Want to catch up with other articles from this series?
- The straight dope on cholesterol – Part I
- The straight dope on cholesterol – Part II
- The straight dope on cholesterol – Part III
- The straight dope on cholesterol – Part IV
- The straight dope on cholesterol – Part V
- The straight dope on cholesterol – Part VI
- The straight dope on cholesterol – Part VII
- The straight dope on cholesterol – Part VIII
- The straight dope on cholesterol – Part IX
Previously, in Part I, Part II, Part III, Part IV and Part V of this series, we addressed these 7 concepts:
#1 — What is cholesterol?
#2 — What is the relationship between the cholesterol we eat and the cholesterol in our body?
#3 — Is cholesterol bad?
#4 — How does cholesterol move around our body?
#5 – How do we measure cholesterol?
#6 – How does cholesterol actually cause problems?
#7 – Does the size of an LDL particle matter?
(Not so) quick refresher on take-away points from previous posts, should you need it:
- Cholesterol is “just” another fancy organic molecule in our body but with an interesting distinction: we eat it, we make it, we store it, and we excrete it – all in different amounts.
- The pool of cholesterol in our body is essential for life. No cholesterol = no life.
- Cholesterol exists in 2 forms – unesterified or “free” (UC) and esterified (CE) – and the form determines if we can absorb it or not, or store it or not (among other things).
- Much of the cholesterol we eat is in the form of CE. It is not absorbed and is excreted by our gut (i.e., leaves our body in stool). The reason this occurs is that CE not only has to be de-esterified, but it competes for absorption with the vastly larger amounts of UC supplied by the biliary route.
- Re-absorption of the cholesterol we synthesize in our body (i.e., endogenous produced cholesterol) is the dominant source of the cholesterol in our body. That is, most of the cholesterol in our body was made by our body.
- The process of regulating cholesterol is very complex and multifaceted with multiple layers of control. I’ve only touched on the absorption side, but the synthesis side is also complex and highly regulated. You will discover that synthesis and absorption are very interrelated.
- Eating cholesterol has very little impact on the cholesterol levels in your body. This is a fact, not my opinion. Anyone who tells you different is, at best, ignorant of this topic. At worst, they are a deliberate charlatan. Years ago the Canadian Guidelines removed the limitation of dietary cholesterol. The rest of the world, especially the United States, needs to catch up. To see an important reference on this topic, please look here.
- Cholesterol and triglycerides are not soluble in plasma (i.e., they can’t dissolve in water) and are therefore said to be hydrophobic.
- To be carried anywhere in our body, say from your liver to your coronary artery, they need to be carried by a special protein-wrapped transport vessel called a lipoprotein.
- As these “ships” called lipoproteins leave the liver they undergo a process of maturation where they shed much of their triglyceride “cargo” in the form of free fatty acid, and doing so makes them smaller and richer in cholesterol.
- Special proteins, apoproteins, play an important role in moving lipoproteins around the body and facilitating their interactions with other cells. The most important of these are the apoB class, residing on VLDL, IDL, and LDL particles, and the apoA-I class, residing for the most part on the HDL particles.
- Cholesterol transport in plasma occurs in both directions, from the liver and small intestine towards the periphery and back to the liver and small intestine (the “gut”).
- The major function of the apoB-containing particles is to traffic energy (triglycerides) to muscles and phospholipids to all cells. Their cholesterol is trafficked back to the liver. The apoA-I containing particles traffic cholesterol to steroidogenic tissues, adipocytes (a storage organ for cholesterol ester) and ultimately back to the liver, gut, or steroidogenic tissue.
- All lipoproteins are part of the human lipid transportation system and work harmoniously together to efficiently traffic lipids. As you are probably starting to appreciate, the trafficking pattern is highly complex and the lipoproteins constantly exchange their core and surface lipids.
- The measurement of cholesterol has undergone a dramatic evolution over the past 70 years with technology at the heart of the advance.
- Currently, most people in the United States (and the world for that matter) undergo a “standard” lipid panel, which only directly measures TC, TG, and HDL-C. LDL-C is measured or most often estimated.
- More advanced cholesterol measuring tests do exist to directly measure LDL-C (though none are standardized), along with the cholesterol content of other lipoproteins (e.g., VLDL, IDL) or lipoprotein subparticles.
- The most frequently used and guideline-recommended test that can count the number of LDL particles is either apolipoprotein B or LDL-P NMR, which is part of the NMR LipoProfile. NMR can also measure the size of LDL and other lipoprotein particles, which is valuable for predicting insulin resistance in drug naïve patients, before changes are noted in glucose or insulin levels.
- The progression from a completely normal artery to a “clogged” or atherosclerotic one follows a very clear path: an apoB containing particle gets past the endothelial layer into the subendothelial space, the particle and its cholesterol content is retained, immune cells arrive, an inflammatory response ensues “fixing” the apoB containing particles in place AND making more space for more of them.
- While inflammation plays a key role in this process, it’s the penetration of the endothelium and retention within the endothelium that drive the process.
- The most common apoB containing lipoprotein in this process is certainly the LDL particle. However, Lp(a) and apoB containing lipoproteins play a role also, especially in the insulin resistant person.
- If you want to stop atherosclerosis, you must lower the LDL particle number.
- At first glance it would seem that patients with smaller LDL particles are at greater risk for atherosclerosis than patients with large LDL particles, all things equal.
- “A particle is a particle is a particle.” If you don’t know the number, you don’t know the risk.
- To address this question, however, one must look at changes in cardiovascular events or direct markers of atherosclerosis (e.g., IMT) while holding LDL-P constant and then again holding LDL size constant. Only when you do this can you see that the relationship between size and event vanishes. The only thing that matters is the number of LDL particles – large, small, or mixed.
Concept #8 – Why is it necessary to measure LDL-P, instead of just LDL-C?
In the growing list of reasons why I used to refer to myself as “chick-repellant” in college, I have a confession to make: I find the topic of statistical concordance and discordance to be so exciting, I sometimes have a hard time containing myself. This may explain the paucity of girlfriends in college. Let me use an example to illustrate the distinction between these terms. Let’s say you want to predict the change in home prices in the following year (I used to model this for a living). There are at least a dozen parameters linked to this, including: GDP growth, unemployment, interest rates (both short term and long term, though to different degrees), housing inventory (i.e., how many houses are on the market), housing absorption (i.e., how quickly houses go from being on the market to being sold), major stock indices, and consumer confidence. Historically, from the mid-1990’s until about the fourth quarter of 2006, this worked like clockwork. While each of these variables had differing strengths of predicting changes in home prices, they all moved together. For example, when GDP growth was robust, unemployment was low, interest rates were modest, housing inventories were about 60 to 90 days, etcetera. All of these variables pointed to a predictable change in home values.
Around Q42006 (i.e., last 3 months of 2006), one of these variables began to deviate from the others. The details aren’t important, but the point is one variable began to suggest home prices would fall while the others all pointed to a continued rise. Prior to Q42006 these parameters were said to be concordant – they all predicted the same thing – either up or down. By 2007, they became discordant – one variable said the sky was falling while others said everything was fine.
This was true on the “micro” level, too. [What I described above is called “macro” level.] As a lender, it should be very important to know the risk of each and every loan you make (clearly this was part of the root problem in the age of mass securitization). Will this person pay the loan back or will they default?
Same game here, but now a new set of even greater variables. As a lender, if I want to know if YOU will default, I will want to know a lot of things about you, such as your agency credit risk scores, your bank account activity, payroll activity, how much you’re borrowing relative to the value of your house, where your house is located, and about 50 other things (literally).
Not surprisingly, the same thing that happened on the macro side happened on the micro side. It became difficult to predict who would default and would not default because there were so many variables to consider and lenders didn’t know which ones were still predictive. The models that predict default are very sensitive to the balance of these inputs. When all of the variables are concordant, their accuracy is prophetic, as was the case from the mid-1990s until late 2006. When some variables become discordant with each other, especially variables that were historically concordant with each other, really bad stuff happens, as became evident to me, personally, one Thursday afternoon in November 2007. It became clear the sky was about to fall. And, of course, it did.
What does real estate have to do with atherosclerosis?
Fortunately, predicting heart disease is a little easier than predicting changes in home prices. It’s not perfect, of course, but it’s pretty good. Why is it not perfect? For one thing, we can’t do the “perfect” experiment. The “perfect” experiment would look something like this:
Take 100,000 people and randomize them into four matched groups, A, B, C, and D. Wave a magic wand (you can see why this experiment hasn’t been and won’t be done) and give the folks in Group A an LDL particle concentration of, say, 700 nmol/L; those in Group B you give 1,200 nmol/L; those in Group C you give 1,600 nmol/L; and those in Group D get 2,000 nmol/L.
In our dream world, due to the randomization process, these four groups would be statistically identical in every way except one – they would, thanks to our magic wand, have a different number of LDL particles. We would follow them without further intervention for 10 years and then compare their rates of heart disease, stroke, and death.
There are some areas in medicine where we can do such experiments. But, we can’t do this experiment for this question. Even when we do the next best thing — give people a drug that lowers their LDL-P and measure the impact of this intervention — there is always a chance we’ve done something in addition to “just” lowering LDL-P. If you’ve been reading this series, you no doubt know my thoughts on this: while other factors are likely to be involved the pathogenesis of atherosclerosis (e.g., endothelial “health”, normal versus abnormal inflammatory response) the primary driver of atherosclerosis is the number of apoB trafficking lipoproteins in circulation, of which LDL particles are the vast majority.
The data below should further clarify this association.
What do concordant LDL-C and LDL-P values look like?
Among the two largest studies tracking the association between cholesterol and atherosclerotic mortality are the Framingham study and the MESA trial (the two largest trials were AMORIS and INTERHEART). The figure below, which I’ve graciously borrowed from Jim Otvos, shows the risk stratification of LDL-C (top) and LDL-P (bottom) from the Framingham study and MESA trial, respectively. As you can see, conveniently, LDL-C values in mg/dL are about 10x off from LDL-P values in nmol/L. In other words, in the Framingham population, the 20th percentile value of LDL-C was 100 mg/dL, while the MESA trial found the 20th percentile of the population to have an LDL-P concentration of 1,000 nmol/L. As you will see by the end of this post, this “rule of the thumb” should never be used to infer LDL-P from LDL-C.
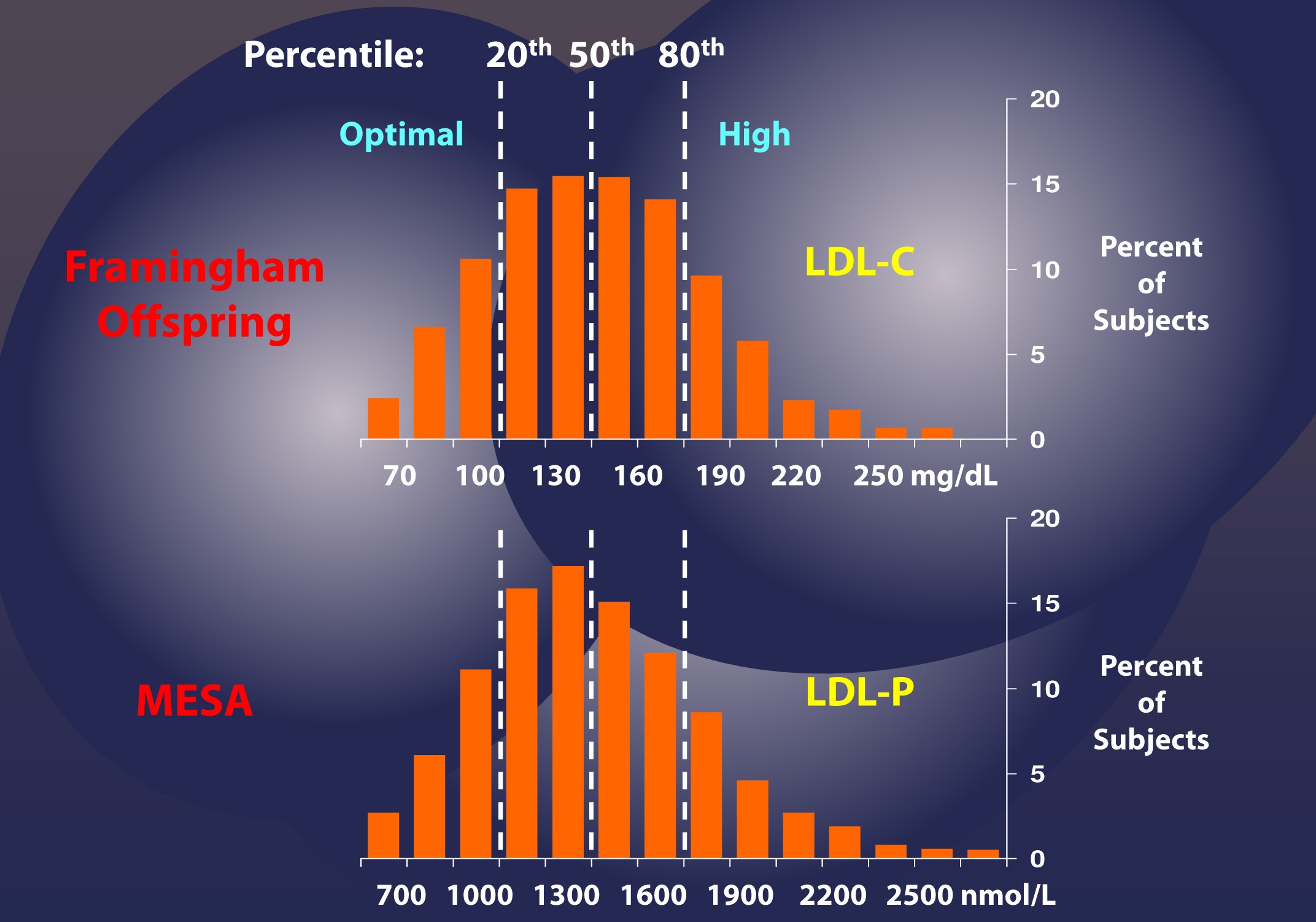
If this were always the case – that is, if LDL-C and LDL-P were always concordant – we could conclude that LDL-C and LDL-P would be of equal value in predicting heart disease. Obviously this is not the case, or I wouldn’t be making such a fuss over the distinction. But how bad is it?
What do discordant LDL-C and LDL-P values look like?
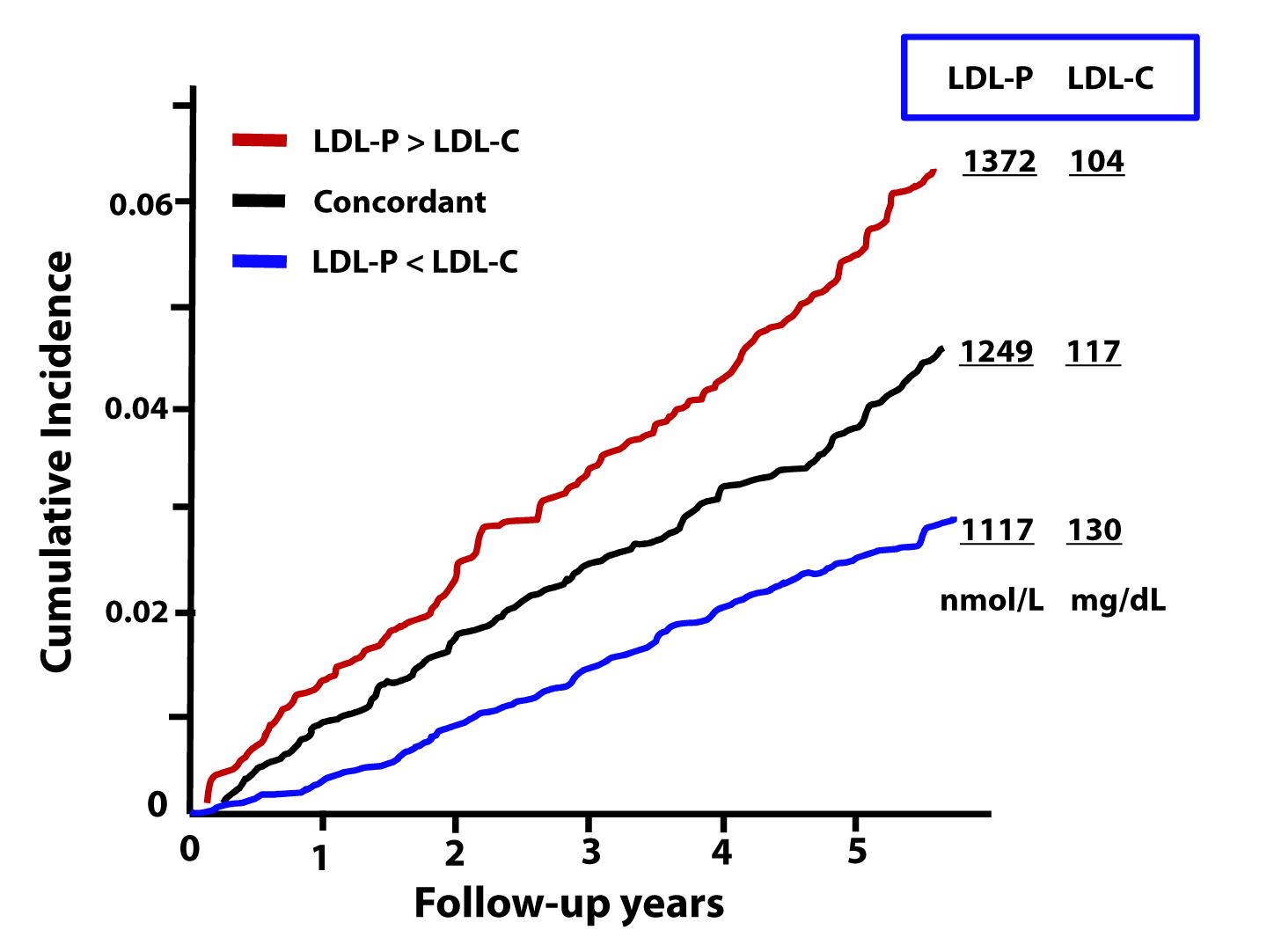
The figure below, from the Journal of Clinical Lipidology, shows the cumulative incidence of cardiovascular events (e.g., myocardial infarction, death) over time in three sub-populations:
- Those with concordant LDL-P and LDL-C (black line);
- Those with discordant LDL-P and LDL-C (LDL-P>LDL-C, shown by the red line);
- Those with discordant LDL-P and LDL-C (LDL-P<LDL-C, shown by the blue line).
This analysis was done using a Cox proportional hazard model and was adjusted for age, sex, and race. The steeper the line the more people in that sub-population died or experienced adverse cardiac events relative to other sub-populations. In other words, the folks in the red group had the worst outcomes, followed by the folks in the black group, followed by the folks in the blue group.
What can we infer from these data?
First, we confirm what I alluded to above. Namely, that a non-zero percent of the population do not have LDL-C and LDL-P values that predict the same level of risk. However, and perhaps more importantly, we get another look at an important theme of this series: LDL-P is driving atherosclerotic risk, not LDL-C. If LDL-P and LDL-C were equally “bad” – even when discordant – you would expect the blue line to be as steep as the red line (and both to be steeper than the black line). But this is not the case.
Let’s look at these data parsed out another way. Below we see the four possible subgroups, from the top:
- Not low LDL-P, low LDL-C (red line);
- Not low LDL-P, not low LDL-C (yellow line);
- Low LDL-P, low LDL-C (black line); and
- Low LDL-P, not low LDL-C (blue line).
Note that “low” is defined below the 30th percentile and “not low” is defined as greater than 30th percentile for each variable. This figure is even more revealing than the one above. Again, it demonstrates the frequency of discordance (about 20% in this population with these cut-off points), and it shows the importance of LDL-P’s predictive power, relative to that of LDL-C.
In fact, though not statistically significant, the highest risk group has high LDL-P and actually has low LDL-C (I’ll give you a hint of why, below) while the lowest risk group has low LDL-P and not-low LDL-C. *This is not a typo.
The highest risk and lowest risk groups are those with discordant LDL-C and LDL-P. The high risk group has high LDL-P and low LDL-C, while the lowest risk group has high LDL-C with low LDL-P. Only a minority of physicians would know that there is a segment of the population with elevated LDL-C who are at low risk! The same conclusion will be drawn from the next study.
Let’s look at an even longer-term follow up study, below. This study followed a Framingham offspring cohort of about 2,500 patients over a median time period of almost 15 years in each of the four possible groups (i.e., high-high, high-low, low-high, and low-low) and tracked event-free survival. In this analysis the cut-off points for LDL-P and LDL-C were the median population values of 1,414 nmol/L and131 mg/dL, respectively. So “high” implies above these values; “low” implies below these values. Kaplan-Meier survival curves are displayed over a 16 year period – the steeper the slope of the line the worse the outcome (survival).
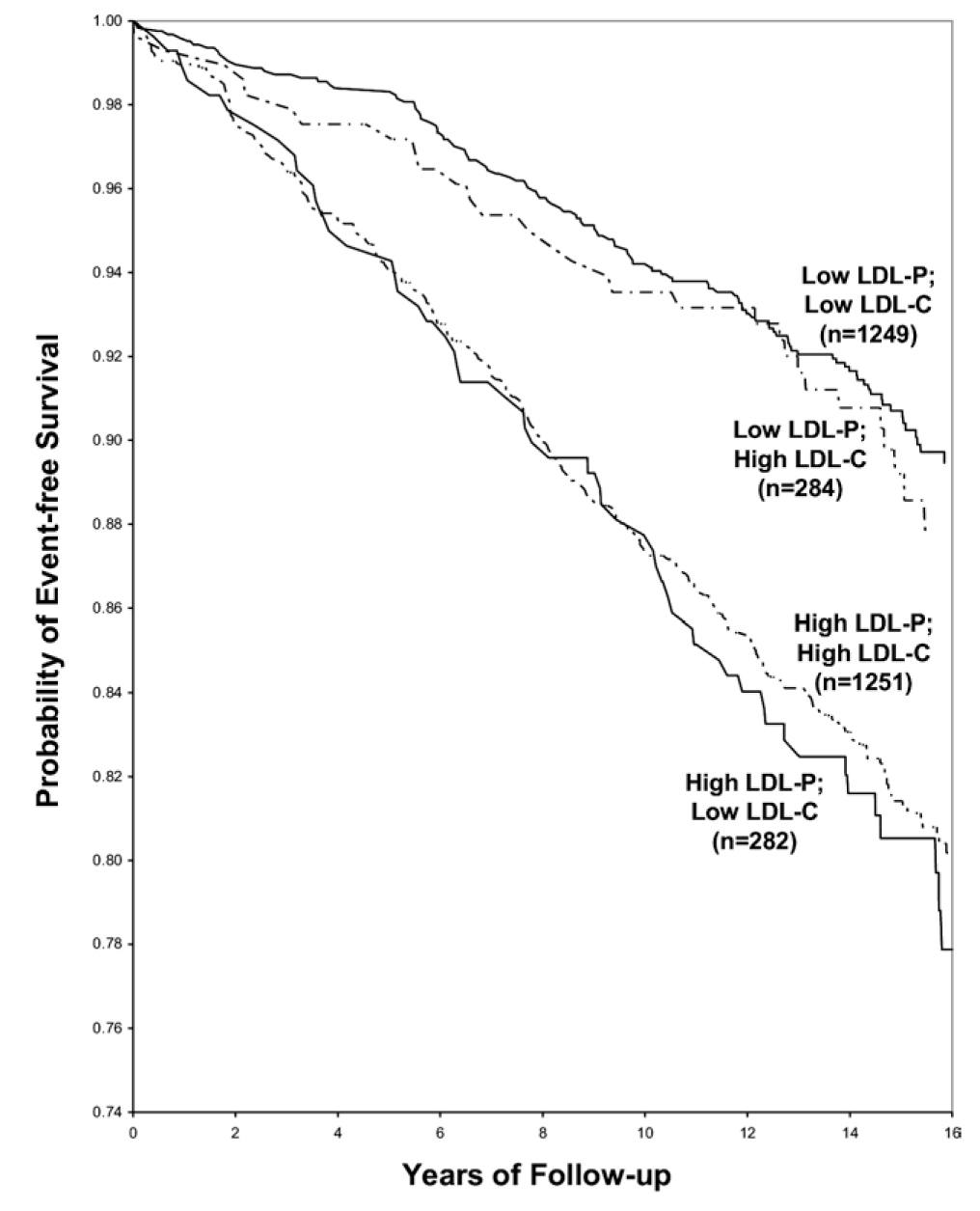
The same patterns are observed:
- LDL-P is the best predictor of adverse cardiac events.
- LDL-C is only a good predictor of adverse cardiac events when it is concordant with LDL-P; otherwise it is a poor predictor of risk.
Amazingly the persons with the worst survival had low (below median) LDL-C but high LDL-P. The patients most likely to have high LDL-P with unremarkable or low LDL-C are those with either small LDL particles, or TG-rich / cholesterol poor LDL particles, or both (e.g., insulin resistant patients, metabolic syndrome patients, T2DM patients). This explains why small LDL particles, while no more atherogenic on a per particle basis than large particles, are a marker for something sinister.
Populations where LDL-P and LDL-C discordance are even more prevalent
As I described above, the discordance between LDL-P and LDL-C is exacerbated in patients with metabolic syndrome. The figure below, MESA data, again borrowed from Jim Otvos, presents this difference in an elegant way. The horizontal axes show LDL-P concentration in the usual units, nmol/L.
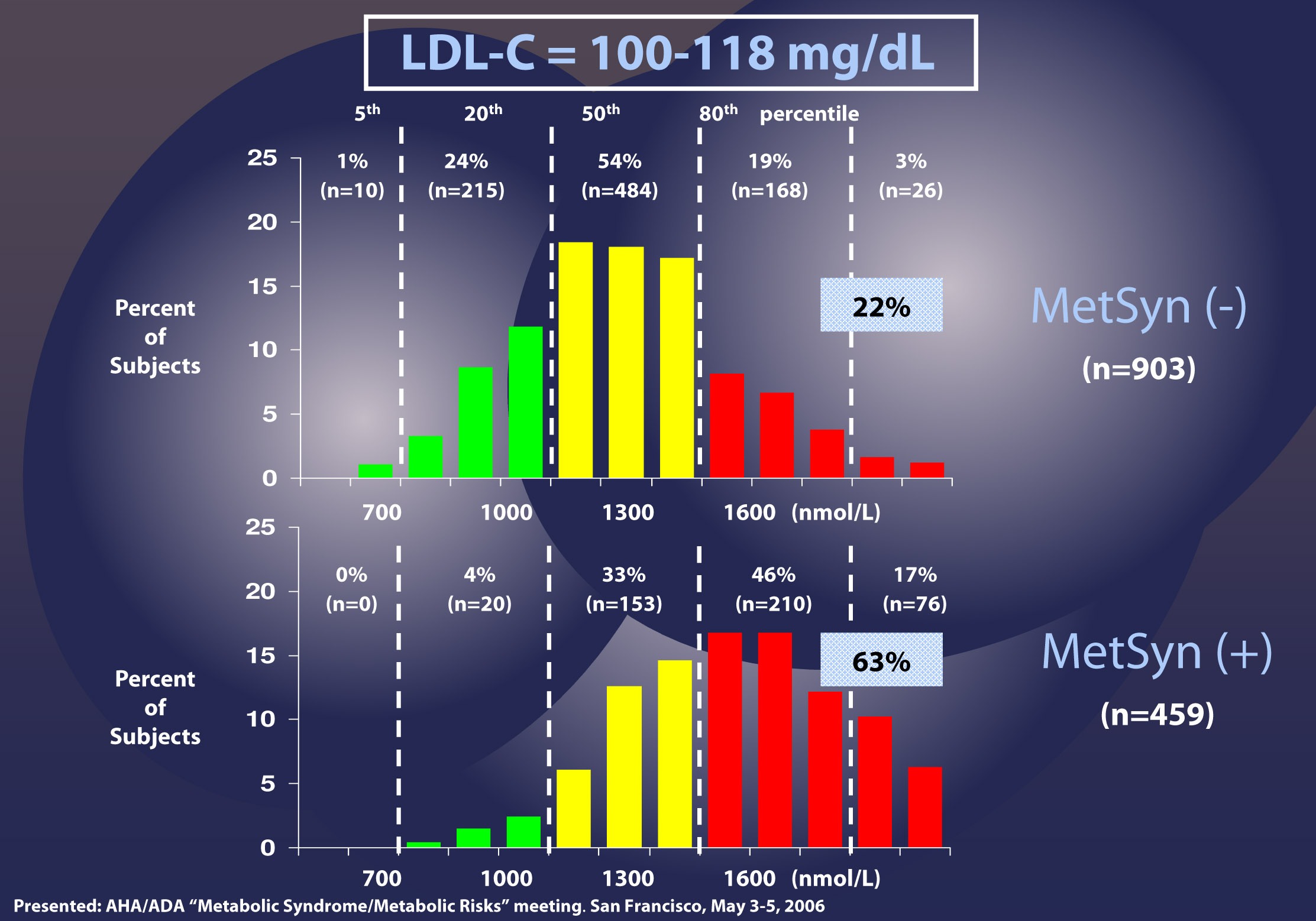
Patients with LDL-C between 100 and 118 mg/dL (i.e., second quartile of risk: 25th to 50th percentile) are shown without metabolic syndrome (top) and with metabolic syndrome (bottom). In the patients without metabolic syndrome, LDL-C under-predicts cardiac risk 22% of the time, consistent with the population data I have shown you earlier. However, when you look at the patients with metabolic syndrome, you can see that 63% of the time their risk of cardiac disease is under-predicted. Again, not a typo.
There are so many subsets and cut-off points that I could devote ten more posts to showing you every one of these analyses. Let me finish this point with the most recent, hot-off-the-press (actually, still in press in the American Journal of Cardiology, though you can get a preprint here) analysis of which Tom Dayspring is one of the authors.
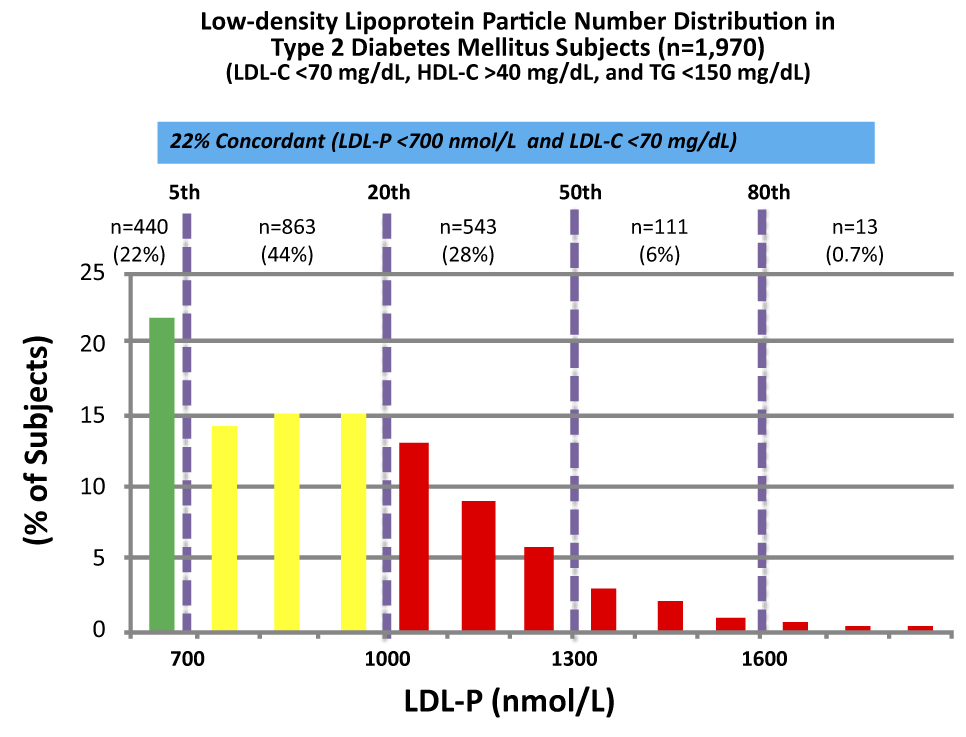
These data were collected from nearly 2,000 patients with diabetes who presented with “perfect” standard cholesterol numbers: LDL-C < 70 mg/dL; HDL-C > 40 mg/dL; TG <150 mg/dL. However, only in 22% of cases were their LDL-P concordant with LDL-C. That is, in only 22% of cases did these patients have an LDL-P level below 700 nmol/L.
Remember, LDL-C < 70 mg/dL is considered VERY low risk – the 5th percentile. Yet, by LDL-P, the real marker of risk, 35% of these patients had more than 1,000 nmol/L and 7% were high risk. When you do this analysis with the same group of patients stratified by less stringent LDL-C criteria (e.g., <100 mg/dL) the number of patients in the high risk group is even higher.
The real world tragedy: 90-95% of physicians, including cardiologists, would bet their own lives that persons with an LDL-C < 70 mg/dL have no atherosclerotic risk.
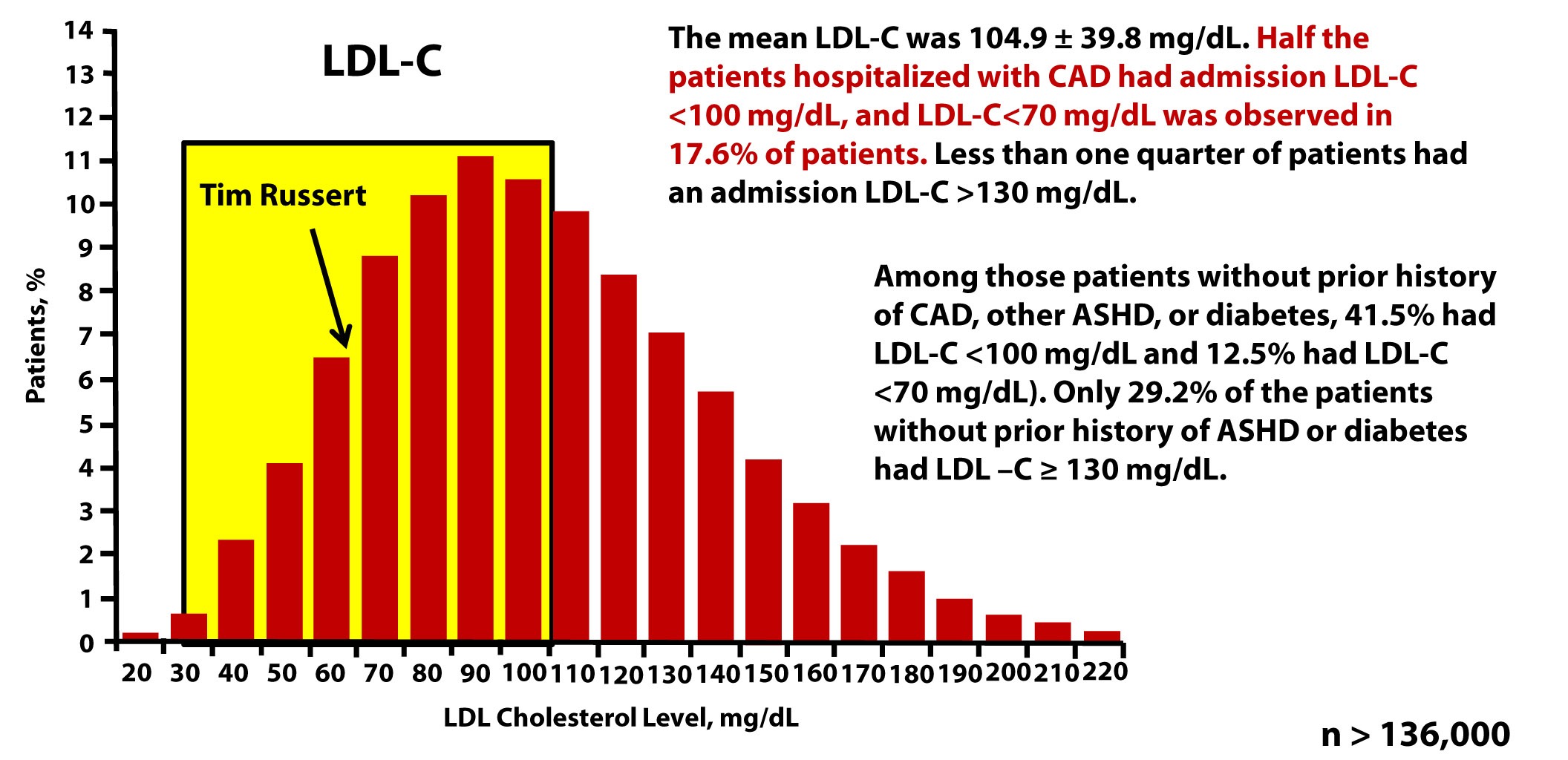
Tim Russert, shortly before his death, had his LDL-C level checked. It was less than 70 mg/dL. Sadly, his doctors didn’t realize they should also have been checking his LDL-P or apoB. The figure below, which is from one of Tom Dayspring’s presentations, shows data from this study of nearly 137,000 patients hospitalized for coronary artery disease between 2000 and 2006. As you can see, LDL-C fails to even reasonably predict cardiovascular disease in a patient population sick enough to show up in the hospital with chest pain or outright myocardial infarction.
Why are LDL-C and LDL-P so often discordant?
Think back to what you learned in a previous post in this series. LDL particles traffic not only cholesterol ester but also triglycerides. Each and every LDL particle has a variable number of cholesterol molecules which, because of constant particle remodeling, is constantly changing. In other words, of the several quadrillion LDL particles floating in your plasma, no two are carrying the exact same number of cholesterol molecules. It takes many more cholesterol-depleted LDL particles than cholesterol-rich LDL particles to traffic a given cholesterol mass (i.e., number of cholesterol molecules) per volume of plasma (i.e., per dL). Core cholesterol mass is related to both LDL particle size (the volume of a sphere is a third power of the radius — it can take 40-70% more small particles than large LDL particles to traffic a given cholesterol mass) and the number of TG molecules per LDL particle.
TG molecules are larger than cholesterol ester molecules, so as the number of TG molecules per particle increases, the number of cholesterol molecules will be less – in a very non-linear manner. Regardless of size it takes many more TG-rich LDL particles (which are necessarily cholesterol-depleted) to traffic a given cholesterol mass than TG-poor LDL particles. The persons with the highest LDL particles typically (though not always) have small LDL particles that are TG-rich. These are incredibly cholesterol-depleted LDL particles.
Summary
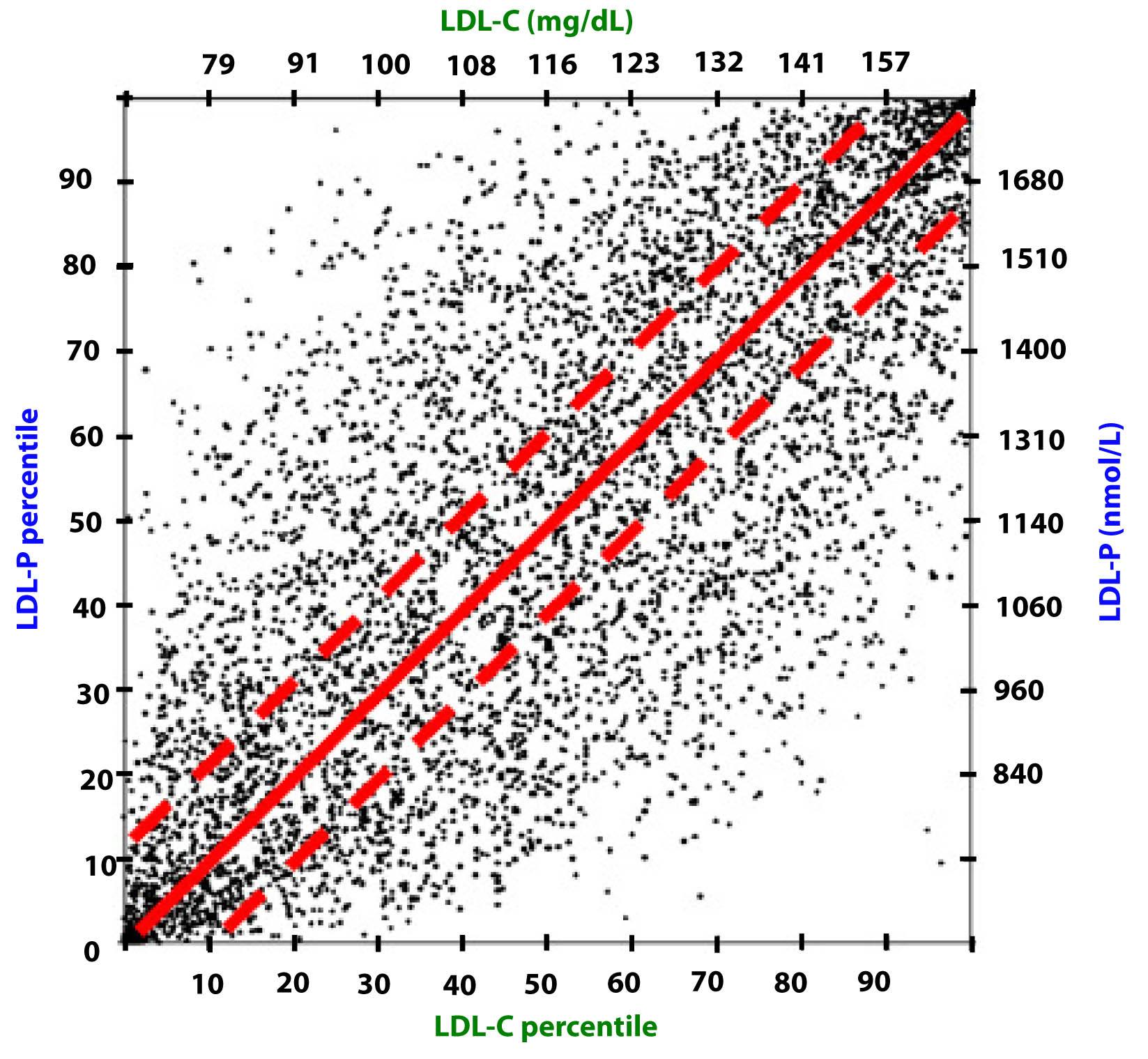
Take a look at this figure below from the 2011 Otvos et al. paper I referenced above. It’s a scatterplot of each data point (i.e., patient) in the study. The solid red line shows perfect concordance between LDL-P and LDL-C. The dashed red lines show a +/- 12% margin on each side. Look at how many dots (remember: each dot represents a person) lie OUTSIDE of the dashed red lines. Now look again.
When people argue with me about why it’s unnecessary to check LDL-P or apoB because it’s much easier and cheaper to check LDL-C, I like to remind them of what Clint Eastwood would probably say in such a situation: “You’ve got to ask yourself one question: Do I feel lucky? Well, do ya, punk?”
- With respect to laboratory medicine, two markers that have a high correlation with a given outcome are concordant – they equally predict the same outcome. However, when the two tests do not correlate with each other they are said to be discordant.
- LDL-P (or apoB) is the best predictor of adverse cardiac events, which has been documented repeatedly in every major cardiovascular risk study.
- LDL-C is only a good predictor of adverse cardiac events when it is concordant with LDL-P; otherwise it is a poor predictor of risk.
- There is no way of determining which individual patient may have discordant LDL-C and LDL-P without measuring both markers.
- Discordance between LDL-C and LDL-P is even greater in populations with metabolic syndrome, including patients with diabetes. Given the ubiquity of these conditions in the U.S. population, and the special risk such patients carry for cardiovascular disease, it is difficult to justify use of LDL-C, HDL-C, and TG alone for risk stratification in all but the most select patients.
- This raises the question: if indeed LDL-P is always as good and in most cases better than LDL-C at predicting cardiovascular risk, why do we continue to measure (or calculate) LDL-C at all?
Photo by Aldric RIVAT on Unsplash





Peter:
Off the subject at hand but have you done any research or reading on the use of heart scans for calcium scoring?
I have not personally done so, though I’m familiar with them and had one at the age of 36, which was enough to convince me I needed to change what I was doing…I was in the 92nd percentile of risk despite doing everything “right.”
I wonder if anyone has had a coronary angiogram after several years to see if there is any change in atherosclerosis.
Would looking at the calcification levels of the plaques also be a less invasive test?
Here’s a summation of your work:
Concordance:
Normal TC or Normal LDL-C
Normal LDL-P
Positive discordance:
High TC or High LDL-C
Normal LDL-P
Negative discordance:
Normal TC or Normal LDL-C
High LDL-P
Unknown-cordance:
Normal TC or Normal LDL-C
Unknown LDL-P
Standard Lipid Panel: $60
NMR Lipoprofile: $90
Worth additional $30 to find out your risk level?
Concordance would also include high LDL-C and high LDL-P. Obviously, I think the extra $30 is worth knowing my LDL-P, but we haven’t quite got to where I’ve “armed” everyone with enough info to make their own personal decision.
wow,could it be true ketosis changes standard risk factors?BTW as an ApoE 2/3 I,too, have the high LDL and LDL-p (ApoB)with low carb and ketosis.so it is not just an ApoE 4 phenomenon.low carb is necessary for blood sugar and triglyceride contro,but the LDL-p is a problem.looking forward to you addressing this issue.
Don’t expect a resolution, however. We are now in the world of hypothesis generation, not assertion.
Did the Massai or Inuit supplement their lifetime of ketosis with sodium and magnesium? Off topic but I kept forgetting to ask until now.
Sodium definitely (either through the blood of their prey and/or salt water). Magnesium, may have come in sufficient quantities from the meat/blood of the meal.
“Did the Massai or Inuit supplement their lifetime of ketosis with sodium and magnesium? ”
Yes. The Inuit made soup using the clean top edge of the sea ice, which is obviously salty, but not as salty as the water. Incredibly, they hunt mussels under the ice, and make mussel soup with melted sea ice: https://www.bbc.co.uk/news/science-environment-12241053
The majority of the magnesium in their diet comes from eating lots of kelp, which they also add to the soup. Kelp is actually quite mineral rich. As for Vit. C, they got theirs from seal brains and caribou liver.
The Masai actually do eat leafy greens, which are high in minerals, esp. magnesium. Spinach-like foods have lots of magnesium.
There is some change on the traditional lipid hypothesis;
Eminent doctor says it is time for a full reappraisal of the cholesterol theory
https://healthydietsandscience.blogspot.com/2012/06/eminent-doctor-says-it-is-time-for-full.html
Also more on a contrarian cholesterol view;
https://healthydietsandscience.blogspot.com/search/label/Cholesterol%20and%20Heart%20Disease
Peter: If you had a calcium scan at age 36, and changed your dietary regimen based upon your risk at 92% level, how would you know your program(if you are taking meds along with your restricted carb diet) that your risk is not worsening, improving or remaining stable. Sounds like you would have had a high calcium score for 92% risk.
It is one thing to lower our LDL-P, but how do we actually know what we are doing is working which is ultimately staying event free? You may get particle count to under 1000, but maybe for any given person’s risk profile it needs to be closer to 400, if possible.
Thanks
Also, how influenced is NMR test by what you have most recently eaten, say in the last few days or weeks?
My score was only 6, but at the age of the 36 that was, obviously, high. Basically, at 36 one shouldn’t have ANY calcium in their artery walls. So “clinically” this was of no value, but it was predicative of something. NMR seems largely insensitive to recent meals/fed state.
OK, so LDL-C alone is not a good predictor of risk. But if LDL-P increases because triglycerides increase, wouldn’t looking at LDL-C together with TG be a good predictor of risk? What’s the concordance between LDL-P and TG?
Not saying that people shouldn’t get their LDL-P number but it seems that a lot of people are reluctant to do this without their doctor’s cooperation which is not always forthcoming.
Life Extension you can order this on your own
for 90 bucks
“a lot of people are reluctant to do this without their doctor’s cooperation” Not to be flip but
adios amigo
(or don’t tell them if you can’t hire your physician)
I’ll leave the country before I beg for cooperation…who wants all this in the mothership data base anyway? There is a lot to be said for keeping your labs private, imo
A couple of questions:
1. If we’re discussing the possibility that LDL particle number may not be as clear a risk factor in individuals who are in ketosis, isn’t that basically saying that we’re considering the possibility that LDL particle concentration ISN’T the one true 1st order factor influencing CVD?
2. Peter, I’m wondering if at some point you plan to discuss the issue of post-prandial serum triglycerides, and whether those are a more useful way to assess risk than are fasting triglycerides, and if so, what that might imply for folks eating a high-fat diet.
3. My impression has been that the correlation of LDL-C with heart disease risk has generally been weaker in women than men- and that in women (of a certain age, at least) all-cause mortality is actually lower when LDL-C is above the range considered officially desirable. Are the results with LDL-P for women still different from those for men, or do findings for men and women converge more with LDL-P than LDL-C? Which studies could I look at that actually include LDL-P and women?
Thanks!
1. I think this hypotheis, that LDL-P may be less important is ketosis, or other LC state is VERY preliminary. That said, if it were shown to be true, it COULD imply that LDL-P is less important that believed in anyone, but for me even suggest that would be irresponsible beyond words.
2. The gold standard is TG AUC (area under curve). Since that’s not a practical test for most folks, myself included, it’s easier to standardize the test in a fasting state. That does mean this is a “better” test, just easier to compare.
3. This is a great question for Tom Dayspring, who actually sub- sub- sub-specializes in this. I’ll defer to Tom for a more robust response.
Hi Peter & Laura:
I think Laura’s 3 is true for women with periods. Google shows quite a few studies suggesting estrogen protects the endothelium somehow. But post menopause risk seems to rise to that of men.
Hi, thanks Peter and HighlySkeptical,
I’m still rather uncertain about serum cholesterol values as they relate to mortality in women, elderly or otherwise. I know one can find a study to support almost any hypothesis, but there have been a number of studies coming out of Scandinavia lately that call some of the CW into question for me. Several specifically on the elderly in Finland, and a big one one from Norway, with abstract pasted in below (the article appears to be freely available). Of course, generally LDL-P is not reported in these studies, but I don’t know that that makes them completely useless.
J Eval Clin Pract. 2012 Feb;18(1):159-68. doi: 10.1111/j.1365-2753.2011.01767.x. Epub 2011 Sep 25.
Is the use of cholesterol in mortality risk algorithms in clinical guidelines valid? Ten years prospective data from the Norwegian HUNT 2 study.
Petursson H, Sigurdsson JA, Bengtsson C, Nilsen TI, Getz L.
Source
Research Unit of General Practice, Department of Public Health and General Practice, Norwegian University of Science and Technology (NTNU), Trondheim, Norway. [email protected]
Abstract
RATIONALE, AIMS AND OBJECTIVES:
Many clinical guidelines for cardiovascular disease (CVD) prevention contain risk estimation charts/calculators. These have shown a tendency to overestimate risk, which indicates that there might be theoretical flaws in the algorithms. Total cholesterol is a frequently used variable in the risk estimates. Some studies indicate that the predictive properties of cholesterol might not be as straightforward as widely assumed. Our aim was to document the strength and validity of total cholesterol as a risk factor for mortality in a well-defined, general Norwegian population without known CVD at baseline.
METHODS:
We assessed the association of total serum cholesterol with total mortality, as well as mortality from CVD and ischaemic heart disease (IHD), using Cox proportional hazard models. The study population comprises 52 087 Norwegians, aged 20-74, who participated in the Nord-Trøndelag Health Study (HUNT 2, 1995-1997) and were followed-up on cause-specific mortality for 10 years (510 297 person-years in total).
RESULTS:
Among women, cholesterol had an inverse association with all-cause mortality [hazard ratio (HR): 0.94; 95% confidence interval (CI): 0.89-0.99 per 1.0 mmol L(-1) increase] as well as CVD mortality (HR: 0.97; 95% CI: 0.88-1.07). The association with IHD mortality (HR: 1.07; 95% CI: 0.92-1.24) was not linear but seemed to follow a ‘U-shaped’ curve, with the highest mortality <5.0 and ?7.0 mmol L(-1) . Among men, the association of cholesterol with mortality from CVD (HR: 1.06; 95% CI: 0.98-1.15) and in total (HR: 0.98; 95% CI: 0.93-1.03) followed a 'U-shaped' pattern.
CONCLUSION:
Our study provides an updated epidemiological indication of possible errors in the CVD risk algorithms of many clinical guidelines. If our findings are generalizable, clinical and public health recommendations regarding the 'dangers' of cholesterol should be revised. This is especially true for women, for whom moderately elevated cholesterol (by current standards) may prove to be not only harmless but even beneficial.
Laura, I think your point about these studies not commenting on LDL-P or apoB is the key point. In fact, most studies looking at overall mortality do not show a strong association between cholesterol levels and mortality, or even disease risk. It’s one of the reasons TC and LDL-C are not even in the criteria for metabolic syndrome. I have no doubt that what is true in men or complete both sexes (in aggregate) may not be true in women, or that what is true in pre-menopausal women, may not be true in post-menopausal women, at least to the same extent. However, the best evidence I have seen still suggests to me that there is no demographic in which high apoB or high LDL-P is not suggestive of more risk.
I am beyond fascinated with this topic and can’t thank you enough for this series. You’re testing the limits of my comprehension, but you still got me with you. I appreciate the explanations without dumbing it down to the point where you don’t show the why or how.
Very much looking forward to reading more
Hello Dr. Attia –
great work! Looking forward to your discussion of Treatments.
I started eating low-carb in 2010 after reading Dr. Cynthia Kenyon’s research work on life-extension by reducing insulin production. I am hoping that there will be an ‘Generalized’ solution that ties her research findings and Cardio Vascular health methods.
Indy M.
Well, Doc, game on!
Having been obese for quite a while (30 years), and having been diagnosed with a congential cardiac defect (hypertrophic cardiomyophathy) a half dozen years ago, I’ve gone highly LCHF and it has been a great improvement for me. I’ve lost 25 pounds, lost my interest/obsession with food, lost my ADHD, and am operating at an improved mental capacity, and my negative physical symptoms have diminished, so I’m a big “buyer” of the concept.
Today I “had it out” with my cardiologist, who prescribed statins for my elevated triglicerides, which occurred after I started an LCHF diet. I pointed him, and his second in command, to your website. We’ll see what happens. As I left, the second in command was quite intrigued by what she was reading. I would like to point out that my doctor has “written the book” on my particular condition and in his field is probably the best there is, but I personally don’t think that makes him qualified to be an expert on blood lipids.
As I pointed out to him, we both have my longevity as a common interest, and I’d be happy to take whatever test he’d prescribe to either convince me that I have incipient CAD, or not, but I wasn’t going to let one blood lipid test determine whether I’d be taking statins or not – he wants me on them, and I don’t generally believe in conventional wisdom. So we agreed I’d get a coronary calcium scan done first.
I hate to disagree with my doc, who is so well intentioned and for whom I have great respect. But I’d like to avoid medications with their unknown effects. Whats the best way to get these alternative data points? NMR? It would be useful to get a “laundry list” of tests.
I’m going to push this as far as I can with my doc. I have no desire to go back to the old me. We could take this off-line if you’d like. It could be useful. Thanks.
Hi Peter,
First time ever posting, so bear with me. I love your site – it has changed my life. I hope too that it might actually save my mom’s. I turned her on to it, and she loves you!
I read all 6 parts of this so far, and I am just floored. Such good info. I have been eating like you for about 6 or 7 weeks (the sautéed ground beef is my absolute fave!). Weight loss is slow, but everything else is great, so I don’t care as much. However, a friend and I were thinking maybe I am really really insulin resistant. About time to check my blood work and see where I am (horrible numbers about 6 months ago). So I asked my doctor about NMR and the HOMA-IR. He SHUT ME DOWN. It was awful. I have a great relationship with this doctor and I was horrified. I fought for the NMR and won, but he wouldn’t even discuss the HOMA-IR. He said he would have to justify it (The ADA goes by sugar level only) and the results don’t matter – the treatment would be the same. So, my question is: Do you think it’s worth it to try to educate your doctor (do you have any advice if so), or just say screw it and go find a new doctor? I apologize if you have covered this previously. I did look, but I am too angry to keep searching.
Thanks and keep on doing your thing – can’t wait to see more!
Your doctor agreed to the NMR, but not the $3 fasting insulin level (HOMA-IR is calculated with fasting insulin and fasting glucose)? Wow! See what the NMR and fasting glucose and TG show. Best way to triangulate in IR is: HOMA-IR, TG/HDL-C, and LP-IR score (which you will get from Liposcience NMR). Just make sure your doctor also requests that with the NMR data.
Peter,
Very much like the scatterplot of LDL-C vs LDL-P in the Summary. Is it possible to add one more variable to the plot, a variable like cardiovascular risk, or cardiovascular death, or total death — showing the variable with a spectrum of colors (e.g. darkest red for worst quintile, lightest red for best quintile)? The image would be really interesting to see, especially if the color gradient was primarily from the bottom of the plot to the top of the plot. Incidentally, what is the plot’s correlation?
I don’t recall and would need to go back and look. I like the idea of the adding more info to this.
Peter,
I finally got around to ordering an online NMR LipidProfile via Life Extensions, and was loving the series till I just got my results back, so I have a feeling that there is a lot more to talk about in the series. (Posting results for info, not advice)
LDL-P : 1932
LDL-C : 157
HDL-C : 56
Trig : 78
TC : 229
HDL-P : 30.0
Small LDL-P: 618
LDL Size : 21.4
LP-IR Score: 13 (I was very happy about this despite not knowing how it’s calculated)
I find these results very concerning just looking at my LDL-P, I’m 28 years old, 6′ 2″ I have been fluctuating between 175-185 pounds (by choice) for almost 12 months now, I eat Ketosis diet for about 2/3 a month, and low carb about 2/9 a month and eat crap about 1/9 a month.
I feel extremely healthy, and would never have expected my LDL-P to be 1932.
So to my question, if high LDL-P is very bad to have when on the high carb diet, why is it not bad when on a low carb diet…?
If both situations are bad, do carbs need a sweet spot of ingestion at 50/100/200g etc to prevent LDL-P rising and inducing plague in the artery walls.
If high LDL-P while in ketosis is still safe, then what about the high carb diet is modifying the artery wall composition to allow LDL-P inside it (or not letting it out), or worse yet what is ketosis generating that may protect against artery wall penetration/extraction? Worse because that means people that occasionally do a 1 day carb binge may in fact be doing the most damage to their arteries than any other person.
Also keep up the good work, I feel my mind growing every week, and it starts with your blog post in the morning.
The best way to find out what your LDL-P would be on a standard diet would be to return to it for a period, say, 3 months, and re-check.
The biggest problem we fact in interpreting data like this in a dietary state different from the dietary state people were in when the studies were done, which is a significant differences, is that we don’t know what other factors may be at play.
Thanks Peter,
My plan of attack after taking some time to think about it is going to be to go even more strict and do ketosis for 3 months straight, get a follow up NMR, that way i know the direction in which my LDL-P is trending, if it trends further up, then i’m going to see what happens when I diet for 3 months on 200g of carbs a day, then get a follow up NMR. And if it is trending down, then I know I was just in a extremely bad place to start with haha. I’ll try to keep coming back to this specific comment with the updates.
Let me know if there are any more data points I should collect now, before I start the experiment, that maybe of value/interest at the end of the 6 months.
Ask you doc to get the “full panel” from Health Diagnostics Labs, Inc. (HDL, Inc.). I’m going to run through some case studies and give folks a sense of what kind of testing is actually out there.
So 6 months later I got my follow up NMR Lipid Profile test, I couldn’t bring myself to go back to eating carbs again, and I just feel so good eating a ketogenic lifestyle that I decided to simply keep to it. Here are the updated results:
LDL-P : 2130
LDL-C : 175
HDL-C : 54
Trig : 52
TC : 239
HDL-P : 28.5
Small LDL-P: 672
LDL Size : 21.4
LP-IR Score: 21
Most noticeably for me, LDL-P continued to rise, triglycerides did plummit while keeping HDL-C stable. Weight wise I was stable during the entire 6 month period, 6′ 2″, 180 pounds, no belly, no six pack either lol.
I have been genotyped by 23 and me a few years ago, so if there are any traits anyone would like to know for understanding high LDL-P then let me know.
This test has made me pause and think for a while, haven’t come to an answer, more research is in store for me, but I think i’m going to be focusing on what I can do to lower that LDL-P, whilst it may not be an issue if I don’t generate any inflammation, I still feel like that is saying don’t worry if you never eat carbs again you’ll be fine, whilst it may be true, its still not the stable place I was in when I was 16. Until I can normalise to that level, I’ll always want to tweak what I’m doing.
Peter,
I want to thank you for this amazing resource. I have to admit that I haven’t fully internalized all of it yet, on my third read-through. Very dense, but I will keep at it. My question has to do with how statins and ldl-p interact. I have been on omega-3’s and statins for many years for high cholesterol and triglycerides triggered after an organ transplant (on cyclosporin as well), and although my numbers are much better, they are still high. We have NEVER done a NMR lipid profile. I would like to get a profile, but would it make any sense to do it with or without the statin on board for 6-8 weeks? You’ve discussed it some, but it’s unclear to me how meaningful the test would be as is. I had mostly normal cholesterol before transplant and cyclosporin, so I suspect I won the transplant lottery and lost the genetics lottery in regards to how cyclosporin affects my endogenous cholesterol production. I tolerate statins well, so it’s not an issue of needing to drop it.
Thanks.
LDL-P concentration is primarily a function of 3 things: how much cholesterol is produced by your body; how much cholesterol is re-absorbed in your guy (from your bile); how many LDL particles are cleared by your liver. Statins primarily work on the first and third of these. Check under your “normal” conditions (i.e., if you’re on a statin, you might as well how it’s doing).
I got my NMR LipoProfile results after strict very low carb for about 5 months (less than 25 grams). I also eat high fat and moderate protein. Maybe I skimped on the calories and messed up some hormones but I’ve been fairly weight stable for a month (losing only about 2-3 pounds maybe) and was at 12.2% body fat when I took the test. The numbers were all great, except for LDL-P. Any idea what might be going on? I’ve been doing some reading and people are suggesting thyroid issues. I’ve started supplementing vitamins and minerals and increasing my calories and increasing exercise since then. But I’m afraid with numbers this high (just in LDL) that I may have some other underlying issues. If it was lipids being poured into my blood from weight loss alone, wouldn’t I see higher triglyceride numbers as well? I’m afraid that even with supplementation and changing things up, I won’t get anywhere within a “normal” range. I won’t even hit average until I drop about 1500 particles.
(Yes, that does say over three thousand LDL-P down there)
LDL-P 3132 (>2000 is highest risk)
LCL-C 323 (>189 highest risk but not concerned about this number)
HDL-C 63 (This is really good >40)
Trig 62 (Also very good 30.5. Don’t know much about HDL-P though)
Small LDL 217 (average is 20.5 for large pattern A)
Insulin Resistance
Large VLDL-P 0.9 (Very good. 7.3 is highest percentile in favor of sensitivity so this is good)
VLDL Size Unknown – “VLDL concentration too low to allow determination of VLDL Size. Low VLDL concentration contributes minimally to the LP-IR score.”
LDL Size 21.7 (>21.2 best percentile)
HDL Size 9.2 (50th percentile)
LP-IR Score 15 (best score is less than 27, worst is over 63 – so this is excellent)
I requested thyroid free t3/t4 and reverse T3 and my doctor refused to do those tests and instead just tested TSH and Free T4. Which he said were within range. So unless I pay for another test out of pocket, I won’t really know if it is perhaps T3. And even if I did, I haven’t found a good way to interpret what healthy/helpful levels are.
Derek, I just can’t imagine an abnormal rT3 (or T3) having this impact on your LDL-P. I don’t know what your LDL-P was on a “standard” diet, but obviously this current level deserves a further work-up (e.g., apoE genotyping, sterol analysis). Please follow up with your physician. In the absence of better data to the contrary, I think we should assume you are at risk.
NOTE TO READERS: I’m commenting specifically to Derek, but this advice holds to EVERYONE who is sending me elevated LDL-P numbers.
This is one of the things that concerns me about the idea of monitoring and treating LDL-P, with powerful drugs if necessary. We know that a significant percentage of people who adopt LCHF diets spike their LDL-C, sometimes dramatically. And now with more people getting NMR tests we know that at least some, and perhaps many, of them also wind up with high LDL-P (in fact, some of us get LDL-C so high that it’s hard to believe our LDL-P could be optimal no matter how big and cholesterol-dense our LDL particles are). Peter from Hyperlipid has said this of himself, and it applies to me, too.
So we have a dietary change that seems incredibly healthy, with many people completely recovering from metabolic syndrome and other ills, including obesity. Yet their LDL-C, and apparently also LDL-P, may spike. Does it make sense that this is a sign of ill health or risk in the context of everything else dramatically improving? I believe this is why Dr. Eric Westman has said that he’s begun to think that spiked LDL-C on LCHF may be a sign of vibrant health, rather than risk. I don’t know if Dr. Westman has addressed spiked LDL-P as well.
If in fact high LDL-P in the LCHF context is healthy that would suggest it is a marker, rather than a major causal factor, in CVD, a marker that only applies in some contexts. Or maybe a minority of people, with specific genetic variations, are really putting themselves at risk with high saturated fat LCHF? (I don’t like that thought, since I’d likely be one of them.) I’m not clear that current research has disambiguated these possibilities.
I know that Peter, and others, acknowledge that the research implicating LDL-P has been done on people eating SAD and may or may not apply to those eating LCHF. I appreciate that LDL-P seems to be a much better “risk factor” than standard measures, but I can’t help wondering if the science is still too preliminary to justify taking powerful pharmaceuticals (or even reducing saturated fat?), at least for those of us on LCHF. Obviously, this is an individual decision that has to be made with imperfect information, like so many in life. Since my default position is to avoid medical intervention in the absence of pretty convincing evidence of net benefit, I’m not yet sure if I even want to get the NMR test. But maybe by the end of this series I’ll be convinced!
Perhaps this is an area where NuSi will be able to promote the needed research.
Thanks again for the excellent and thought-provoking series.
Bill, Eric Westman and I had breakfast last week in DC and discussed this exact topic at length. I *wish* I had an answer or *knew* what was right, but I don’t. This is one of those areas that really warrants each of us making a personal choice with the best data available, however applicable it may or may not be. What I’m hoping to do is provide readers with the current state of knowledge so they might be able to make the most informed decisions possible, but I’m am fully aware of the challenges these seemingly conflicting data provide.
Thanks, Peter.
It will be interesting to see whether more docs successfully using LCHF, such as Dr. Westman, will start following LDL-P routinely, and if so what they will recommend. I’ll wait until you complete your series before giving my own doc another headache about this.
And most importantly, if we can develop some long-term studies to actually determine the predictive power of LDL-P/apoB in LCHF/ketotic persons.
It would be interesting to me if Specialty Health (the firefighters in AZ) would be able to do an analysis of their population on the LDL-P to see what percentage of their population who switches to carb restriction gets this increase in LDL-P with all other markers going in the right direction. It seems like they’re serving a large population and it also seems like everybody is getting an NMR. Looking back over existing data like theirs, and seeing if there are trends, could provide an insight that could lead to a testable hypothesis.
It would also be great if Drs. Westman, Volek and Phinney could start to look at this, by including the NMR in their lipid analyses of their patients/subjects.
@Derek, ketosis significantly skewed my thyroid labs (which I”ve been doing regularly for a very long time). My TSH, which has been nailed to the floor at 1.85 for years is now .0016 (!!). My free T3/free T4 which always ran a bit on the low end of normal are now above optimal, and I’m converting a lot into rT3, which is now at the highest end of normal. My antibodies are okay. One of at least three things could account for this: 1) I no longer need the same amount (or any) thyroid med. I have backed way down and will retest in a few weeks 2) I have very early Hashi’s 3) ketosis screws up normal test results. There’s some discussion in the literature that, in a nutshell, dietary carbohydrate is thyroid hormone intensive; i.e., requires thyroid hormone to metabolize. This could be another example of lab “normals” being based on western diets. So I’m just sayin’ that I’m not sure that getting your thyroid tested will get you answers. Having said that, if your thyroid is an issue, I have never known or read of a thyroid patient who didn’t have lots of symptoms in addition to an abnormal lipid result. Thyroid imbalance is very heavy on the symptoms, so if you don’t have any, a bad lipid finding by itself wouldn’t be a strong sign to me of an underlying thyroid issue.
Yes, I would like to see this, too.
I appreciate this is new research but I’d be very interested in hearing Peter’s reaction to it and also the response of other contributors here.
The real culprit behind hardened arteries? Stem cells, says landmark study
Differentiation of multipotent vascular stem cells contributes to vascular diseases.
However it’s a sad reflection on modern medicine that the emphasis is on the development of new treatments rather than improving our ability to prevent vascular disease.
“If your target is wrong, then your treatment can’t be very effective,” said Dr. Shu Chien, “These new findings give us the right target and should speed up the discovery of novel treatments for vascular diseases.”
It’s not clear to me how this information changes the problem statement or remedy any time soon. Perhaps, some time in the future, this insight (assuming it’s correct) will offer alternative treatments.
Peter,
This site is a treasure for me; I am on a ketogenic diet for 2 months, after a break of 10 years for main stream diets. If a site like this would have existed then, I guess I was still on this diet. I am also an ultramarathoner, training for my first 100 mile on a ketogenic diet. So this site is perfect for me. Thank you very much Peter.
Quick question on this post, LDL-C today is still considered as a risk predictor, and medicines are given to reduce the LDL-C level. If we know now that LDL-C is meaningless, what does it say on the medicine?
It’s not that LDL-C is meaningless, it’s just that 30-50% of the time it’s not in line with the actual driver of risk, LDL-P. If all patients were treated based on LDL-C some good would (and is) done. The point is, we should sharpen our pencils, so to speak, and be sure patients are being treated correctly.