Note to readers: This post was written in December of 2011. PLEASE do not ask me why I eat ‘this’ or why I don’t eat ‘that’ — as what is shown here does not necessarily reflect what or how I eat today (or more importantly, how you should eat). My diet evolves constantly, due to my constant tweaking and self-experimentation. Over time, I’ll share it here and there, but what I eat is not at all the focus of this blog. I ask that you refrains for pursuing questions about what I eat in the comment section.
Once people start to “get it” with respect to why carbohydrate reduction, or all-out restriction, leads to good things, the inevitable question I’m asked is, “So….what exactly do you eat?” I’m always a bit hesitant to get into this. It’s sort of like asking a pilot, “So…how do you fly this plane?” It’s a great question, but probably the wrong first question.
For many people it’s so overwhelming to contrast what they currently eat – probably a typical American diet of 500-600 daily grams of carbohydrates (200 grams of which are sugar) – with a diet of less than 50 daily grams of carbohydrate, which is what I consume. Remember, what I’m showing you here is what I have been eating for about the last 7 months. For the first 20 months of my nutritional transformation, I was gradually reducing carbohydrate intake from about 600 daily grams to 300 daily grams to 150 daily grams.
It’s really important to understand that carbohydrate reduction is a continuum. There is no “right” amount of carbohydrate to eat. Let me illustrate this with the following “2 by 2” matrix, below (sorry, once a consultant, always a consultant). When asking the question, “How much should I reduce my intake of carbohydrates?” it’s a good idea to start with two broader questions:
- What is my inherent level of insulin resistance?
- What are my goals?
There are technical ways to quantify the answer to the first question, which I will detail in future posts. However, the simple version of determining your inherent amount of insulin resistance is checking how many criteria of metabolic syndrome are present. In other words, are you overweight? Is your waist large? Is your blood pressure high? Do you have elevated blood glucose or triglycerides (these are determined from a standard blood test)? Do you have low HDL cholesterol? For the purpose of this question, even responding “yes” to one of these questions means you are predisposed to being insulin resistant. I was a “yes” to 3 of these questions.
Consider this matrix, and let’s use me as an example.
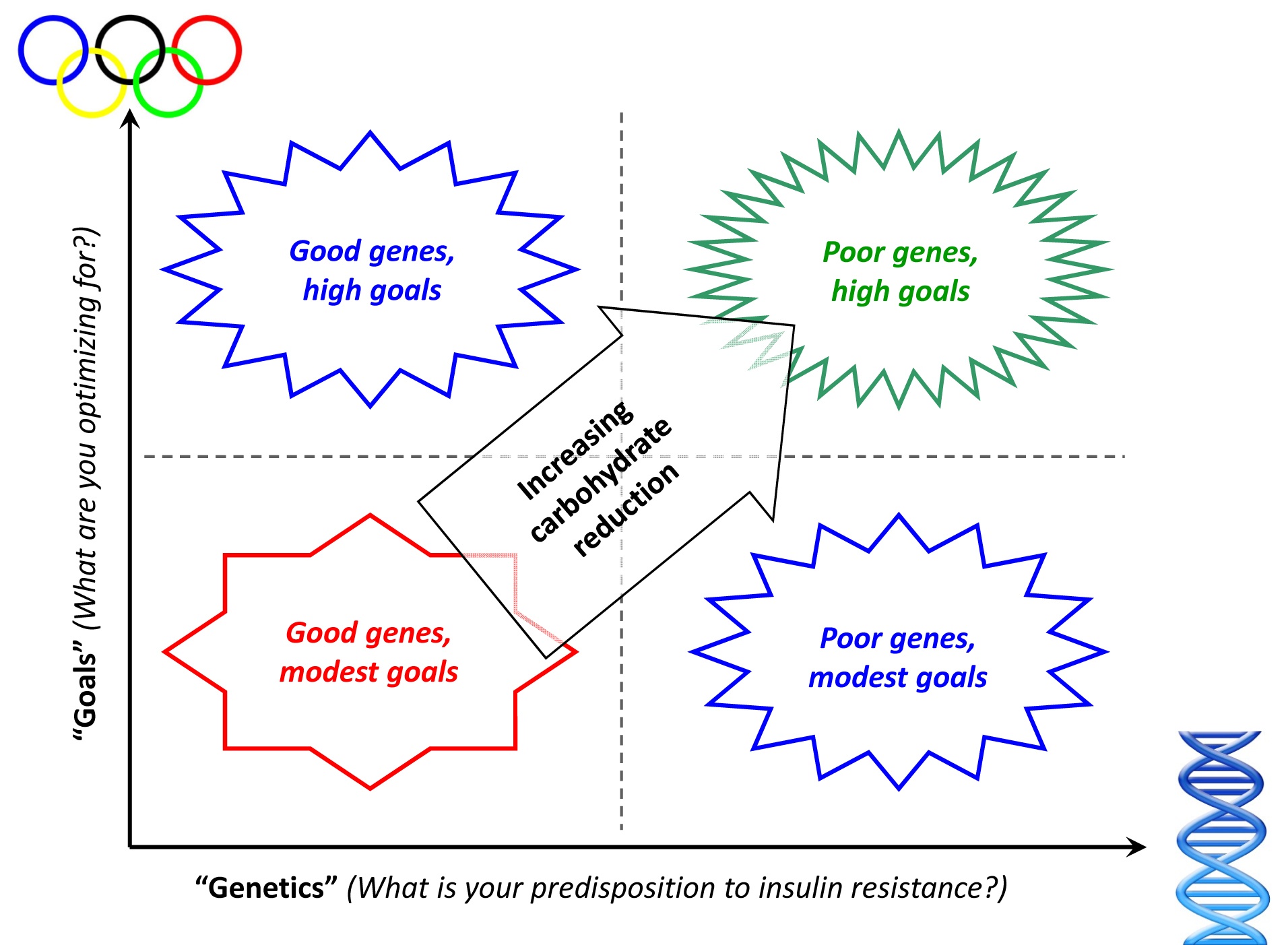
- How predisposed am I to insulin resistance? One look at a picture of me in my non-lean state, coupled with an understanding of my family history, and it’s clear I didn’t hit the genetic lottery with respect to insulin resistance. Hence, I am towards the right of graph.
- What am I optimizing for? Some folks want to lose 15 pounds. Others want to have fewer swings in daily energy level, or stop taking their blood pressure medicine. In my case, I want to maximize as many variables as possible: I want to be as lean as I can; I want to cure my insulin resistance; I want to be sure I never have a single symptom of metabolic syndrome; I want to do everything I can to avoid cancer and Alzheimer’s disease; I want to be metabolically flexible. Hence, I am towards the top of the graph.
As you can see, based on my poor genes and lofty goals, I find myself in the upper right square, which means I need to adopt the greatest amount of carbohydrate restriction. My wife, in contrast, has good genes, coupled with high goals, placing her in the upper left box. As a result of this combination, she does not need to restrict carbs as much as I do. If her goals were even more modest, she could get away with very little reduction in carbohydrates – probably just reducing sugar without much reduction in starch.
Below is a picture of a few of the foods you’ll typically find in my refrigerator. Note that on average I consume about 4,000 to 4,500 calories per day. I get this from approximately 400-425 grams of fat, 120-140 grams of protein, and 30-50 grams of carbs. In addition, there are a number of supplements I consume daily, which I describe in the table below. In future blog posts I will go into greater detail as to why I consume each of these supplements, but for now I’ll give a very quick explanation.
Finally, note that under no circumstance do I ever count calories (for the sake of limiting them). When I was first transitioning into ketosis I did need to count how much carbohydrate and protein I was consuming – anything over about 50 grams of carbs and 150 grams of protein makes it difficult to generate sufficient ketones – but I do not ever count calories for the sake of restricting them. I eat when I’m hungry. I don’t eat when I’m not hungry.

Regular supplements I consume every day
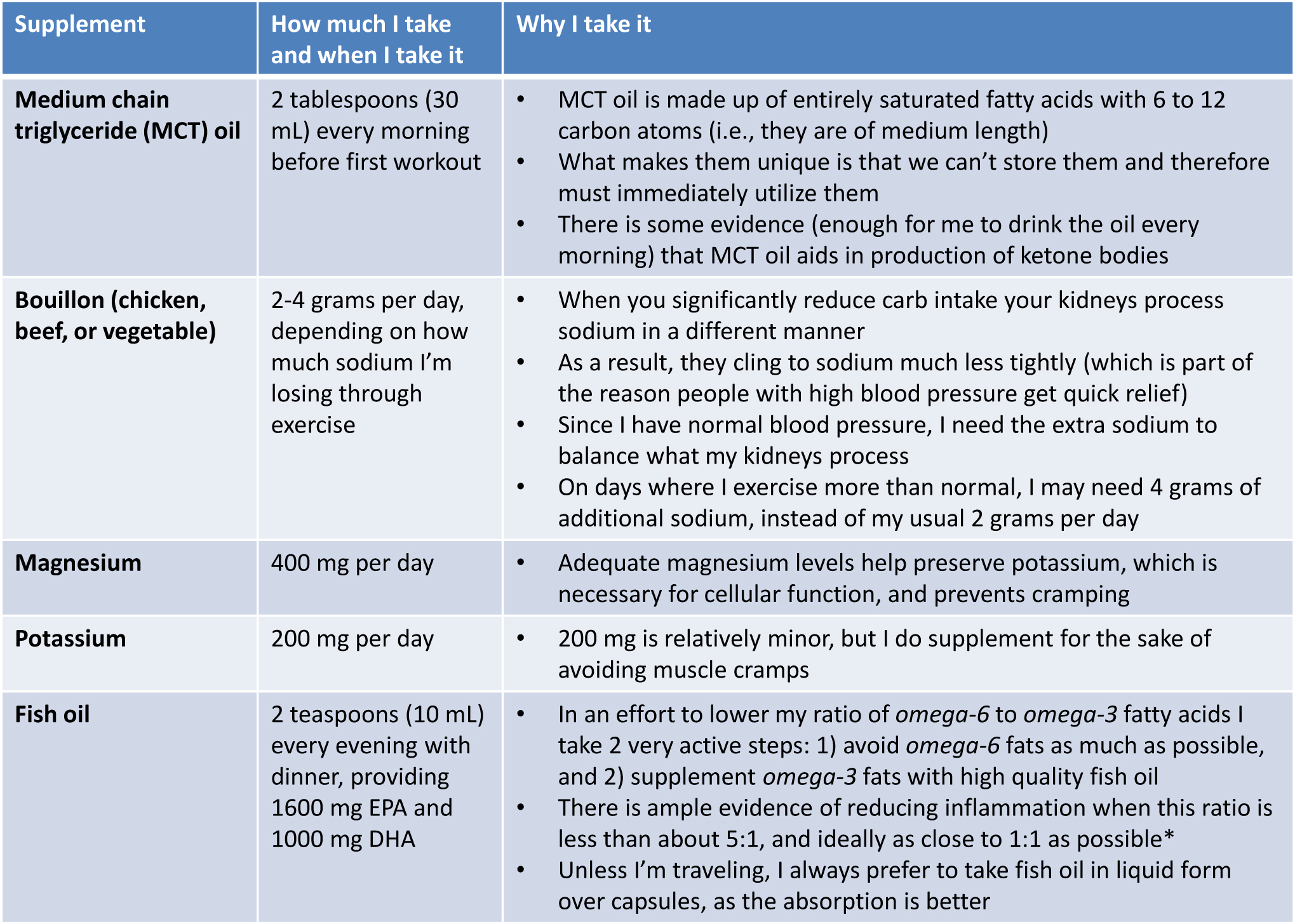
*I will be writing a great deal about the role of omega-6 and omega-3 fatty acids in our diet in subsequent posts. However, if you want a quick (albeit high-level and not overly nuanced) overview of the topic, take a look at what Dr. Andrew Weil and Livestrong have to say about it.
One last point on supplements – I do not take a multivitamin at this time, but I am looking into it a bit more closely. My concern is that 1) they may not be necessary when you remove glucose from your diet (I’ll write about why in the future), and 2) they may actually do direct harm, as a result of contaminants.
Ok, at long last, here is a list of what I ate over the past 5 days (excluding water, still and sparkling, which I consume about a gallon of each day)
Wednesday
Breakfast: “Fat shake” (In a blender: 8 oz heavy whipping cream, 8 oz sugar-free almond milk; 25 gm sugar-free hydrolyzed whey protein, 2-3 frozen strawberries)
Lunch: About 4 or 5 oz of assorted cheese (Gouda, Swiss, Manchego), 2 or 3 oz olives, about 4 oz of particularly fat salami and pepperoni
Late afternoon: About 2 oz of mixed nuts (almonds, walnuts, peanuts), large latte (latte made with heavy fat cream instead of milk) at Peet’s
Dinner: Garden salad with olive oil (lots of extra oil) and balsamic vinegar dressing, about 6 oz grilled salmon with a lot of butter and lemon juice
Thursday
Breakfast: Scrambled eggs (6 yolks, 3 whites**, with added heavy fat cream) cooked in coconut oil, 3 or 4 sausage patties (be sure to look for brands not cured in sugar).
Coffee with homemade whip cream (heavy fat cream hand whipped)
Lunch: Half chicken (thigh, breast, wings) with lots of skin; about 2 oz of Gouda and aged-cheddar
Dinner: Wedge blue cheese salad with bacon; 12 oz prime rib with lots of butter; 5 or 6 pieces of asparagus coated in butter
Coffee with half and half cream, 2 cups (the restaurant did not have heavy cream, so I had to settle for half-and-half)
**The reason I typically minimize egg whites, at least when making my own eggs, is to ensure I keep protein intake under about 125 grams per day. Ketosis is pretty easy to attain if one is eating, say, 2500 calories per day. However, given my caloric demands – and the requirement that I keep protein intake limited – I really need to go out of my way to ensure I’m not eating too much protein. I will be writing about this in much greater detail in a future post.
Friday
Breakfast: Whole fat latte at Starbucks (made same as above), scrambled eggs (about 4 eggs), bacon (high fat pieces), slice of Swiss and slice of cheddar (since I was eating in the airport, the scrambled eggs were made “normally,” not with the additional fat I use when making my own)
Lunch: About 4 oz of especially fat salami and pepperoni, about 2 oz Parmesan cheese
Dinner: Ground beef sautéed with heavy cream, onions, broccoli, and melted cheese
2 large cups of decaf coffee with homemade whip cream (heavy cream whipped with a touch of xylitol)
Saturday
Breakfast: Scrambled eggs (6 yolks, 3 whites, with added heavy fat cream) cooked in coconut oil, 3 or 4 pieces of especially fat bacon (not cured in sugar), about 3 oz of cream cheese
2 cups of coffee with heavy cream
Lunch: Tomatoes with basil and mozzarella and balsamic vinegar and olive oil, about 2 oz raspberries with homemade whip cream
Dinner: Leftover ground beef sautéed from previous night, salad with homemade cream dressing (whole fat Greek yogurt, olive oil, basil, blue cheese, garlic)
1 cup of decaf coffee with homemade whip cream
Sunday
Breakfast: Omelet (6 yolks, 3 whites, coconut milk, sautéed onions) cooked in coconut oil, 4 or 5 pieces of the fattest bacon I can find
2 cups of coffee with heavy cream
Lunch: Plate of assorted cheeses (aged Gouda, Swiss loaf, aged Parmesan – about 3 oz), about 2 oz salami, about 1 oz olives
Dinner: Cream of mushroom bacon soup (heavy cream, chicken broth, shredded Parmesan cheese, mushrooms, chopped bacon, garlic, butter, chopped papers, various spices), leg of lamb (baked in sauce made of red wine, balsamic vinegar, diced tomatoes, garlic, and a lot of spices)
2 cups decaf coffee with homemade whip cream (as above)
So there you have it — 5 days in the eating life of Peter Attia. This may look a bit strange, relative to what you may be eating now, but remember, I’m at the far end of the spectrum – i.e., nutritional ketosis. You may just be starting your own journey of reducing carbohydrates, but I hope this gives you an idea of what I eat. In particular, what probably stands out is:
- I go to great lengths to avoid sugar which, unfortunately, shows up in virtually every highly processed food.
- I eat zero starch (e.g., bread, cereal, rice, crackers, pasta).
- I consume only modest amounts of fruit (one serving per day, at most, and only in the form of berries, which contain the least amount of fructose).
- I eat vegetables, but primarily because they are a great way to get more fat (e.g., high-fat salad dressings, butter), not because I “need” them.
- I go out of my way to eat as much fat as possible, especially monounsaturated and saturated fat (the only fat I avoid is omega-6 polyunsaturated fat).
- I have a few “go to” meals that I eat several times per week. I do this because I really like them and it’s quick and easy make them. Yours need not be the same!



