The notion that in some cases food can be a medicine rings true. For better or for worse, diet can change one’s physiology. One of the more popular diets today is the high-fat, very low-carbohydrate (typically between 20-50 grams) diet (VLCD), which we will also refer to as a ketogenic diet. In some, the ketogenic diet may help to ameliorate metabolic syndromes like obesity and type 2 diabetes, and positively affect problematic cardiometabolic markers. However, a recent paper published in the Journal of Clinical Lipidology highlights five cases in which patients had severe lipid perturbations while on the diet. Though these patients lost weight, they were found to have elevated total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C). These lipid perturbations were due to pre-existing conditions, some of which were identified in the paper, and the cases suggest that abnormal lipid responses to the ketogenic diet is driven, in part, by genetics.
About the Study
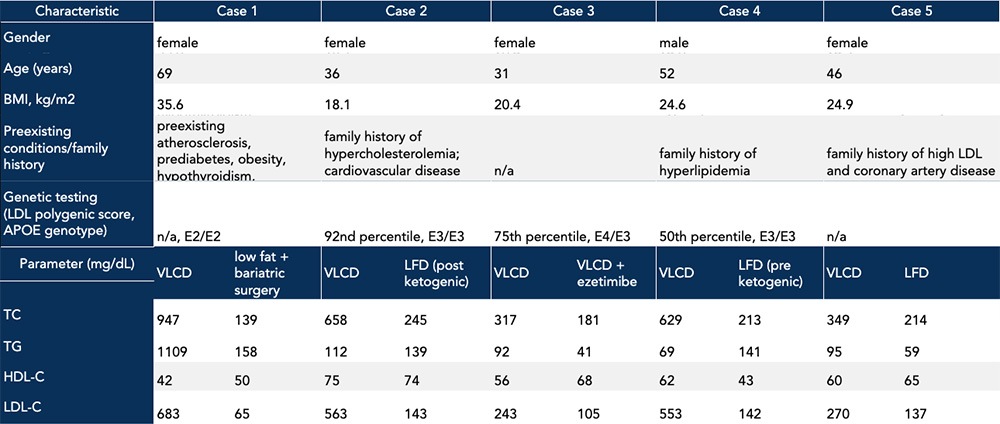
While it is not a revelation to say that genetic factors can influence one’s physiologic response to diet, the VLCD importantly did not cause aberrant baseline lipids in the instances under discussion. Rather, the diet may interact with intrinsic factors to exacerbate underlying conditions, which may or may not be known upon starting the diet. Some patients in the study had an identified family history of cardiovascular disease, and in all cases, subjects responded to the diet with elevated TC and LDL-C (Table). In one case, the patient had two copies of the apolipoprotein E2 gene variant, a variant associated with development of dysbetalipoproteinemia. This lipid disorder is characterized by the presence of atherogenic lipoprotein remnant particles, which are associated with significant elevations in triglycerides (TG) and calculated-LDL-C. In another case, the patient had familial hypercholesterolemia that contributed to the abnormal increase in TC and LDL-C observed in response to the ketogenic diet. Further, two of the study subjects had a family history of lipid abnormalities and atherosclerotic cardiovascular disease which might have explained, in part, the observed elevations in TC and LDL-C (Table). Although one out of these five total subjects did not report a pre-existing condition or family history of lipid abnormalities, the patient’s apoE genotype revealed a single copy of the apolipoprotein E4 allele, often correlated with the hyperabsorption of cholesterol. This association could explain the concomitant increase in TC, TG, and LDL-C on a ketogenic diet.
Table. Case study characteristics including family history and preexisting conditions, along with lipid panel results on a ketogenic diet vs an alternative diet or lipid-lowering treatment. Data adapted from Goldberg et al., 2021.
Why is elevated LDL-C a concern?
The case study report, among others, sounds the alarm because of the elevated baseline LDL-C. Elevated LDL-C is a concern for many because it is a measure of cardiovascular disease risk used in most health guidelines, including those by the American Heart Association. The logic goes like this: the LDL-C measure refers to how much cholesterol is carried in LDL particles, each of which also carries a single copy of apolipoprotein B (apoB). ApoB-containing lipoproteins transport cholesterol content into the arterial wall, which may cause plaque to develop. Given the one-to-one ratio of LDL and apoB, an apoB measure, compared to LDL-C, provides a more accurate measure of cardiovascular disease risk, though LDL-C and not apoB is often reported in studies. Some analyses suggest that a ketogenic diet compared to a low-fat diet reduces cardiovascular risk factors despite an increase in LDL-C. With that said, LDL-C remains the primary guideline target for lipid-lowering drug therapy and for dietary management as it pertains to atherosclerotic risk.
What information is missing from the study?
Though this case study reports personal and family medical history for each patient, as well as genotypes for relevant genes where available, the study might have benefited from more complete clinical profiles for each subject. First, although the paper refers to a ketogenic diet, the investigators did not take blood measurements confirming nutritional ketosis (characterized by beta-hydroxybutyrate levels between 0.4 and 0.6 mmol/L). The study also failed to include other useful markers that would have helped create a better clinical picture and better guide for individualized corrective action. For instance, in addition to lipoprotein burden, I evaluate cardiovascular risk based on measures of inflammation such as C-reactive protein, molecules such as uric acid and homocysteine that relate to endothelial function, and metabolic markers of insulin resistance/sensitivity and kidney function.
The case study report also does not mention evaluating markers of cholesterol synthesis. In some people, dietary saturated fat induces excess cholesterol synthesis and can also decrease the expression of LDL receptors in the liver, which impairs clearance cholesterol-carrying apoB particles from the plasma. Understanding the potential effect of dietary saturated fat on increasing circulating LDL particles can inform the decision to pursue a ketogenic diet. While there is no “real-world” measure for LDL receptor activity, cholesterol production can be measured by lathosterol and desmosterol, and if production is found to be elevated, statins can be used to inhibit cholesterol synthesis. In the cases I have seen where a ketogenic diet induces significant dyslipidemia, cholesterol synthetic markers have always been very elevated, suggesting that at least part of the problem is excess cholesterol synthesis, presumably in response to the high saturated fat burden. (And in a few of those cases, dyslipidemia was reversed when the fat content was changed from primarily saturated to primarily monounsaturated fat.)
The Bottom Line
The five case series presented in the paper illustrate the interactive effects of intrinsic factors like genetics and dietary responses. Those who are starting a ketogenic diet or have experienced abnormal physiological responses to this diet can and should be tested for underlying predispositions. Collecting information to triangulate the responsible drivers of elevated LDL particles and apoB allows for appropriate diet modifications, unique to the individual. A ketogenic diet often has many metabolic benefits, even among those who respond with an increased burden of potentially atherogenic particles. In such cases, replacing dietary saturated fat or implementing lipid modulating therapies may preserve the diet’s benefits while mitigating possible cardiovascular risks. Thus, I interpret lipoprotein results in the context of other variables in my evaluation of metabolic health and cardiovascular risk. Irrespective of the diet someone chooses, one thing is for certain: people vary greatly in their response to any given diet, making it especially important to track and assess each scenario on an individual basis.
– Peter





When describing the ketogenic diet as high fat, does that term refer to the total grams of fat ingested or just the grams of fat relative to the grams of carbohydrate ingested? If the latter, then all ketogenic diets are high fat, even the ones that emphasize protein. Also were the diets in this study calorie restricted at all? I’d like to see a comparison of HDL. VLDL, IDL, LDL and ApoB 48 and 100 in these two types of ketogenic diets.
It is a shame that the “results” of a study like this will be applied in “broad brush” fashion against the low carb community without any regard to the limitations and qualifications you mention in your analysis above.
I’m just shaking my head (again!)….
Phil
It is very difficult to maintain a ketogenic diet without resorting to increased consumption of saturated fats such as found in cheeses (my favorite).
I note that this paper mentions that one hypercholesterolemic patient refused to change his diet but had a satisfactory low-density lipoprotein cholesterol reduction on ezetimibe.
Given the benefits of a ketogenic diet (or at least a ketogenic-ish low carb/low protein/high fat diet) I wonder out loud whether resort to Ezetimibe prophylaxis could be advised as a first course of action – before even augmentation of MSFA over SFA?
Bottom Line – This paper demonstrates why a full battery of blood tests immediately before and after dramatic changes to lifestyle and/or medication regimens are clearly crucial.
Great post – thanks for the heads up!
Lp(a) also have apoB so if apoB is a better marker than LDL does that not imply that Lp(a) is more important than LDL-C?
One thing I don’t hear discussed often enough is the role of bile acid metabolism, the genes involved, variations from one person to the next, how macros may influence it, how hormones may influence it (insulin, glucagon, etc), if there’s any sort of transcriptional regulation going on with bile acid synthesis, what mediates bile acid resorption in the gut, what changes may be occurring with increased/decreased cholesterol synthesis, level of LDL receptor expression on liver, and then the broader implications of all this stuff to the health of the individual. This is what’s so friggen cool about biology. You can’t study anything in isolation and get anywhere and our tools still seem to be so crude. Like, will AI get to the point where we can model out something as complex as a human being where we can pull various levers and see what effects it has without actually having to study a living person? If we had the tech, would we even want to? What would be the implications of that on society? Would that level of tech in the wrong hands bring about a nightmare dystopian future?
relevant review article to above comment
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4422175/
Dr. Attia,
I have been following you for years and I think you are a brilliant researcher and obsessed with getting to the truth, but in my laymen opinion, I think you just missed a great opportunity to tell people about a long-tested concept that has clinical studies showing huge positive differences with well-known and ever-growing medical issues. Like Virta, a San Francisco based company has clinical showing that this LCHF lifestyle change has reversed Diabetes at a rate of greater than 60%. Where in the heck are the headlines about this? Your current article talks about this Keto approach increasing Total Cholesterol and more specifically LDL and that is valid and has been widely known. Is it the fact that as a cardiologist you are focused on the measurement of Cholesterol and its individual components as the driving factor of heart disease? Could it be that the SAD garbage, processed, laced with junk “vegetable oils” and loaded with sugar American diet is what really got us here? Could Cholesterol be trying to save our lives from this junk, rather than kill us.
Still and fan and follower, but not in this week’s write up….
Thanks Joe,
Believing that eating fatty foods is the root cause of the buildup of atherosclerotic plaques is “nonscientific extrapolation”, and sheer nonsense. When you restrict dietary cholesterol, from any source, your body will synthesize the exact amount it needs to try and function normally. Every cell in the body has the ability to synthesize cholesterol from scratch, if needed, or if someone convinces you to interfere with the synthesis of cholesterol.
Cholesterol is the sturdy fat molecule mother Nature designed to allow plants to leave the ground, and have muscles and nerves. Cholesterol is your bodies basic building block, repair and “starter molecule” for hormones, and even vitamin D production. In reality, cholesterol is a hero, not a villain, giving strength, and flexibility to our cell membranes.
Ansel Keys, and the powerful food/pharma/herbicide industry is the only winner in this dogfight. Peter, you have been duped along with every poor person on this planet cutting out fatty red meat, butter, and cheese. If we as human animals stick to grass fed fats, whole animal products, and look elsewhere for the “root cause” of the buildup of cholesterol in our arteries we wont find opportunity for our magic bullet blockbuster drugs, don’t forget who funds medical research these days, profits supersede science, and common sense.
How ill were these people? did they show up with pain, or complaints? or did their “yearly screening” turn up results used to scare someone off a ketogenic diet?
If you went to a grocery story 20,000 years ago, you would find a ketogenic diet, because fat is our main fuel, it always has been, and always will be.
Sulfur deficiency, related to glyphosate (in almost every processed food you eat), and a breakdown of the glycocalyx is just one of the real root causes of CVD, not butter, and certainly not red meat. Add in a K2 deficiency, and we have calcium building up in arteries, coupled with magnesium deficiencies, and the big one, a vitamin D3 deficiency, and we have the perfect storm. No apoB particle is to blame, (sure its there, getting stuck, that doesn’t make it causal) look at the RAS system, (renin angiotensin system)”and check to see if these people have an “evolutionary” level of vitamin D.
Just because someone wants to put GMO industrial deuterated seed oils loaded with glyphosate in our food, that doesn’t make the food safe for human consumption.
(gout https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3945755/ )
You may consider vitamins and minerals as snake oil, but at least these are natural substances. CAD is multifactorial, and totally epigenetic…
I can’t remember where I read it, but is it true that before they invented the statins, 300 was considered normal cholesterol level?
Dr. Attia is not a cardiologist. And I believe what he is writing here isn’t an argument of the ideal approach to have the best health, but a small nuance not discussed much for a diet pattern (keto) that has gained mainstream practice. Many people try to follow the path you’ve described, eliminating the SAD and the poisons within, using a ketogenic approach and under the physician’s blessing only to find lipid blood markers related to elevated cardiovascular risk have changed undesirably. The article is more a discussion about why one-size-fits-all approaches don’t work.
Great article Peter.
I think some people would have liked you to cover the usual increase in HDLc and the decrease in triglycerides. This group thinks it negates the increased LDLc risk.
Thank you for another great article on cholesterol. I’ve read all of your articles on the topic at least twice, and listened to all of your podcasts on the topic. I still have two questions that I’ve not seen addressed:
1. Can non-oxidized apoB particles lodged in artery walls initiate CHD, or is disease initiated only by oxidized apoB particles in artery walls?
2. What is the cause of apoB particle oxidiation?
Any direction on these two questions is appreciated!
Thanks,
Dave
Very interesting points. I have 5 or 6 SNPs on FTO which indicate a tendency towards insulin resistance in the presence of too much saturated fat vs. mono/poly (via Rhonda Patrick’s genetic tool). I’m remembering a way back in the day podcast that you had with Rudy Leibel which included a discussion about FTO, and his comment that he might start looking at some of these dietary implications on FTO. I’m wondering if he’s done any of that work and I’ll have to check the literature. I’m also ApoE3/4, and have a good deal of lethal heart disease on one side of my family (although they also all smoked). When I utilize ketosis, I am careful to get the majority of my fat from monosaturated sources. And I track ApoB and CRP. Discussions like these and podcasts like yours (I’ve been following you for maybe a decade, since the Insulin Wars days) have certainly given me tools that neither my prior generation relatives had nor my graduate education in physiology gave me. Thank you always.
I think the ultimate goal is a diet that can be free of refined carbs (junk) in the long term. I wonder if the study were longer, would cholesterol levels eventually normalize. By eventually, it could be a couple of years.
If someone is an APOE 3/4 genotype? What would be the best diet to follow?
I have been LC/Keto for about 4 years. My TC, LDL both have remained nearly the same, slightly high (215 and 130). My TG went down by 50% and my HDL up 80% (65 and 60). My concern is that my LDL-P is 2136 and APOb is 108.
As others have mentioned, we expect a ketogenic diet to increase total cholesterol including LDL. But the critical ratios are generally in the preferred range. I’d like to have seen a comparison between the elevated markers in the study and elevated markers from a ketogenic diet with a “normal” response.
That is, how high should one expect his cholesterol to be on a ketogenic diet – at what point should one be concerned?
This is the first time, I have been disturbed by Peter’s analysis. I trust Peter because he usually has no bias or bent. However, I sensed a ketogenic bent in his analysis of this clinical study. He cannot hedge his bets. Either lower LDL and Apo B is good or it is not. If yes, the ketogenic diet is risky, even for healthy people