genetic and lifestyle factors that influence the risk of AD and uses Lauren’s unique situation to explain how he diagnoses patients and personalizes care. They go through Lauren’s protocol of preventative measures that have already produced marked results, and end with the uplifting message that one’s genetic predisposition does not seal one’s fate.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER
We discuss:
- Lauren’s deep family history of Alzheimer’s disease (3:10);
- The influence of genetics, epigenetics, and lifestyle on Alzheimer’s disease risk (13:45);
- Lauren’s mother’s disease progression and the enormous stress it causes for family members (24:30);
- The various manifestations of Alzheimer’s disease depending on the location of pathology (29:30);
- The three stages of Alzheimer’s disease (34:45);
- Richard’s deep exploration into Lauren’s family history revealing clues about a diagnosis and a roadmap to successful disease mitigation (39:15);
- How exercise reduces Alzheimer’s disease risk, and the different risk between males and females (58:00);
- Why knowing your APOE status is important, and whether certain people should be wearier of head trauma (1:08:00);
- How Richard uses genetic testing to personalize care (1:14:45);
- The “ABCs” of Alzheimer’s prevention, lifestyle interventions, and Lauren’s personal protocol for reducing her risk (1:21:45);
- Unique treatment for people with the ApoE4 variant (1:36:30);
- Richard’s mixed opinion on CBD and THC as a tool for disease prevention (1:40:00);
- Cognitive testing procedures, and how Lauren’s tests furthered her commitment to her disease prevention protocol (1:41:45);
- The relevance of sense of smell and hearing in Alzheimer’s disease risk and prevention (1:50:00);
- The emotional benefit of knowing you have control over your mental and physical health (1:57:30);
- HFC—a charitable organization founded by Lauren and Seth (2:00:15); and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Lauren’s deep family history of Alzheimer’s disease [3:10]
Family history of Alzheimer’s disease
- Her maternal grandfather had Alzheimer’s disease (AD), started showing symptoms in his late fifties/early sixties and was put into a nursing home when Lauren was 9 or 10
- After Lauren’s grandfather passed away, her grandmother began showing symptoms of AD and she also ended up in a nursing home and died in her mid 70s
Losing her mother to Alzheimer’s disease
- At the time of Lauren’s college graduation, she noticed her mother (just 52 years old) repeating stories—something that really worried Lauren
- Within a year or two, she was losing her ability carry out her job as a teacher and function as a cognitively healthy person would
- At this point, they brought her to a doctor and Lauren’s mother was given “as much as a diagnosis as one could get at that time”
- At this point, it was clear there was something going on in the family with AD
- Lauren was confronted with a difficult mix of emotions, including fear, anger, depression, and denial (Lauren said her father was in the most denial)
- In 2005, Lauren finally admitted out loud that her mom was suffering from AD
“Who she was, was just fading away and changing right in front of her eyes.” —Lauren Miller Rogen
- After another couple of years,
- it was clear that Lauren’s mother should not be driving or be teaching in a traditional classroom
- She was also unable to carry out long conversations
- This was devastating for Lauren and was a dark time for her
- What scared her mother the most about having AD: “And she told me that she wasn’t scared for her. She was scared for me and my brother and my dad, because I think she got that at some point she may not know what’s happening, and that the weight would be on us.”
- Devastating consequences:
- At this point, Lauren was a young adult and just beginning to interact with her mother as a friend more so than a mom
- Being deprived of the opportunity to develop this friendship with her mother was very difficult for Lauren
- Lauren was intent on finding a way to help her mother, but despite her best efforts, she found nothing
“There was nothing. And so it was a really scary, hard time where I felt like I could do nothing and that this train had left the station for my mom and that was it.” —Lauren Miller Rogen
The influence of genetics, epigenetics, and lifestyle on Alzheimer’s disease risk [13:45]
Richard’s perspective on Alzheimer’s disease
- Richard sees it as an insidious disease – he “hates” it because it not only robs the person with it of who they are, but also robs the entire family
- Alzheimer’s begins in the brain about a decade before the first symptoms of memory loss, and this is something many doctors are still unaware of
- Onset of Alzheimer’s symptoms usually occurs in one’s seventies, but with early-onset Alzheimer’s disease, symptoms can begin in one’s forties or fifties
- While genetics is often responsible for an early onset of Alzheimer’s disease, Richard points out that there are cases when there is more to the story that can cause an earlier onset (lifestyle, head trauma, comorbidities, etc.)
- Richard suspects this might be the case with Lauren’s family – “there’s a one plus one equals three here”
“… could it be lifestyle? Could it be an exposure to something? Could it be head trauma? Could it be uncontrolled diabetes, high blood pressure, cholesterol? These are all things that just synergize together to potentially make a late onset Alzheimer’s case start earlier.” —Richard Isaacson
Genetic risk factors for early-onset Alzheimer’s disease
- Genes known to cause early-onset Alzheimer’s disease: Variations in the genes for presenilin-1, presenilin-2, and amyloid precursor protein gene mutation
- These variations are quite rare (far less than 1% of people):
- Richard has only had a few patients (out of more than 1,500) that have had one of these variations
- Peter has never had a patient with one of them
- These variations are quite rare (far less than 1% of people):
Genetic and epigenetic causes pushing onset of AD earlier in life
Most people that get AD earlier in life don’t have “early-onset Alzheimer’s disease” but rather they have a “milieu of things” aka polygenic risk and epigenetics that simply push the onset of AD earlier in life
- For example, the apolipoprotein E (ApoE) gene variants
- The E4 variant raises AD risk
- In contrast, the E2 variant is protective and the E3 variant, which is most common, is neutral
- Lifestyle and behavioral characteristics
- Diet
- Exercise
- Head trauma
- Comorbidities (e.g., diabetes, high blood pressure, cholesterol)
“Genes are not our destiny. We can absolutely win the tug of war against our genes.” —Richard Isaacson
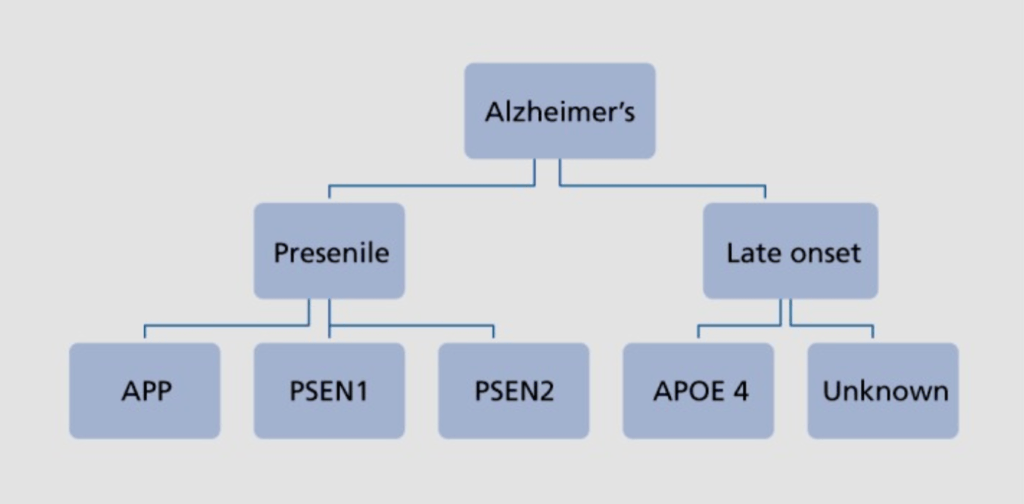
Figure 1. Genetic influence on early and late Alzheimer’s disease risk. Image credit: ncbi.nlm.nih.gov
The future of Alzheimer’s disease prevention and treatment:
- And there are usually multiple genes involved, which is why Richard believes that the future of Alzheimer’s prevention will be based on precision medicine
- Using these types of genetic underpinnings, understanding all the individual genes that impact a person’s risk, figuring out what they are, figuring out what their biological function is, figuring out why it puts a person down the path towards Alzheimer’s and then telling that person to do A, B, C, X, Y, and Z to get them off the path towards Alzheimer’s
What is it about APOE4 that confers more risk for AD?
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.