Guest Episode
Women’s sexual health, menopause, and hormone replacement therapy (HRT)
Guest Episode
Cardiovascular disease, the number one killer: development, biomarkers, apoB, cholesterol, brain health, and more
Guest Episode
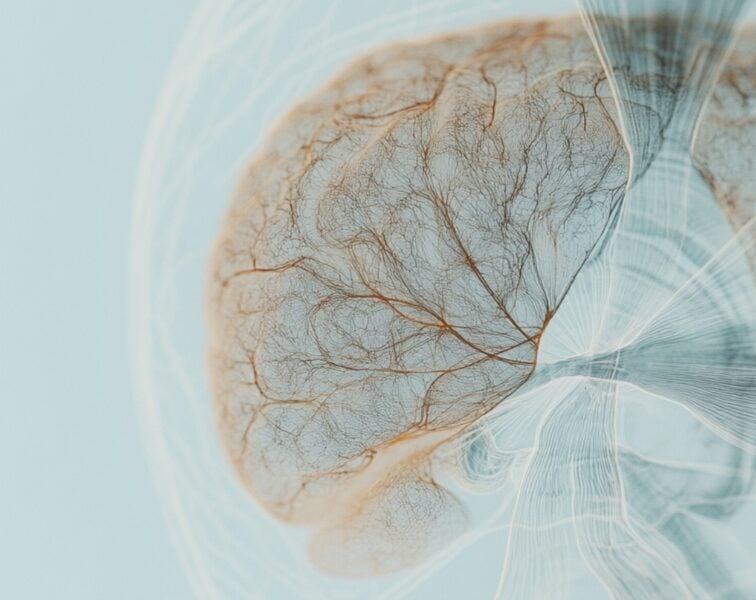
A breakthrough in Alzheimer’s disease: the promising potential of klotho for brain health, cognitive decline, and as a therapeutic tool for Alzheimer's disease
Free Article
Aerobic exercise for Parkinson’s disease
Free Article