Adam Cohen is an orthopedic surgeon with expertise in sports medicine. In this episode, Adam breaks down the anatomy of the lower extremities: the hip, knee, ankle, and foot. He explains in detail the common injuries, sources of pain, and what leads to the development of arthritis. He lays out the non-surgical and surgical treatment options as well as the factors that determine whether surgery is appropriate. The discussion includes various procedures like hip replacement, knee replacement, ACL reconstruction, repair of meniscus tears, and more. Additionally, Adam sheds light on the utility of biological therapies like stem cells and platelet-rich plasma (PRP) and how they compare to more traditional approaches.
Subscribe on: APPLE PODCASTS | RSS | GOOGLE | OVERCAST | STITCHER

(NOTE: Find video clips of exams that Adam performed on Peter at the end of the show notes)
We discuss:
- Anatomy of the hip, hip dysplasia in infants, and the development of arthritis [3:00];
- Diagnosing hip pain in people under 50, stress fractures in the femoral neck, and more [11:15];
- Common hip injuries, gender differences, and problems that occur when the hip isn’t formed normally [19:30];
- Advancements in hip replacement surgery [25:15];
- Common hip problems in people over age 60 [27:30];
- The importance of muscular strength around the hips for injury prevention [30:30];
- Hip fractures due to osteopenia and osteoporosis [36:00];
- The utility of biological therapies like stem cells and platelet-rich plasma (PRP) [40:30];
- Cortisone as a treatment to delay the need for surgical intervention [53:30];
- Anatomy of the knee [56:30];
- Are activities like running that amplify forces bad for the knee? [59:45];
- Risk of future knee issues and arthritis following an ACL tear or other substantial knee injury [1:04:30];
- How the ACL injury happens and how it is repaired [1:08:30];
- Arthritis of the knee [1:19:00];
- Meniscus tears: how they happen and when surgery is appropriate [1:21:30];
- Total knee replacement: when it’s appropriate and how the recovery process compares to hip replacement [1:30:30];
- Surgical vs. non-surgical approaches to various knee injuries [1:40:45];
- Achilles tendon: tendinitis, rupture of the Achilles tendon, and prevention strategies [1:44:15];
- Anatomy of the ankle and foot [1:49:00];
- Common injuries to the ankle and foot [1:51:15];
- Tips for finding a good orthopedic surgeon [2:01:45]; and
- More.
Get Peter’s expertise in your inbox 100% free.
Sign up to receive An Introductory Guide to Longevity by Peter Attia, weekly longevity-focused articles, and new podcast announcements.
Anatomy of the hip, hip dysplasia in infants, and the development of arthritis [3:00]
- The hip joint is a ball and socket joint
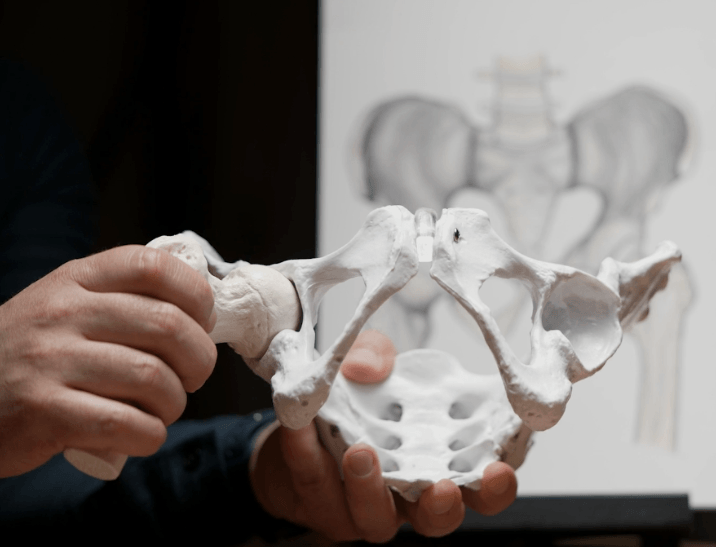
Figure 1. Model of the hip joint
- Unlike the shoulder, it’s a very contained concentric joint and much more stable under normal circumstances than the shoulder
- It’s a deep socket
- The socket is called the acetabulum
- The femoral head, it is covered with cartilage
- If we just focus on the proximal femur (shown below), we have the head, the neck, the subtrochanteric region, and the trochanteric region
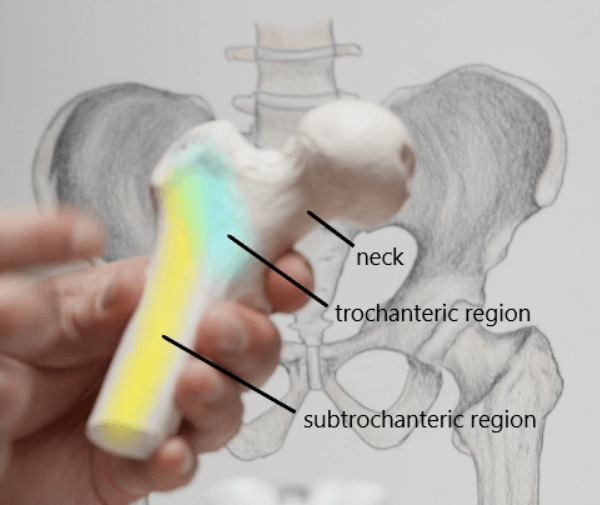
Figure 2. Model of the proximal femur.
Many problems in the hip begin during development
- The acetabulum is formed in utero beginning about fourth week, and then by the 30th week it starts to develop
- This is a good starting spot because a number of the problems seen in the hip start that early
- There is a condition called developmental dysplasia of the hip
- It used to be referred to as congenital dysplasia of the hip, but there are more factors involved than any congenital ones in particular
Basically what happens is if the hip is not concentrically reduced either late in stages of pregnancy or in early childhood (the first several months of life), the acetabulum will not form properly
- For example, if the ball is shifted out of the socket, let’s say due to positioning in utero where it’s not completely in, the acetabulum will not form correctly
- What that means is that after birth, if it’s sitting outward, this deep socket will not form and it’ll be quite shallow
- That has major implications later in life because if it’s not deep in the socket, it’s sitting on the edge of the socket, which means there’s greater pressure here, and that pressure can lead to mechanical overload and arthritis
“Even conditions that happen much later in life can start quite early”‒ Adam Cohen
Peter’s son had hip dysplasia at birth
- One of Peter’s kids was breached, and as soon as he was born, they immediately said he has hip dysplasia
- He was in a brace (called a Pavlik harness), splayed open for nine months
- It’s actually quite comfortable for the child
- He basically only came out of it for a bath
- But nine months later, his hips were fine (remarkably)
Adam’s takeaway ‒ We know that if the ball is not sitting in that socket, it will not form properly
- So the harness keeps that positioning until the acetabulum forms properly
- The exams that pediatricians do, we always check the hip and we want to make sure that it’s in the socket
- Going forward, a lot more physicians and orthopedic pediatric specialists are using ultrasound to better quantify that the hip is in the socket because we really don’t want to miss any dysplastic hips
If you have a dysplastic hip, you are going to get arthritis
- Dysplastic hips are not necessarily symptomatic
- It doesn’t mean you’re going to need a hip replacement
- But the acetabulum is not formed properly, and it’s a mechanical problem where the forces are unevenly distributed across that ball and there’s edge loading and that will break down over time no matter what you do
- People with this are going to get arthritis
Do we have a sense of the incidence of developmental dysplasia of the hip?
- It’s about 1 in 1,000
- Discussed in JAMA in 2022
- An exam would miss more than ultrasound, and we shouldn’t miss any
- The ultrasound is not that hard to do (certainly teachable), and it confirms that the ball is in the socket and the socket is healing properly
- An animal study done many, many years ago put a cube shaped object in the acetabulum and found the acetabulum formed in the shape of a cube
- It is going to develop based on what is sitting in that area
- If you wait too long, what happens is the soft tissue deep in the socket will become hypertrophied and it’s harder to get in
- Adam has patients (age 28-29) come to see him because their hip hurts
- They never had a problem before, did not suspect anything wrong
- They get an x-ray of the hip and are shocked to learn they have arthritis
Arthritis of the hip [8:45]
Arthritis can be diagnosed with an x-ray
- A plain x-ray is good enough to diagnose arthritis when it is symptomatic because you’ll see the absence or thinning of cartilage
- There is a spectrum where the process starts to happen before we’re even clinically aware of it, and detecting that is the future
- The trick is to find out before someone has clinical arthritis: do we know about it, and what can we do to avoid it?
Defining arthritis [9:30]
- This is an important conversation Adam has with his patients
- The ends of all long bones have cartilage at the end (it’s a very smooth layer), and the only reason joints move pain free, without friction, is because of that cartilage
- The coefficient of friction of cartilage is so smooth
- It’s smoother than ice on ice; it’s smoother than Teflon
- Cartilage is a biological substance that is constantly remodeling (albeit slowly) and can adjust to pressures
- Part of arthritis is the loss of that cartilage
- The cartilage starts to thin
- Cartilage itself is avascular, and it gets nutrition through diffusion from the joints
- Chondrocytes (which is the cell of cartilage) create proteins to make the extracellular matrix so that it remains healthy, but they’re not very efficient at making the extracellular matrix, which is imperative
- If there is overload of the cartilage, the chondrocytes will respond and sometimes they die, sometimes they go into senescence
- Take the knee for example, 2% of the cartilage is chondrocytes
- They don’t have a lot of leeway when the load is substantial
Diagnosing hip pain in people under 50, stress fractures in the femoral neck, and more [11:15]
When a person comes to your office complaining of hip pain, what are the top three most common diagnoses for a person under 50?
- Right away, Adam is thinking about the different layers of the hip from deep to superficial
{end of show notes preview}
Would you like access to extensive show notes and references for this podcast (and more)?
Check out this post to see an example of what the substantial show notes look like. Become a member today to get access.

Adam Cohen, M.D.
Adam Cohen earned his Bachelor’s Degree from Washington University in St. Louis. He then earned his Medical Degree from New York Medical College where he received AOA Academic Honors and the Trustee Merit Scholarship for Academic Excellence. He completed his internship in general surgery and residency in orthopedic surgery at the St. Luke’s-Roosevelt Department of Orthopedics in New York City. He went on to do a research fellowship in Knee and Sports Medicine in San Diego. Dr. Cohen then returned to Manhattan to practice medicine and earned an appointment as an Assistant Clinical Professor at Columbia University from 2004-2014. During this time he also served as the Assistant Team Physician for the New York Yankees (from 2004-2008). He also served as a consultant for the US Open Tennis Championships and provided orthopedic coverage for the New York City Ballet.
Currently, Dr. Cohen is the Director of Sports Medicine at OrthoManhattan and serves as the Team Physician for Horace Mann Athletics. He holds academic appointments at the NYU Langone Health System and the Mount Sinai Health System.
Dr. Cohen has been recognized as a Castle-Connolly Top Doctor since 2015 and has been selected to appear in New York Magazine’s Top Doctor issue in 2017, 2018, 2019 and 2020. He also received the Mount Sinai Orthopedic Residency “Teacher of the Year” honors in 2017.
Dr. Cohen has advanced training and expertise in sports medicine injuries of the shoulder, elbow, hip, knee and ankle. He has extensive experience in arthroscopic minimally invasive surgery and advanced reconstructive procedures, including shoulder and knee replacement surgery. [AdamCohenMD.com]
Website: adamcohenmd.com
Facebook: Adam Cohen MD – Orthopedic Surgeon and Sports Medicine Specialist