Want to catch up with other articles from this series?
- The straight dope on cholesterol – Part I
- The straight dope on cholesterol – Part II
- The straight dope on cholesterol – Part III
- The straight dope on cholesterol – Part IV
- The straight dope on cholesterol – Part V
- The straight dope on cholesterol – Part VI
- The straight dope on cholesterol – Part VII
- The straight dope on cholesterol – Part VIII
- The straight dope on cholesterol – Part IX
I’ve been planning to write at length about this topic for a few months, but I’ve been hesitant to do so for several reasons:
- To discuss it properly requires great care and attention (mine and yours, respectively).
- My own education on this topic only really began about 9 months ago, and I’m still learning from my mentors at a geometric pace.
- This topic can’t be covered in one post, even a Peter-Attia-who-can’t-seem-to-say-anything-under-2,000-word post.
- I feel a bit like an imposter writing about lipidology because my mentors on this topic (below) have already addressed this topic so well, I’m not sure I have anything to add.
But here’s the thing. I am absolutely – perhaps pathologically – obsessed with lipidology, the science and study of lipids. Furthermore, I’m getting countless questions from you on this topic. Hence, despite my reservations above, I’m going to give this a shot.
A few thoughts before we begin.
- I’m not even going to attempt to cover this topic entirely in this post, so please hold off on asking questions beyond the scope of this post.
- Please resist the urge to send me your cholesterol numbers. I get about 30 such requests per day, and I cannot practice medicine over the internet. By all means, share your story with me and others, but understand that I can’t really comment other than to say what I pretty much say to everyone: standard cholesterol testing (including VAP) is largely irrelevant and you should have a lipoprotein analysis using NMR spectroscopy (if you don’t know what I mean by this, that’s ok… you will soon).
- This topic bears an upsettingly parallel reality to that of nutrition “science” in that virtually all health care providers have no understanding of it and seem to only reiterate conventional wisdom (e.g., “LDL is bad,” “HDL is good”). We’ll be blowing the doors off this fallacious logic.
By the end of this series, should you choose to internalize this content (and pick up a few homework assignments along the way), you will understand the field of lipidology and advanced lipid testing better than 95% of physicians in the United States. I am not being hyperbolic.
One last thing before jumping in: Everything I have learned and continue to learn on this topic has been patiently taught to me by the words and writings of my mentors on this subject: Dr. Tom Dayspring, Dr. Tara Dall, Dr. Bill Cromwell, and Dr. James Otvos. I am eternally in their debt and see it as my duty to pass this information on to everyone interested.
Are you ready to start an exciting journey?
Concept #1 – What is cholesterol?
Cholesterol is a 27-carbon molecule shown in the figure below. Each line in this figure represents a bond between two carbon atoms. Sorry, I’ve got to get it out there. That’s it. Mystery over.
All this talk about “cholesterol” and most people don’t actually know what it is. So there you have it. Cholesterol is “just” another organic molecule in our body.
I need to make one important distinction that will be very important later. Cholesterol, a steroid alcohol, can be “free” or “unesterified” (“UC” as we say, which stands for unesterified cholesterol) which is its active form, or it can exist in its “esterified” or storage form which we call a cholesterol ester (“CE”). The diagram above shows a free (i.e., UC) molecule of cholesterol. An esterified variant (i.e., CE) would have an “attachment” where the arrow is pointing to the hydroxyl group on carbon #3, aptly named the “esterification site.”
Since cholesterol can only be produced by organisms in the Animal Kingdom it is termed a zoosterol. In a subsequent post I will write about a cousin of cholesterol called phytosterol, but at this time I think the introduction would only confuse matters. So, if you have a question about phytosterols, please hang on.
Concept #2 – What is the relationship between the cholesterol we eat and the cholesterol in our body?
We ingest (i.e., take in) cholesterol in many of the foods we eat and our body produces (“synthesizes”) cholesterol de novo from various precursors. About 25% of our daily “intake” of cholesterol – roughly 300 to 500 mg — comes from what we eat (called exogenous cholesterol), and the remaining 75% of our “intake” of cholesterol — roughly 800 to 1,200 mg – is made by our body (called endogenous production). To put these amounts in context, consider that total body stores of cholesterol are about 30 to 40 gm (i.e., 30,000 to 40,000 mg) and most of this resides within our cell membranes. Every cell in the body can produce cholesterol and thus very few cells actually require a delivery of cholesterol. Cholesterol is required by all cell membranes and to produce steroid hormones and bile acids.
Of this “made” or “synthesized” cholesterol, our liver synthesizes about 20% of it and the remaining 80% is synthesized by other cells in our bodies. The synthesis of cholesterol is a complex four-step process (with 37 individual steps) that I will not cover here (though I will revisit), but I want to point out how tightly regulated this process is, with multiple feedback loops. In other words, the body works very hard (and very “smart”) to ensure cellular cholesterol levels are within a pretty narrow band (the overall process is called cholesterol homeostasis). Excess cellular cholesterol will crystalize and cause cellular apoptosis (programmed cell death). Plasma cholesterol levels (which is what clinicians measure with standard cholesterol tests) often have little to do with cellular cholesterol, especially artery cholesterol, which is what we really care about. For example, when cholesterol intake is decreased, the body will synthesize more cholesterol and/or absorb (i.e., recycle) more cholesterol from our gut. The way our body absorbs cholesterol is so amazing, so I want to spend a bit of time discussing it.
In medical school, whenever we had to study physiology or pathology I always had a tendency to want to anthropomorphize everything. It’s just how my brain works, I guess, and understanding cholesterol absorption is a great example of this sort of thinking. The figure below, from the Gastroenterology Journal, shows a cross-section of a cell in our small intestine (i.e., our “gut”) called an enterocyte that governs how stuff in our gut actually gets absorbed. The left side with the fuzzy border is the side facing the “lumen” (the inside of the “tube” that makes up our gut). You’ll notice two circles on that side of the cell, a blue one and a pink one.
[What follows is a bit more technical than I would have liked, but I think it’s very important to understand how this process of cholesterol absorption works. It’s certainly worth reading this a few times to make sure it sinks in.]
- The blue circle represents something called a Niemann-Pick C1-like 1 protein (NPC1L1). It sits at the apical surface of enterocytes and it promotes active influx (i.e., bringing in) of gut luminal unesterified cholesterol (UC) as well as unesterified phytosterols into the enterocyte. Think of this NPC1L1 as the ticket-taker at the door of the bar (where the enterocyte is the “bar”); he lets most cholesterol (“people”) in. However, NPC1L1 cannot distinguish between cholesterol (“good people”) and phytosterol (“bad people” – I will discuss these guys later, so no need to worry about it now) or even too much cholesterol (“too many people”). [I can’t take any credit for this anthropomorphization – this is how Tom Dayspring explained it to me!]
- The pink circle represents an adenosine triphosphate (ATP)-binding cassette (ABC) transporters ABCG5 and ABCG8. This complex promotes active efflux (i.e., kicking out) of unesterified sterols (cholesterol and plant sterols – of which over 40 exist) from enterocytes back into the intestinal lumen for excretion. Think of ABCG5,G8 as the bouncer at the bar; he gets rid of the really bad people (e.g., phytosterols as they serve no purpose in humans) you don’t want in the bar who snuck past the ticket-taker (NPC1L1). Of course in cases of hyperabsorption (i.e., in cases where the gut absorbs too much of a good thing) they can also efflux out un-needed cholesterol. Along this analogy, once too many “good people” get in the bar, fire laws are violated and some have to go. The enterocyte has “sterol-excess sensors” (a nuclear transcription factor called LXR) that do the monitoring and these sensors activate the genes that regulate NPC1L1 and ABCG5,G8).
There is another nuance to this, which is where the CE versus UC distinction comes in:
- Only free or unesterified cholesterol (UC) can be absorbed through gut enterocytes. In other words, cholesterol esters (CE) cannot be absorbed because of the bulky side chains they carry.
- Much (> 50%) of the cholesterol we ingest from food is esterified (CE), hence we don’t actually absorb much, if any, exogenous cholesterol (i.e., cholesterol in food). CE can be de-esterified by pancreatic lipases and esterolases – enzymes that break off the side branches and render CE back to UC — so some ingested CE can be converted to UC.
- Furthermore, most of the unesterified cholesterol (UC) in our gut (on the order of about 85%) is actually of endogenous origin (meaning it was synthesized in bodily cells and returned to the liver), which ends up in the gut via biliary secretion and ultimately gets re-absorbed by the gut enterocyte. The liver is only able to efflux (send out via bile into the gut) UC, but not CE, from hepatocytes (liver cells) to the biliary system. Liver CE cannot be excreted into bile. So, if the liver is going to excrete CE into bile and ultimately the gut, it needs to de-esterify it using enzymes called cholesterol esterolases which can convert liver CE to UC.
- Also realize that the number one way for the liver to rid itself of cholesterol is to convert the cholesterol into a bile acid, efflux that to the bile (via a transporter called ABCB11) and excrete the bile acids in the stool (typically most bile acids are reabsorbed at the ileum).
Concept #3 – Is cholesterol bad?
One of the biggest misconceptions out there (maybe second only to the idea that eating fat makes you fat) is that cholesterol is “bad.” This could not be further from the truth. Cholesterol is very good! In fact, there are (fortunately rare) genetic disorders in which people cannot properly synthesize cholesterol. Once such disease is Smith-Lemli-Opitz syndrome (also called “SLOS,” or 7-dehydrocholesterol reductase deficiency) which is a metabolic and congenital disorder leading to a number of problems including autism, mental retardation, lack of muscle, and many others.
Cholesterol is absolutely vital for our existence. Let me repeat: Cholesterol is absolutely vital for our existence. Every cell in our body is surrounded by a membrane. These membranes are largely responsible for fluidity and permeability, which essentially control how a cell moves, how it interacts with other cells, and how it transports “important” things in and out. Cholesterol is one of the main building blocks used to make cell membranes (in particular, the ever-important “lipid bilayer” of the cell membrane).
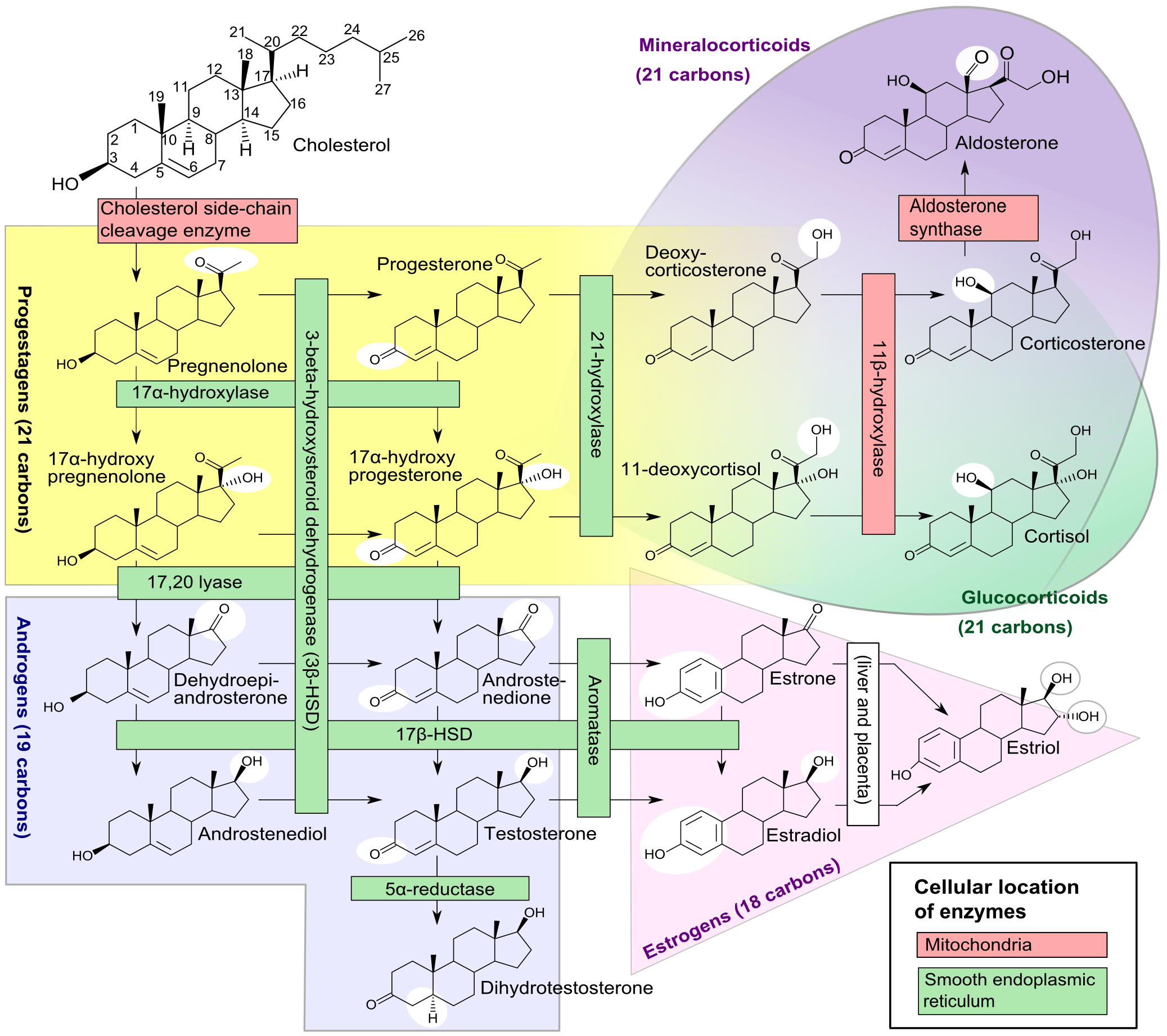
Beyond cholesterol’s role in allowing cells to even exist, it also serves an important role in the synthesis of vitamins and steroid hormones, including sex hormones and bile acids. Make sure you take a look at the picture of steroid hormones synthesis and compare it to that of cholesterol (above). If this comparison doesn’t convince you of the vital importance of cholesterol, nothing I say will.
One of the unfortunate results of the eternal need to simplify everything is that we (i.e., the medical establishment) have done the public a disservice by failing to communicate that there is no such thing as “bad” cholesterol or “good” cholesterol. All cholesterol is good!
The only “bad” outcome is when cholesterol ends up inside of the wall of an artery, most famously the inside of a coronary artery or a carotid artery, AND leads to an inflammatory cascade which results in the obstruction of that artery (make sure you check out the pictures in the links, above). When one measures cholesterol in the blood – we really do not know the final destination of those cholesterol molecules!
And that’s where we’ll pick it up next time – how does “good” cholesterol end up in places it doesn’t belong and cause “bad” problems? If anyone is looking for a little extra understanding on this topic, please, please, please check out my absolute favorite reference for all of my cholesterol needs, LecturePad. It’s designed primarily for physicians, but I suspect many of you out there will find it helpful, if not now, certainly once we’re done with this series.
To summarize this somewhat complex issue
- Cholesterol is “just” another fancy organic molecule in our body, but with an interesting distinction: we eat it, we make it, we store it, and we excrete it – all in different amounts.
- The pool of cholesterol in our body is essential for life. No cholesterol = no life.
- Cholesterol exists in 2 forms – UC and CE – and the form determines if we can absorb it or not, or store it or not (among other things).
- Most of the cholesterol we eat is not absorbed and is excreted by our gut (i.e., leaves our body in stool). The reason is it not only has to be de-esterified, but it competes for absorption with the vastly larger amounts of UC supplied by the biliary route.
- Re-absorption of the cholesterol we synthesize in our body is the dominant source of the cholesterol in our body. That is, most of the cholesterol in our body was made by our body.
- The process of regulating cholesterol is very complex and multifaceted with multiple layers of control. I’ve only touched on the absorption side, but the synthesis side is also complex and highly regulated. You will discover that synthesis and absorption are very interrelated.
- Eating cholesterol has very little impact on the cholesterol levels in your body. This is a fact, not my opinion. Anyone who tells you different is, at best, ignorant of this topic. At worst, they are a deliberate charlatan. Years ago the Canadian Guidelines removed the limitation of dietary cholesterol. The rest of the world, especially the United States, needs to catch up.



